According to the world health organization
According to the world health organization
according to the World Health Organ
according to the World Health Organisation, malaria, a disease spread by mosquitoes, affects millions of people every year. Everyone knows how irritating the noise made by a mosquito,followed by a painful reaction to its bite, can be. It is astonishing that so little is known about why mosquitoes are drawn to or driven away from people, given the level of distress and disease caused by these insects. We know that the most effective chemical for protecting people against mosquitoes is diethyltoluamide, commonly shortened to deet. Though deet works well, it has some serious drawbacks: it can damage clothes and some people are allergic to it.
Scientists know that mosquitoes find some people more attractive than others, but they do not know why this should be. They also know that people vary in their reactions to mosquito bites. One person has a painful swelling while another who is bitten by the same mosquito may hardly notice. Scientists have not discovered the reason for this, but they have carried out experiments to show that mosquitoes are attracted to, or put off by, certain smells. In the future, scientists hope to develop a smell that mosquitoes cannot resist. This could be used in a trap so that, instead of attacking people, mosquitoes would fly into the trap and be destroyed. For the time being however, we have to continue spraying ourselves with unpleasant liquids if we want to avoid getting bitten.
Theo Tổ chức Y tế Thế giới, bệnh sốt rét, một bệnh lây truyền qua muỗi, ảnh hưởng đến hàng triệu người mỗi năm. Mọi người đều biết cách kích thích các tiếng ồn được thực hiện bởi một con muỗi, theo sau là một phản ứng đau đớn để cắn của nó, có thể được. Nó là đáng ngạc nhiên rằng rất ít thông tin về lý do tại sao muỗi được rút ra để định hướng hoặc cách xa mọi người, đưa ra mức độ căng thẳng và bệnh gây ra bởi các loài côn trùng. Chúng ta biết rằng các hóa chất hiệu quả nhất để bảo vệ con người chống lại muỗi là diethyltoluamide, thường được rút ngắn xuống còn DEET. Mặc dù DEET hoạt động tốt, nó có một số hạn chế nghiêm trọng: nó có thể làm hỏng quần áo và một số người bị dị ứng với nó. Các nhà khoa học biết rằng muỗi tìm thấy một số người trở nên hấp dẫn hơn những người khác, nhưng họ không biết tại sao điều này nên được. Họ cũng biết rằng những người khác nhau về phản ứng của họ để muỗi đốt. Một người có sưng đau trong khi một người bị cắn bởi muỗi cùng khó có thể nhận thấy. Các nhà khoa học đã không phát hiện ra lý do cho điều này, nhưng họ đã tiến hành các thí nghiệm để chứng minh rằng muỗi bị thu hút, hoặc đưa ra bởi, mùi nhất định. Trong tương lai, các nhà khoa học hy vọng phát triển một mùi mà muỗi không thể cưỡng lại. Điều này có thể được sử dụng trong một cái bẫy do đó, thay vì tấn công người, muỗi sẽ bay vào cái bẫy và bị tiêu diệt. Đối Tuy nhiên thời điểm hiện tại, chúng ta phải tiếp tục phun chính mình với chất lỏng khó chịu nếu chúng ta muốn tránh bị cắn.
Health
Health is a term that refers to a combination of the absence of illness, the ability to manage stress effectively, good nutrition and physical fitness, and high quality of life.
In any organism, health can be said to be a «state of balance,» or analogous to homeostasis, and it also implies good prospects for continued survival.
A widely accepted definition is that of the World Health Organization (WHO), the United Nations body that sets standards and provides global surveillance of disease. In its constitution, the WHO states that «health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.» In more recent years, this statement has been modified to include the ability to lead a «socially and economically productive life.»
The WHO definition is not without criticism, as some argue that health cannot be defined as a state at all, but must be seen as a process of continuous adjustment to the changing demands of living and of the changing meanings we give to life. The WHO definition is therefore considered by many as an idealistic goal rather than a realistic proposition.
Beginning in the 1950s with Halbert L. Dunn, and continuing in the 1970s with Donald B. Ardell, John Travis, Robert Allen and others, optimal health was given a broader, more inclusive interpretation called «wellness.»
Health is often monitored and sometimes maintained through the science of medicine, but can also be improved by individual health and wellness efforts, such as physical fitness, good nutrition, stress management, and good human relationships. Personal and social responsibility (those with means helping those without means) are fundamental contributors to maintenance of good health. (See health maintenance below).
Contents
In addition to the focus on individual choices and lifestyles related to health, other key areas of health include environmental health, mental health, population health, and public health.
Wellness
According to Dr. Donald B. Ardell, author of the best seller “High Level Wellness: An Alternative To Doctors, Drugs and Disease” (1986) and publisher of the Ardell Wellness Report, “wellness is first and foremost a choice to assume responsibility for the quality of your life. It begins with a conscious decision to shape a healthy lifestyle. Wellness is a mindset, a predisposition to adopt a series of key principles in varied life areas that lead to high levels of well-being and life satisfaction.”
Many wellness promoters like Ardell see wellness as a philosophy that embraces many principles for good health. The areas most closely affected by one’s wellness commitments include self-responsibility, exercise and fitness, nutrition, stress management, critical thinking, meaning and purpose or spirituality, emotional intelligence, humor and play, and effective relationships.
Health maintenance
Physical fitness, healthy eating, stress management, a healthy environment, enjoyable work, and good human relationship skills are examples of steps to improve one’s health and wellness.
Physical fitness has been shown to reduce the risk of dying prematurely, developing heart disease, diabetes, high blood pressure, and colon cancer. It has also been shown to reduce feelings of anxiety and depression, control weight, and help improve overall psychological well-being.
Healthy eating has been linked to the prevention and treatment of many diseases, especially cancer, heart disease, hypoglycemia, and diabetes. Overall, people with healthy eating habits feel better, keep up strength and energy, manage weight, tolerate treatment-related side effects, decrease the risk of infection, and heal and recover more quickly. Studies have also shown a correlation between persons with a hypoglycemia and crime. For persons with adult onset diabetes, in some cases healthy eating can reduce or eliminate the need for insulin.
Researchers have long known that stress management can help people reduce tension, anxiety, and depression, as well as help people cope with life challenges more effectively. Stress management can also assist persons in having more satisfying human relationships, job satisfaction and a sense of life purpose. Duke University Medical Center researchers have recently found that stress may also provide cardiovascular health as well.
A good environment that has clean and safe drinking water, clean air, is relatively free of toxic elements, and not overcrowded, can increase life expectancy significantly. Environmental Health is becoming an increasingly important consideration for causes of premature death.
Wellness workplace programs are recognized by an increasingly large number of companies for their value in improving health and well-being of their employees, and increasing morale, loyalty, and productivity at work. A company may provide a gym with exercise equipment, start smoking cessation programs, and provide nutrition, weight, or stress management training. Other programs may include health risk assessments, safety and accident prevention, and health screenings. Some workplaces are working together to promote entire healthy communities. One example is through the Wellness Council of America. [1]
Environmental health
Environmental health comprises those aspects of human health, including quality of life, that are determined by physical, chemical, biological, social, and psychosocial factors in the environment. It also refers to the theory and practice of assessing, correcting, controlling, and preventing those factors in the environment that can potentially affect adversely the health of present and future generations [2]
Environmental health, as used by the WHO Regional Office for Europe, includes both the direct pathological effects of chemicals, radiation, and some biological agents, and the effects (often indirect) on health and wellbeing of the broad physical, psychological, social, and aesthetic environment, which includes housing, urban development, land use, and transport.
Nutrition, soil contamination, water pollution, air pollution, light pollution, waste control, and public health are integral aspects of environmental health.
In the United States, the Center for Disease Control Environmental Health programs include: air quality, bioterrorism, environmental hazards and exposure, food safety, hazardous substances, herbicides, hydrocarbons, lead, natural disasters, pesticides, smoking and tobacco use, water quality, and urban planning for healthy places. [3]
While lifestyles have been by far the leading factor in premature deaths, environmental factors is the second leading cause and has been increasing in its importance for health over the past several decades.
Environmental health services are defined by the World Health Organization as:
those services that implement environmental health policies through monitoring and control activities. They also carry out that role by promoting the improvement of environmental parameters and by encouraging the use of environmentally friendly and healthy technologies and behaviors. They also have a leading role in developing and suggesting new policy areas.
The Environmental Health profession had its modern-day roots in the sanitary and public health movement of the United Kingdom. This was epitomized by Sir Edwin Chadwick, who was instrumental in the repeal of the poor laws and was the founding president of the Chartered Institute of Environmental Health.
Mental health
Mental health is a concept that refers to a human individual’s emotional and psychological well-being. The Merriam-Webster dictionary defines mental health as «A state of emotional and psychological well-being in which an individual is able to use his or her cognitive and emotional capabilities, function in society, and meet the ordinary demands of everyday life.»
According to the World Health Organization (WHO), there is no one «official» definition of mental health:
Mental health has been defined variously by scholars from different cultures. Concepts of mental health include subjective well-being, perceived self-efficacy, autonomy, competence, intergenerational dependence, and self-actualization of one’s intellectual and emotional potential, among others. From a cross-cultural perspective, it is nearly impossible to define mental health comprehensively. It is, however, generally agreed that mental health is broader than a lack of mental disorders. [4]
Cultural differences, subjective assessments, and competing professional theories all affect how «mental health» is defined. In general, most experts agree that «mental health» and «mental illness» are not opposites. In other words, the absence of a recognized mental disorder is not necessarily an indicator of mental health.
One way to think about mental health is by looking at how effectively and successfully a person functions. Feeling capable and competent, being able to handle normal levels of stress, maintaining satisfying relationships, leading an independent life, and being able to «bounce back,» or recover from difficult situations are all signs of mental health.
Mental health, as defined by the U.S. Surgeon General’s Report on Mental Health, «refers to the successful performance of mental function, resulting in productive activities, fulfilling relationships with other people, and the ability to adapt to change and cope with adversity.»
Some experts consider mental health as a continuum with the other end of the continuum being mental disorders. Thus, an individual’s mental health may have many different possible values. Mental wellness is generally viewed as a positive attribute, such that a person can reach enhanced levels of mental health, even if they do not have any diagnosable mental illness. This definition of mental health highlights emotional well being as the capacity to live a full and creative life, with the flexibility to deal with life’s inevitable challenges. Some mental health experts and health and wellness promoters are now identifying the capability for critical thinking as a key attribute of mental health as well. Many therapeutic systems and self-help books offer methods and philosophies espousing presumably effective strategies and techniques for further improving the mental wellness of otherwise healthy people.
Population health
Population health is an approach to health that aims to improve the health of an entire population. One major step in achieving this aim is to reduce health inequities among population groups. Population health seeks to step beyond the individual-level focus of mainstream medicine and public health by addressing a broad range of factors that impact health on a population-level, such as environment, social structure, resource distribution, and so forth.
Population health reflects a shift in thinking about health as it is usually defined. Population health recognizes that health is a resource and a potential as opposed to a static state. It includes the potential to pursue one’s goals to acquire skills and education and to grow.
An important theme in population health is importance of social determinants of health and the relatively minor impact that medicine and healthcare have on improving health overall. From a population health perspective, health has been defined not simply as a state free from disease but as «the capacity of people to adapt to, respond to, or control life’s challenges and changes.» [5]
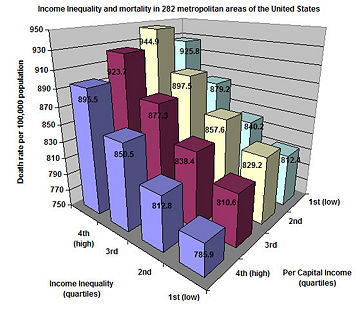
Recently, there has been increasing interest from epidemiologists on the subject of economic inequality and its relation to the health of populations. There is a very robust correlation between socioeconomic status and health. This correlation suggests that it is not only the poor who tend to be sick when everyone else is healthy, but that there is a continual gradient, from the top to the bottom of the socioeconomic ladder, relating status to health. This phenomenon is often called the «SES Gradient.» Lower socioeconomic status has been linked to chronic stress, heart disease, ulcers, type 2 diabetes, rheumatoid arthritis, certain types of cancer, and premature aging.
Population health parameters indicate, for example, that the economic inequality within the United States is a factor that explains why the United States ranks only 30th in life expectancy, right behind Cuba. which is 29th. All 29 countries that rank better than the United States have a much smaller gap of income distribution between their richest and poorest citizens.
Despite the reality of the SES Gradient, there is debate as to its cause. A number of researchers (A. Leigh, C. Jencks, A. Clarkwest) see a definite link between economic status and mortality due to the greater economic resources of the better-off, but they find little correlation due to social status differences. Other researchers (such as R. Wilkinson, J. Lynch, and G. A. Kaplan) have found that socioeconomic status strongly affects health even when controlling for economic resources and access to health care.
Most famous for linking social status with health are the Whitehall studies—a series of studies conducted on civil servants in London. The studies found that, despite the fact that all civil servants in England have the same access to health care, there was a strong correlation between social status and health. The studies found that this relationship stayed strong even when controlling for health-effecting habits such as exercise, smoking, and drinking. Furthermore, it has been noted that no amount of medical attention will help decrease the likelihood of someone getting type 1 diabetes or rheumatoid arthritis—yet both are more common among populations with lower socioeconomic status. Lastly, it has been found that among the wealthiest quarter of countries on earth (a set stretching from Luxembourg to Slovakia), there is no relation between a country’s wealth and general population health, suggesting that past a certain level, absolute levels of wealth have little impact on population health, but relative levels within a country do. [6]
The concept of psychosocial stress attempts to explain how psychosocial phenomenon such as status and social stratification can lead to the many diseases associated with the SES Gradient. Higher levels of economic inequality tend to intensify social hierarchies and generally degrades the quality of social relations, leading to greater levels of stress and stress related diseases. Wilkinson found this to be true not only for the poorest members of society, but also for the wealthiest. Economic inequality is bad for everyone’s health.
Inequality does not affect only the health of human populations. D. H. Abbott at the Wisconsin National Primate Research Center found that among many primate species, those with less egalitarian social structures correlated with higher levels of stress hormones among socially subordinate individuals. Research by R. Sapolsky of Stanford University provides similar findings.
Public health
Public health is concerned with threats to the overall health of a community based on population health analysis.
The size of the population in question can be limited to a dozen or less individuals, or, in the case of a pandemic, whole continents. Public health has many sub-fields, but is typically divided into the categories of epidemiology, biostatistics, and health services. Environmental, social and behavioral health, and occupational health are also important fields in public health.
The focus of a public health intervention is to prevent, rather than treat a disease, through surveillance of cases and the promotion of healthy behaviors. In addition to these activities, in many cases treating a disease can be vital to preventing it in others, such as during an outbreak of an infectious disease such as HIV/AIDS. Vaccination programs, distribution of condoms, and promotion of abstinence or fidelity in marriage are examples of public health measures advanced in various countries.
Many countries have their own government agencies, sometimes known as ministries of health, to respond to domestic health issues. In the United States, the frontline of public health initiatives are state and local health departments. The Surgeon General-led United States Public Health Service, and the Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia, although based in the United States, are also involved with several international health issues in addition to their national duties.
All of the areas of health, including individual health and wellness, environmental health, mental health, population health, and public health now need to be viewed in a global context. In a global society, the health of every human being is relevant to the health of each one of us. For example, a disease outbreak in one part of the world can quickly travel to other regions and continents, via international travel, creating a global problem.
Global health requires that the world’s citizens collaborate to improve all types of health in all nations, rich or poor, and seek to prevent, reduce, and stop disease outbreaks at their source.
Notes
References
External links
All links retrieved March 18, 2020.
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.
Перевод «the world health organization to» на русский
Всемирной организацией здравоохранения для
Vsemirnoy organizatsiyey zdravookhraneniya dlya
11 примеров, содержащих перевод
Всемирную организацию здравоохранения
Vsemirnuyu organizatsiyu zdravookhraneniya
9 примеров, содержащих перевод
Всемирной организации здравоохранения по
Vsemirnoy organizatsii zdravookhraneniya po
8 примеров, содержащих перевод
Всемирной организацией здравоохранения в целях
Vsemirnoy organizatsiyey zdravookhraneniya v tselyakh
3 примеров, содержащих перевод
что Всемирная организация здравоохранения
chto Vsemirnaya organizatsiya zdravookhraneniya
3 примеров, содержащих перевод
Всемирной организацией здравоохранения в том, что касается
Vsemirnoy organizatsiyey zdravookhraneniya v tom, chto kasayetsya
2 примеров, содержащих перевод
ВОЗ, чтобы
VOZ, chtoby
2 примеров, содержащих перевод
Всемирной организацией здравоохранения с целью
Vsemirnoy organizatsiyey zdravookhraneniya s tsel’yu
2 примеров, содержащих перевод
Всемирной организацией здравоохранения в вопросе
Vsemirnoy organizatsiyey zdravookhraneniya v voprose
What Does the World Health Organization Do?
Introduction
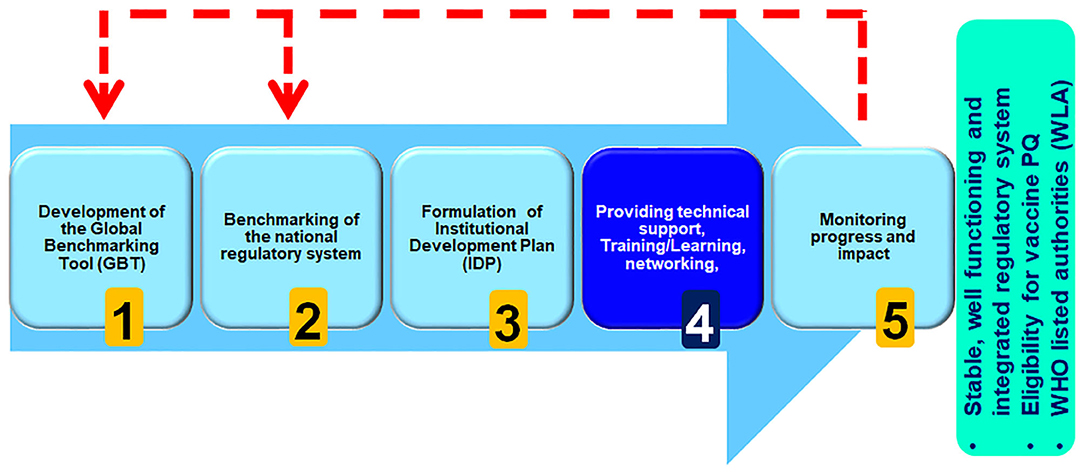
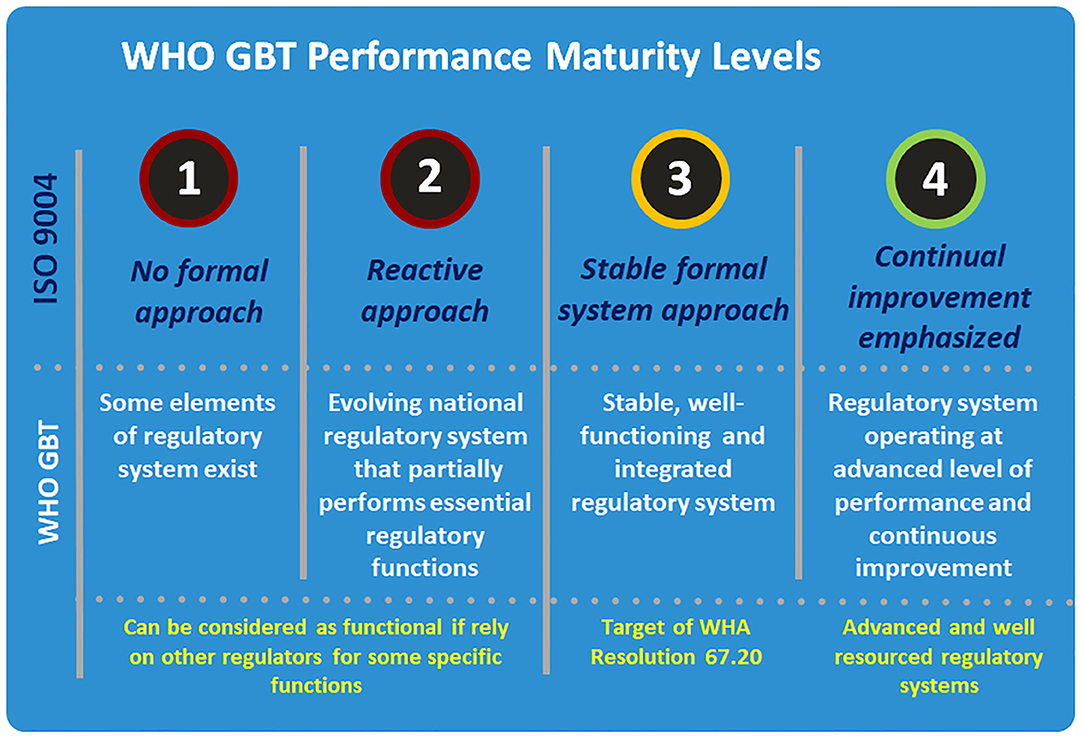
The World Health Organization (WHO) is the UN agency charged with spearheading international public health efforts. Over its nearly seventy-five years, the WHO has logged both successes, such as eradicating smallpox, and perceived failures, such as its delayed response to the Ebola outbreak in 2014.
In response, the WHO has undertaken reforms to improve its ability to fight future epidemics and boost the health of the hundreds of millions of people still living in extreme poverty. However, the WHO is in an uphill battle to loosen its rigid bureaucracy and it faces an increasingly troublesome budget. The COVID-19 pandemic has proved to be another monumental challenge for the health agency, sparking fresh debate over its effectiveness.
Why was the WHO established?
Created in 1948 as part of the United Nations, the WHO has a broad mandate to guide and coordinate international health policy. Its primary activities include developing partnerships with other global health initiatives, conducting research, setting norms, providing technical support, and monitoring health trends around the world. Over the decades, the WHO’s remit has expanded from its original focus on women’s and children’s health, nutrition, sanitation, and fighting malaria and tuberculosis.
What does the WHO do?
A summary of global news developments with CFR analysis delivered to your inbox each morning. Most weekdays.
The World This Week
A weekly digest of the latest from CFR on the biggest foreign policy stories of the week, featuring briefs, opinions, and explainers. Every Friday.
Think Global Health
A curation of original analyses, data visualizations, and commentaries, examining the debates and efforts to improve health worldwide. Weekly.
Today, the WHO monitors and coordinates activities concerning many health-related issues, including genetically modified foods, climate change, tobacco and drug use, and road safety. The WHO is also an arbiter of norms and best practices. Since 1977, the organization has maintained a list of essential medicines it encourages hospitals to stock; it has since made a similar list of diagnostic tests. The agency also provides guidance on priority medical devices, such as ventilators and X-ray and ultrasound machines.
Some of the WHO’s most lauded successes include its child vaccination programs, which contributed to the eradication of smallpox in 1979 and a 99 percent reduction in polio infections in recent decades, and its leadership during the 2003 severe acute respiratory syndrome (SARS) epidemic. The agency has the exclusive authority to declare global health emergencies, which it has done several times since its members granted it the power in 2007. At present, the WHO’s work includes combating the COVID-19 pandemic and other emergencies, as well as promoting refugees’ health.
In its 2019 strategy, the WHO identified three priorities [PDF] for its work over the next five years:
The WHO’s strategic priorities are rooted in the United Nations’ Sustainable Development Goals, a set of seventeen objectives for ending poverty by 2030.
How is the WHO governed?
The WHO is headquartered in Geneva and has six regional and 150 country offices. It is controlled by delegates from its 194 member states, who vote on policy and elect the director general. Tedros Adhanom Ghebreyesus, previously Ethiopia’s foreign minister, was elected to a five-year term in 2017 and reelected in 2022. He is the WHO’s first leader from Africa, and his election was the first time all WHO countries had an equal vote.
WHO delegates set the agency’s agenda and approve an aspirational budget each year at the World Health Assembly. The director general is responsible for raising the lion’s share of funds from donors.
What is the WHO’s budget?
The WHO has become increasingly dependent on voluntary contributions, which puts pressure on the organization to align its goals with those of its donors.
Some experts argued that the Trump administration’s moves seriously threatened the body’s effectiveness and cited budget cuts as a major factor in the WHO’s slow response to outbreaks. The eradication of polio could also place financial stress on the WHO, whose budget has for decades been bolstered by polio funding, and on lower-income countries that rely on international funding to keep up surveillance and immunization efforts.
How does the WHO fight global health emergencies?
Under the International Health Regulations (IHR), a legally binding framework drawn up in 2005 to prevent and mitigate health emergencies, WHO member states are required to monitor and report potential crises. Countries have historically been hesitant to report outbreaks, often because they’re fearful of economic repercussions. In 2003, for example, China denied for months that it was suffering an outbreak of the infectious disease that was eventually identified as SARS. Before the WHO declared China free of SARS in 2004, the disease killed more than three hundred people. In Ethiopia, Tedros himself was accused of downplaying cholera outbreaks while he was the country’s health minister; he denied these claims.
In an extraordinary crisis, the WHO can declare a public health emergency of international concern (PHEIC), which it has done six times: during the 2009 swine flu (H1N1) epidemic; in reaction to a reversal of progress in eradicating polio in 2014; amid the 2014 Ebola outbreak in West Africa; during the 2016 Zika virus outbreak in the Americas; once the ongoing Ebola epidemic reached the city of Goma in the Democratic Republic of Congo in 2019; and amid the global outbreak of the new coronavirus in 2020.
During a PHEIC, the WHO issues nonbinding guidance to its members on how they should respond to the emergency, including on potential travel and trade restrictions. It seeks to prevent countries in the surrounding region and beyond from overreacting and inflicting undue economic harm on the country in crisis. The WHO has hoped this would encourage affected countries to report outbreaks in a timely manner. However, experts say that, despite the WHO’s guidance, many countries continue to impose damaging travel and trade restrictions, a problem that was laid bare during the Ebola and COVID-19 crises. In an emergency, the WHO also spells out treatment guidelines and acts as a global coordinator, shepherding scientific data and experts to where they are most needed.
Additionally, the WHO provides guidance and coordination for emergencies that don’t rise to the level of a PHEIC. But declaring a PHEIC can help speed up international action and often encourages research on the disease in question, even if there is little risk of a pandemic. This was particularly true for the 2014 declaration for polio. At the same time, PHEIC declarations are contentious, and some argue that they can exacerbate ongoing outbreaks.
How has the WHO responded to COVID-19?
As it has done in past health crises, the WHO has provided medical and technical guidance as its experts investigate the virus, particularly new variants, as well as coordinated with world leaders on their national responses. It has also distributed critical supplies to member states, including millions of diagnostic tests and personal protective equipment for health-care workers. Additionally, it has helped to lead the global vaccination effort: the WHO partnered with the Coalition for Epidemic Preparedness Innovations (CEPI) and Gavi, the Vaccine Alliance, to launch COVAX, a global initiative aimed at providing equitable access to COVID-19 vaccines. By mid-2022, COVAX had delivered about 1.5 billion doses, falling short of its goal to distribute 2 billion by the end of 2021.
However, the WHO’s response has been the subject of controversy. Many experts have raised concerns about the agency’s deference to Beijing and increasing Chinese influence over the institution. Among other criticisms, they say WHO officials accepted misinformation from the Chinese government as the outbreak unfolded, waited too long to declare an emergency, and have shunned Taiwan because of bias toward China. Trump was particularly critical of the agency and in May 2020 he announced an end to the U.S. relationship with the WHO. (Biden reversed course on the U.S. exit immediately after taking office.) In January 2021, a delegation of WHO scientists traveled to Wuhan to investigate the virus’s origin, though its findings were inconclusive and critics say Beijing constrained the group’s work. The WHO has since established a new advisory group to continue research on the issue.
What reforms has the WHO made?
Under Tedros, the WHO has tackled another of its most enduring problems: political friction between its headquarters and its six regional offices, which critics say have enjoyed too much autonomy. Some say that tension between Geneva and the WHO’s Africa office, in Brazzaville, Republic of Congo, contributed to the agency’s poor response to the 2014 Ebola outbreak. To assert its authority over these regional power bases, the WHO has begun requiring staff to rotate among posts around the world, similar to a policy at UNICEF. While some observers paint this and other changes as merely cosmetic, others have applauded the reforms. “There is much greater cooperation than there was in the past,” global health expert Ilona Kickbusch said at a 2020 CFR meeting.
More recently, the COVID-19 crisis has prompted calls for major reforms. In a rare special session of the WHO’s World Health Assembly in 2021, delegates initiated the drafting of a global treaty on pandemic prevention, preparedness, and response. The proposal for a pandemic treaty has sparked debate, however, and the deliberation process could take years. At the 2022 assembly, countries agreed on a U.S.-led proposal to strengthen the IHR by increasing member states’ accountability around disease outbreaks, though no changes have been formally approved.
“Pleas for strengthening the WHO have remained prominent,” writes CFR’s David P. Fidler for Think Global Health. “However, this goal faces serious obstacles,” Fidler says, namely resistance from China, Russia’s war in Ukraine, and a lack of strong U.S. support for expanding the body’s authority and funding.
Recommended Resources
On The President’s Inbox podcast, CFR’s Stewart M. Patrick lays out what the WHO can and cannot do.
For Think Global Health, CFR’s David P. Fidler looks at the World Health Assembly’s slow steps toward global health reforms.
This CFR Independent Task Force report argues that the WHO has an important leadership role in public health emergencies but lacks the geopolitical heft to address their broader implications.
In Foreign Affairs, Laurie Garrett examines the WHO’s mishandling of the 2014 Ebola outbreak.
Plagues and the Paradox of Progress, a 2018 book by CFR’s Thomas J. Bollyky, discusses the WHO’s attempts to improve itself after the Ebola crisis.
This CFR Backgrounder describes ongoing global efforts to eradicate polio.
World Health Organization
Our editors will review what you’ve submitted and determine whether to revise the article.
Our editors will review what you’ve submitted and determine whether to revise the article.
Read a brief summary of this topic
World Health Organization (WHO), French Organisation Mondiale de la Santé, specialized agency of the United Nations (UN) established in 1948 to further international cooperation for improved public health conditions. Although it inherited specific tasks relating to epidemic control, quarantine measures, and drug standardization from the Health Organization of the League of Nations (set up in 1923) and the International Office of Public Health at Paris (established in 1907), WHO was given a broad mandate under its constitution to promote the attainment of “the highest possible level of health” by all peoples. WHO defines health positively as “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity.” Each year WHO celebrates its date of establishment, April 7, 1948, as World Health Day.
With administrative headquarters in Geneva, governance of WHO operates through the World Health Assembly, which meets annually as the general policy-making body, and through an Executive Board of health specialists elected for three-year terms by the assembly. The WHO Secretariat, which carries out routine operations and helps implement strategies, consists of experts, staff, and field workers who have appointments at the central headquarters or at one of the six regional WHO offices or other offices located in countries around the world. The agency is led by a director general nominated by the Executive Board and appointed by the World Health Assembly. The director general is supported by a deputy director general and multiple assistant directors general, each of whom specializes in a specific area within the WHO framework, such as family, women’s, and children’s health or health systems and innovation. The agency is financed primarily from annual contributions made by member governments on the basis of relative ability to pay. In addition, after 1951 WHO was allocated substantial resources from the expanded technical-assistance program of the UN.
WHO officials periodically review and update the agency’s leadership priorities. Over the period 2014–19, WHO’s leadership priorities were aimed at:
1. Assisting countries that seek progress toward universal health coverage
2. Helping countries establish their capacity to adhere to International Health Regulations
3. Increasing access to essential and high-quality medical products
4. Addressing the role of social, economic, and environmental factors in public health
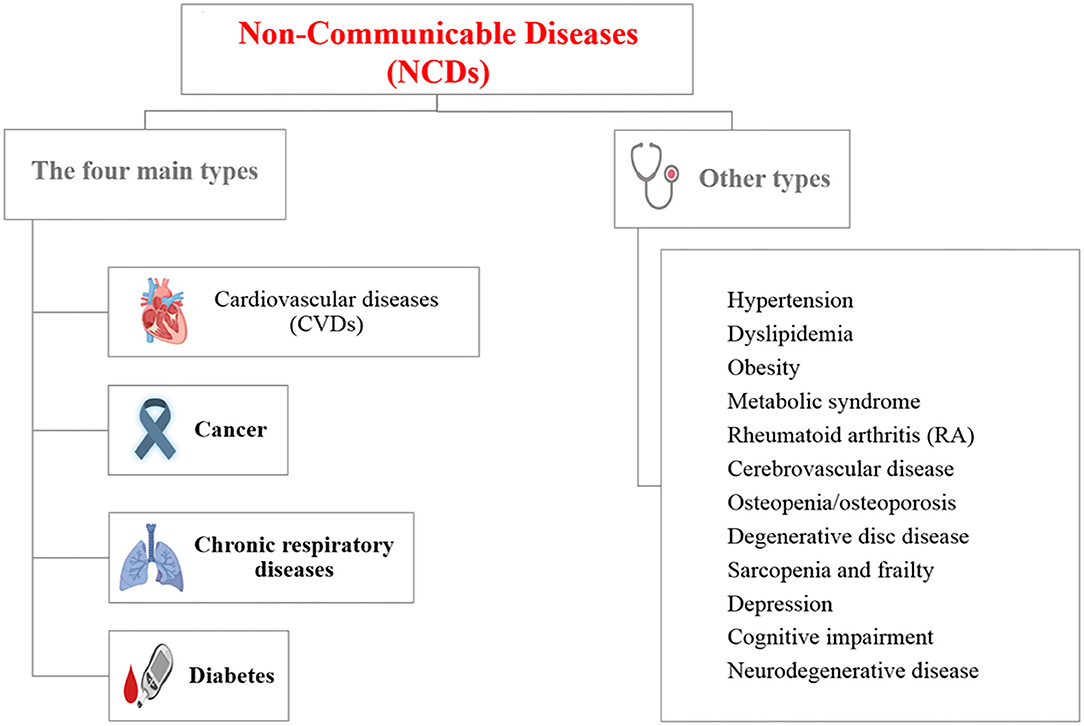
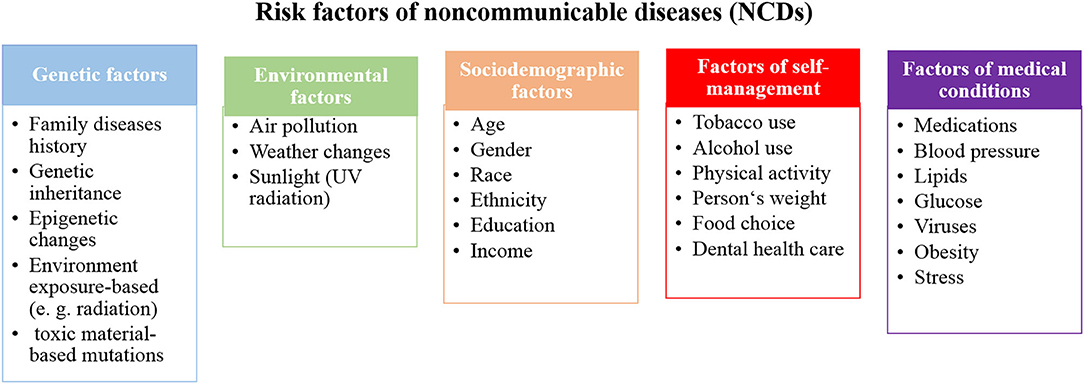
5. Coordinating responses to noncommunicable disease
6. Promoting public health and well-being in keeping with the Sustainable Development Goals, set forth by the UN.
The work encompassed by those priorities is spread across a number of health-related areas. For example, WHO has established a codified set of international sanitary regulations designed to standardize quarantine measures without interfering unnecessarily with trade and air travel across national boundaries. WHO also keeps member countries informed of the latest developments in cancer research, drug development, disease prevention, control of drug addiction, vaccine use, and health hazards of chemicals and other substances.
WHO sponsors measures for the control of epidemic and endemic disease by promoting mass campaigns involving nationwide vaccination programs, instruction in the use of antibiotics and insecticides, the improvement of laboratory and clinical facilities for early diagnosis and prevention, assistance in providing pure-water supplies and sanitation systems, and health education for people living in rural communities. These campaigns have had some success against AIDS, tuberculosis, malaria, and a variety of other diseases. In May 1980 smallpox was globally eradicated, a feat largely because of the efforts of WHO. In March 2020 WHO declared the global outbreak of COVID-19, a severe respiratory illness caused by a novel coronavirus that first appeared in Wuhan, China, in late 2019, to be a pandemic. The agency acted as a worldwide information centre on the illness, providing regular situation reports and media briefings on its spread and mortality rates; dispensing technical guidance and practical advice for governments, public health authorities, health care workers, and the public; and issuing updates of ongoing scientific research. As pandemic-related infections and deaths continued to mount in the United States, Pres. Donald J. Trump accused WHO of having conspired with China to conceal the spread of the novel coronavirus in that country in the early stages of the outbreak. In July 2020 the Trump administration formally notified the UN that the United States would withdraw from the agency in July 2021. The U.S. withdrawal was halted by Trump’s successor, Pres. Joe Biden, on the latter’s first day in office in January 2021.
In its regular activities WHO encourages the strengthening and expansion of the public health administrations of member nations, provides technical advice to governments in the preparation of long-term national health plans, sends out international teams of experts to conduct field surveys and demonstration projects, helps set up local health centres, and offers aid in the development of national training institutions for medical and nursing personnel. Through various education support programs, WHO is able to provide fellowship awards for doctors, public-health administrators, nurses, sanitary inspectors, researchers, and laboratory technicians.
World Health Organization’s Ranking of the World’s Health Systems
Some people fancy all health care debates to be a case of Canadian Health Care vs. American. Not so. According to the World Health Organization’s ranking of the world’s health systems, neither Canada nor the USA ranks in the top 25.
Improving the Canadian Healthcare System does not mean we must emulate the American system, but it may mean that perhaps we can learn from countries that rank better than both Canada and the USA at keeping their citizens healthy.
World Health Organization Ranking; The World’s Health Systems
| 1 France 2 Italy 3 San Marino 4 Andorra 5 Malta 6 Singapore 7 Spain 8 Oman 9 Austria 10 Japan 11 Norway 12 Portugal 13 Monaco 14 Greece 15 Iceland 16 Luxembourg 17 Netherlands 18 United Kingdom 19 Ireland 20 Switzerland 21 Belgium 22 Colombia 23 Sweden 24 Cyprus 25 Germany 26 Saudi Arabia 27 United Arab Emirates 28 Israel 29 Morocco 30 Canada 31 Finland 32 Australia 33 Chile 34 Denmark 35 Dominica 36 Costa Rica 37 USA 38 Slovenia 39 Cuba 40 Brunei 41 New Zealand 42 Bahrain 43 Croatia 44 Qatar 45 Kuwait 46 Barbados 47 Thailand 48 Czech Republic 49 Malaysia 50 Poland 51 Dominican Republic 52 Tunisia 53 Jamaica 54 Venezuela 55 Albania 56 Seychelles 57 Paraguay 58 South Korea 59 Senegal 60 Philippines 61 Mexico 62 Slovakia 63 Egypt 64 Kazakhstan | 65 Uruguay 66 Hungary 67 Trinidad and Tobago 68 Saint Lucia 69 Belize 70 Turkey 71 Nicaragua 72 Belarus 73 Lithuania 74 Saint Vincent and the Grenadines 75 Argentina 76 Sri Lanka 77 Estonia 78 Guatemala 79 Ukraine 80 Solomon Islands 81 Algeria 82 Palau 83 Jordan 84 Mauritius 85 Grenada 86 Antigua and Barbuda 87 Libya 88 Bangladesh 89 Macedonia 90 Bosnia-Herzegovina 91 Lebanon 92 Indonesia 93 Iran 94 Bahamas 95 Panama 96 Fiji 97 Benin 98 Nauru 99 Romania 100 Saint Kitts and Nevis 101 Moldova 102 Bulgaria 103 Iraq 104 Armenia 105 Latvia 106 Yugoslavia 107 Cook Islands 108 Syria 109 Azerbaijan 110 Suriname 111 Ecuador 112 India 113 Cape Verde 114 Georgia 115 El Salvador 116 Tonga 117 Uzbekistan 118 Comoros 119 Samoa 120 Yemen 121 Niue 122 Pakistan 123 Micronesia 124 Bhutan 125 Brazil 126 Bolivia 127 Vanuatu | 128 Guyana 129 Peru 130 Russia 131 Honduras 132 Burkina Faso 133 Sao Tome and Principe 134 Sudan 135 Ghana 136 Tuvalu 137 Ivory Coast 138 Haiti 139 Gabon 140 Kenya 141 Marshall Islands 142 Kiribati 143 Burundi 144 China 145 Mongolia 146 Gambia 147 Maldives 148 Papua New Guinea 149 Uganda 150 Nepal 151 Kyrgystan 152 Togo 153 Turkmenistan 154 Tajikistan 155 Zimbabwe 156 Tanzania 157 Djibouti 158 Eritrea 159 Madagascar 160 Vietnam 161 Guinea 162 Mauritania 163 Mali 164 Cameroon 165 Laos 166 Congo 167 North Korea 168 Namibia 169 Botswana 170 Niger 171 Equatorial Guinea 172 Rwanda 173 Afghanistan 174 Cambodia 175 South Africa 176 Guinea-Bissau 177 Swaziland 178 Chad 179 Somalia 180 Ethiopia 181 Angola 182 Zambia 183 Lesotho 184 Mozambique 185 Malawi 186 Liberia 187 Nigeria 188 Democratic Republic of the Congo 189 Central African Republic 190 Myanmar |
125 Comments
France’s excellence in health care delivery is probably due to two major factors: 1) it is extraordinarily open and communicative with patients and families which reaps significant patient safety benefits; and 2) it has far more doctors per capita so physicians want patients and patients get a choice.
I lived in France and you can go to a pharmacist and be diagnosed for common ailments and walk out with an Rx in 15 mins. Bad ass!
French have a real Universal Healthcare System and unlike we Americans are not stupid to call it Socialistic Healthcare System. As much as military industrial complex for its own benefits unjustly frightened us from Socialism, Private Insurance Industry for same goal, with using same tactic an same word, frightening us from Universal Healthcare System, and as much as we were stupid in believing MIC bull shits, we are stupid in believing PII bull shits. Of course a corrupt and criminal party like Republican Party in harmony with a do nothing but talk too much, but as much corrupt party like Democratic Party helping them as much as they can, but main factor is our own absolute ignorance and stupidity.
Universal health care is socialized medicine.
And why exactly is that bad? Sorry, when the US is ranked so low, despite the highest health expenditure in the world, maybe you need to let go of ideology and actually look at some evidence.
Under socialized medicine population health and minimizing public health care costs always trump what’s best for individual patients. It’s one thing for a person to voluntarily give up their freedom to a health care collective promising free health care for all. But it’s a whole different thing if that person or group of persons summons the power of government to forcibly remove the freedom of others.
I totally disagree with Heather… The evidence is apparent in the rankings…. Private healthcare is far more frightening than socialized and far less effective: when health has a profit making motive, you will never reap the benefits of excellent healthcare. The only problem you have with socialized healthcare is that it fully depends on the motivations of your government and how apathetic the population are when it comes to legislative changes that curb things that were previously considered rights. Im from the UK and i can say that the NHS was fantastic though it has declined since tony blair first started to cut its funding… This has been exacerbated under david ham head cameron! But i would much rather have the NHS than an american style alternative… Nixon even said that the US healthcare system had a profit making motive, i do worry that we, in the UK are heading in the same way…. I have much empathy for americans who have suffered or lost prople as a result of that system. Everyone should have the right to healthcare.
Helen,
The profit motive helps drive innovation and excellence in health care.
People from countries around the world travel to the US for health care.
It’s wrong to force citizens to depend on the motivations of their government for access to health care. Everyone should have the freedom to spend their own money on their own health care in their own country.
Heather,
no the profit motive does not inspire innovation, if that be the case with the way we spend and go for profit we would have the number one health system, with a much lower negative outcomes, and way better access to care. To profit off of illness is a sick sad, and disgusting way to run a system. If the government is to make decisions on how healthcare is run then that would work best in a country with no parliament and direct voting. if we use the democratic processes we founded this country on (in Ideology) then the government would have to run it the way the people want it.
What’s wrong with the profit motive? Every employee in a public health care system personally benefits from the profit motive. The only difference under a public health care system is that the government controls the profit motive and decides which groups and corporations will benefit the most. Democracy works best with a limited government otherwise the biggest groups end up calling the shots for the rest of us.
Heather: Private healthcare DOES NOT “drive innovation and excellence in health care” – it makes doctors over-prescribe (for commission on medicine) and request useless tests that are not needed, just because it will make the hospital more money.
About 6 months later I moved to Spain (public health service) – went to hospital and found out I have a malignant tumor and needed an operation urgently to remove it.
Private healthcare also demands that the doctors can charge whatever they like and if you don’t like/can’t afford then you don’t get treatment.
There should always be the choice of public and private, but it should be the right of every citizen to have access to basic healthcare.
Robert,
A free market offering choice, competition, and price transparency does drive innovation and excellence by increasing quality and reducing price. Misdiagnosis can happen in private or public health care. Doctors who place profits ahead of providing high quality medical services to their patients can be found practicing in private and public health care systems (i.e. fraudulent Medicare claims). In a free market these doctors would soon find themselves out of business, but here in Saskatchewan doctors are paid by Medicare regardless of the quality of care provided.
Public health care demands that doctors help ration care to save the system money. Here in Saskatchewan the regional health authorities allocate money to diagnostic tests and surgeries. If your regional health authority can’t afford it then you don’t get treatment which is why we have government-mandated waiting lists.
The Canadian Charter of Rights and Freedoms doesn’t guarantee a right to benefits from a government program like Medicare – nor should it. What is unjust in a free and democratic society is that a government monopoly on health care not only infringes on our legal “…right to life, liberty and security of the person…” but leaves no option for escaping the harms caused by this infringement.
Is there a rubric to the rankings. If you look at patents on medicinal items, Israel is first, and American is 2nd. If the rubric has 20% of its value on being affordable (whatever that means), and 20% on survival rates, then I disagree. I’d rather be alive and broke than dead with money. If there is a high percentage on low costs, but no reference to innovative discoveries, I also disagree. In short, without the rubric for judging systems, this “ranking” is meaningless.
It’s strange how Americans trust private profit driven organisation’s over their own government. When we use the private sector in the UK it’s very rarely has a good outcome. You’re government tries to do the best by its people or we vote them out. In the UK you can still have private healthcare and pay insurance and about 11% of people do. This is choice in the US if you get cancer the chances you will go bankrupt. In the European countries all your treatment is paid for, prescriptions are often free for a number of years after diagnosis. In most European countries the life expectancy is higher than the US and we spend much less than the US. People need too look at the facts and move away from their suspicions of socialised. Trust me if I’m ill I don’t worry about money I just go to the doctor, no it’s not perfect but it’s better than going bankrupt.
These comparisons are for the most part meaningless, yet we keep trudging them out as if there was some gem to be revealed. All of the data comes from self-reporting entities. There’s no standardization and there’s very little commonality. That’s why you’ll see similar national health care systems have significantly different rankings. If outcomes were measured consistently, we’d see consistency in the rankings. (no one every explains why we don’t because that wouldn’t further an agenda) I’ve seen one “study” ranking UK as #1, which this ranking has them quite a bit further down the list. So why the disparity? I don’t suppose it would be that there are certain incentives that certain providers receive based on certain data? (Naw that would harken to much back to the days of the USSR.) The US usually ranks lower in these studies because there is less incentive to hide data-sets or pad stats on outcomes. Do we not see some correlation between the incentives provided by governments as part of reimbursement and the outcomes that get reported? Is there any disincentive in those very same countries for skewing self-reported data? I know people will want to believe what they want to believe, but to rely on these data sets as being meaningful for policy positions is to build your house out of a deck of cards. (remember My Cousin Vinny? seems like P.T. Barnum is alive and well.)
It’s bad because our government says it’s bad (for profit). A society of sheep that think they are individuals.
No true… these are just political terms… the question and debate is deeper than politics. notably, is healthcare a basic human “right” or a “privilege?” I’m an american living in France and can tell you the french system works because the french see healthcare as a human rights issue. Right or wrong, good or bad, this is the french mentality. This debate in the US will only be resolved when we can answer this question. Free market capitalism favors healthcare as privilege and its in the blood of every American (republican, democrat, etc.) Like it or not, this is who we are… This is how our society was built. The french see paying taxes to support their healthcare system as totally reasonable. Taxes are an anathema to almost every American.
‘Taxes are anathema to almost every American’? Please. It’s the ridiculously low tax rates of the 1% and the hugely unequal business taxes that favor large corporations that are anathema to any American with a brain, including not a few of the 1%.
Government is an essential component of Democracy. Taxes are like dues to be a member of the democracy. Do I want my life run by huge corporations? No, I want a government that can control those corporations whose only duty is their executives and their largest shareholders. Your outlook is strictly a Republican outlook. It may be shared by some Democrats, but not many. I’m 66. I grew up with an anesthisiologist at each and of the dinner table. I was for National Health Care then and I am for it now, even more so. My sister-in-law is a Harvard MS family doc who is extremely discourage with the devolution of US healthcare into the mess that it now is. To whatever degree the ACA struggles it is largely due to 60 yrs+ of Republican intransigence and the disfunctional system that very few Europeans would sacrifice their access to their system to be part of ours. Relatively few Canadians live in Seattle and very few Europeans. Healthcare is one of the reasons. I know now what an extortionary, corrupt system we have created by pretending that free market’s are good to begin with and that we ever had a free market in US healthcare. Free markets do not exist where pricing is not transparent. Healthcare is the most expensive thing in most Americans lives but nobody, including the doctors knows the price of any medical service. So if you wanted to compare prices from one place to the other, or given the extreme costs in the US, send out your procedure for bids. I don’t think so.
Once again this is a system that has been completely taken over by huge corporations.
Secondly when you restrict the number of physicians both internally and externally (from outside the US) it is absolutely NOT a free market. This has been going on since I was a kid in the 50s at least. France has 50% more physicians/capita than the US.
Heather isn’t thinking. There are many thing wrong with her story. Most basically, whereas she reveres competition as a trait of capitalism as most of its defenders do, every capitalist from day one strives and struggles to eliminate competition, and by eliminating competition they have brought us to a place of less choice due to 6 major Big Banks, 5 manufacturers of household appliances, a handful of major health insurance companies, and on and on. And the profits that she praises and defends mean health insurance companies, to increase profits, are motivated to find innovative ways to pay out less in benefits while charging more for premiums.
No, it is not. You should learn vocabulary.
Heather, you and people like you are the problem. The GOP has you buffaloed with their scare tactics.
What scare tactics? This is real life.
real world – a great society cannot be borne of the elderly and infirmed. People are made to suffer to what end?
Wrong. Bismark model in Germany is completely privatized and there is universal coverage.
of course, only a Republican would dig their heels in to protect the WORST health system in the developed world. The American “your-money-or-your-life” health non-system consistently ranks DEAD (no pun intended) LAST or next to last in all positive measures (quality, accessibility, affordability, outcomes, healthy lives) but it makes a FEW VERY RICH to deny other access to affordable care – so, to Republicans, it’s the “best” system in the world and must be protected!
Call it what you want but it does work better than our current system
And that seems to be a very good thing in this case. In America, we are made by the government to have insurance on our cars, our public schools are paid for by taxes, our public libraries, too. The list is rather long, and we haven’t all been put in chains. Time to recognize the new world, folks. Universal coverage just sounds better to those who are so paranoid about socialism. It’s just a word.
Socialism is not just a word in Venezuela.
Fast forward to today August 3rd 2017………..now tell that to the UK baby, the hospital held that baby hostage……….WOULDN’T ALLOW IT TO COME TO THE US, FOR TREATMENT, EVEN THOU THE PARENTS HAD RAISED MONEY TO COME, SO YOU SOCIALIST CAN TAKE YOUR UNIVERSAL CARE AND SHOVE IT WHERE THE SUN DON’T SHINE.
Medicare is socialized medicine. Medicaid is socialized medicine. Healthcare for vets is socialized medicine. As someone on medicare I can attest to the fact that it’s a great system, though it certainly has problems. I had far more problems, however, when I was dependent upon profit-motivated companies to provide me with health insurance. I have absolutely nothing against profit-motivated companies, especially as I’m a business owner myself. They just aren’t a very good solution to providing coverage when the demand for healthcare has a very low level of elasticity. We need to stop thinking in terms that create knee-jerk reactions and start thinking about what works best.
Road construction and maintenance, railroad systems, law enforcement, fire protection and many. many other services are socialism, too. So is the U.S. system of tax exempting religious institutions so far as providing fire, police and other public services is concerned. I don’t hear “socialism” opponents protesting that.
“Socialized” medicine is a term only used in the USA. It’s meaningless elsewhere. The USA has an army, a navy, and an airforce, but doesn’t describe these as ‘socialized defence’. We recognise threats to our nation’s health as a threat to our nation. But doctors, drugs companies, medical equipment manufacturers, continue to operate privately and for profit. The UK’s NHS is not socialized. It was ‘nationalised’ during the war when our cities were being bombed. It’s just like defence.
The UK, like most European countries have a degree of private practice – which performs less well than the NHS. The example lower down of a UK patient refused an operation in the US, was a patient expecting the UK to fund care from taxation. There are plenty of examples of US patients refused care by their insurer.
Just curious why we want to place more financial responsibility in the hands of a government that continues to go in debt and can’t guarantee the taxes paid towards Medicare social security will every be available to anyone under the age of 40? To expand government control over already government regulated areas seems insane. Balance budget and reduce national debt before adding more responsibility and money to a incompetent government, regardless of party. If this doesn’t seem sensible, please send me your money and I’ll take care of your money as well as government is now.
The World Health Organization said that Columbia has one of the worst health care systems in the world yet, they ranked them #22 because they had equal access to that terrible system. The USA was ranked number 1 in quality but was ranked #37 because quality only counts 10% toward the rating. Typical of liberal think.
I think you misread that a bit. The US system is ranked 24th, so it’s pretty good but definitely not ranked #1. When you combine that with the fact that we are the most expensive and rank horribly in the accessibility categories, I think 37 is almost generous.
The US health care system is so screwed up it makes it impossible for most people to retire because of the high cost of insurance–even the new Obama care is unaffordable. Third world countries have better health care systems than us. I can only attribute it to the greed of the people who run this country. As said earlier, our government treats health care as a privilege for those who can afford it. Why should we have to “shop” for an insurance that is “best” for us? Why aren’t all of the plans the same, so that no matter what you need to see a doctor for, whether a cold or cancer, the overall cost you pay per month for this service is the same for everyone! That is equality! That is the way health care should be! And don’t give me that socialist crap!
you nailed it Beth. I am a healthcare practitioner and most of my constituients share the exact sediments …kudos
“Third world countries have ‘better’ health care systems than us.” Alright Beth, I challenge you to go have your heart transplant in a third world country if you ever need one.
The WHO rankings are completely devoid of any common sense. Ranking third world countries higher than the US is completely ridiculous. Don’t just believe any biased statistics you hear. Look more closely. Use your brains people.
Why in the world should it be the same across the board? Why should a group of nuns have to pay for birth control/child birth expenses? There is a case going on right now where a nunnary is being charged tens of millions over that. Why should a single (or not) male be responsible for mammograms and other female care? Why should a woman be responsible for a man’s prostate trouble? And why in the world should I be responsible for a smoker’s lung problems or an addict’s treatment?
I extremely disagree with the push for privitisation in my home country of Australia. Many years have gone past where I have had no need for the medical system. The barely noticable standard amount deducted from my income tax to contribute to our countries healthcare is something I’m more than happy to do for my fellow countrymen, regardless of personal usage. Take care of the people around you, simple! I don’t buy into the ploy of ‘I didn’t use this, I don’t do that, so therefor..’ game. In my opinion it has been cunningly exploited by privitisation advocates as justification to leave their brothers and sisters out in the cold. A business has a primary goal to make more money than it did the year before! that and caring for people in need don’t mix too well. The motivations behind systems of care, governance and infrastructure right across the board in most places need to be addressed. Everyone pays their percentage, one that is adequate for research too. By that system the need for profit is taken out of the equation, reducing cost. Medical advancements made in reserched tech. advancements can then also be implemented at cost. With patients not needing insurance approval or lump sums of cash to get what they need to survive or have quality of life, the knock on effects to society and the way we think about caring for others is a step in the right direction we all need.
I’ve been to 77 different countries, experienced (through my work) healthcare offered in at least 20, France, russia, iceland, denmark, australia to name a few, the USA has (b4 obamacare) the absolute, hands down – no completion, most advanced healthcare to offer to it’s poorest citizens. obama care has created what was once a classless system into a class system of healthcare- wait in line, panel decides your procedure to be performed by fewer docs/specialists.
WE’VE BEEN RIPPED OFF
Many doctors are now opting out of socialized medicine in the USA and offering fee for service directly to their patients. This is the only way to save the doctor/patient relationship and the practice of medicine.
The USA does NOT have SOCIALIZED medicine, but according to the rankings the countries that do HAVE socialized medicine are at the top of the list and the US is #37. Where do you live.
Hi Diane,
Socialized medicine is known as Medicare in Canada and Medicare and Medicaid in the United States.
I don’t understand your comment that the government decides the quantity and quality of your healthcare. You are free to go to any doctor you want, as many times as you want. The quality is somewhat regulated – there are very few medical education systems in the world that Canada will accept doctors from without requiring further medical education.
Some provinces restrict how many patients a doctor can see in a day to try to improve care.
So you don’t think that quality should be weighted by access?? So what if a country of 1000 people had all of the worlds best doctors and only 500 people had access to them. 200 people. 5 people!? The others would just die, or go bankrupt getting the proper care.. Access is clearly a HUGELY important variable in the equation – and each country has vastly different rates.
The capitalist approach certainly does stimulate research, but not necessarily for effective cures. Often times it creates marketing for ineffective cures, that the company holds patents on and has the means to promote. Other times it creates ailments and syndromes to fit products it has on the shelf. The mere fact that Cuba,an impoverished nation, ranks very near to the US in effective healthcare, belies the capitalist argument. Politicizing healthcare is it’s biggest impediment.
I think it breaks down to health care for profit. The motivation will always be to improve the bottom line. So the underline story is to supply cheaper healthcare but in reality, it’s simply less coverage.and victims are simply chronic complainers
Genetics should make health care better yet for insurance companies they regard this as a new cash tool. Your genetics will help identify the possible probability of your future health care failure and you will be assessed on these risk also.
Canada’s health care is not perfect but at about 11% of GDP compared to the US at over 18%, better longevity(close to 3 years) and a lot fewer birth deaths. It seems simple decision with just those few stats “longer life, lower cost”
But it is painfully evident to me that the two party system with it’s inability to purge the deadwood has contributed to the polarity we now see.
It is not what is required but simply what is politically feasible or possible. What can be done that will appease the electorate without negatively affecting our fund raising for the next election which is always two years away.
Bad power and mostly greed are killing my southern friends and for the most part, all we can do is watch. If I can make but one humble suggestion in planning the future for next generation: If you want to make America great again consider giving the same reverence to health care and education as you do the second amendment and gun control. And if you don’t believe that look at America after WW2 with the VA, the GI Bill, and the Marshall plan.
Do you have a source of this ranking? Thanks.
Paolla,
This information is available on the World Health Organization’s website at http://www.who.int/whr/2000/en/
The ranking is contained in Annex Table 10 available here http://www.who.int/whr/2000/annex/en/index.html
Admin – This is not the source for the data you cite. On the “Annex 10 Table” Canada ranks 30th and the United States is 72nd. There are a variety of tables in the WHO report which rank the countries on different criteria, thus moving the order around. Which table are you citing here, as it is not the “Over All Performance” table. Thanks.
April,
The citation is correct. Perhaps you read the table too quickly.
Hi Admin,
How the HELL is NZ behind America? NZ has GREAT healthcare. We don’t require insurance and we have free care paid for by taxes in emergency situations, or if you need an operation. The only drawback is the waiting time for surgeries but, beyond that, at least we don’t have to pay insurance companies a cent.
America, on the other hand, are slaves to the healthcare system(although I’m looking forward to see what the ACA does).
Looking forward to learning something new,
– Adam
The World Health Organization said that Columbia has one of the worst health care systems in the world yet, they ranked them #22 because they had equal access to that terrible system. The USA was ranked number 1 in quality but was ranked #37 because quality only counts 10% toward the rating. Typical of liberal think.
Andy1555, where do you get your info. The WHO did not say Columbia has one of the worst!! In fact, they have one of the best. I know people from the US that go there specifically for their healthcare. You know little about this, based on your last comment you must be a conservative that falsely believes that the US has the best of everything. Open your eyes, get off your mother’s couch and experience the world.
This is from the year 2000. Anything a little more ‘current’?
Why? Has our system, or any other, changed much? ( dont say ours has, ACa isnt active yet.)
Oh yes it is…..just wait until the employer mandate kicks in January 2015. Talk about all hell breaking loose. Then you will understand that the ACA has very little to do with health care.
Of course everyone thinks they are as or more important than the next guy. We are a fast food society which expects everything now, regardless of how hungry you are. As someone who has experienced both health care systems (the US and Canada) first hand I can tell you, the wait times are not much different. However, in the US if you have private insurance, you will be greeted with open arms like your checking into the Hyatt Regency. In Canada you are greeted with disdain and told to sit down. In the US the floors are shinny buffed with an expensive machine daily using some kind of toxic cleaner and wax. In Canada the floors are dull but clean having been cleaned with some environmentally safe cleaner but without the special polymer based coating. Canadians are mostly treated like cattle. The quality of health care is not much different depending on your condition. The US has centers of excellence which do advanced research and are well funded. In Canada there is advanced research on a much smaller scale. In the US if you don’t have insurance you avoid seeing the doctor unless your on your death bed, in Canada people fill Emergency rooms with relatively minor complaints, or you see you GP on a regular basis. The treatments in Canada are more standard and well tested and endorsed by Health Canada, even stricter then the FDA. As for the so called rationing, it’s not really rationing, it’s prioritizing based on the urgency for treatment, if it can wait it will while the resources are committed to the people who can’t wait. in the US resources are committed to the people who can pay others are directed to free clinics.
This is all true – but only for the wealthy Americans. I’ve been to free clinics, and they are nothing like what you describe here. In Canada, at least everyone has a fair and equal chance to seek treatment. You don’t have to be nobility or a lottery winner to get health care like you do in the U.S.
I have lived in both countries. Received and had relatives receive treatment in both countries. I prefer USA. You pay for treatment there, true. But we pay for it here, too. In taxes.
http://www.fraserinstitute.org/research-news/display.aspx?id=18858
I was neither a lottery winner, nor nobility. I’m just a blue-collar stiff.
When Canadian politicians and bureaucrats leave the country to seek medical care they go to the United States.
When politicians and bureaucrats in the USA seek medical care, they go to the best facilities and doctor’s available. One has to be a very wealthy Canadian to seek care in the USA. Those who have no health insurance in the USA go to ER when they are often in dire situation and would never get a knee replacement if needed. No one in Canada goes without health care.. Everyone gets what they need though elective requires wait.
Mary,
When Canadian politicians leave the country to access free market medicine they go to the USA. Many Canadian patients, who are not wealthy, are forced to leave Canada to access medical care in the USA. Everyone in Canada has government health insurance but not access to medical care. Right now close to 20,000 patients in Saskatchewan are being forced to wait on lists for medically necessary surgery.
Am Canadian and knowthe system … I know people who have needed surgery and did not get it (so they continue in pain) … know people who are suffering while waiting MONTHS just to get an appointment with a specialist … know people who have been on a gurney for days in emergency because there were no rooms available (not exagerated by the way, 3 nights in emergency in the hall way) … People in Canada go without the health care they need all the time! I believe it´s different from province to province … Now living in Mexico, and – based on personal experience – Mexico should be ranked high in the medical facilities and doctors.
This report was published in 2000 with source data from 1997, so the data is now 14 years old. I wonder when they will publish more current rankings and how/if they will differ?
I had a look and see that there has been another World Health Report, published in 2010, but I did not find any world-wide rankings for health systems.
Andrea,
Each of the WHO’s reports covers a specific subject. Their 2010 report is about the financing of health systems. Their next report will cover health research. I’m not sure if or when they will revisit health system performance but you’re right it would be interesting to see how current rankings would compare. Let me know if you come across any current studies or reports covering health system performance.
Will do. Thanks for your response.
Well I say that I had bad experience in Canada or Ontario with the healthcare, it’s free but I have to say it’s not the best. I had to get stiches done and I had to wait for 13 hours to get myself treated by a doctor, and the nurses basically ignored me during that time and told me to sit down. And I basically waited for 13 hours by the doctor. Once I got thru the doctor, he was rude, same as the nurse that was standing by him. Well I got my sitches, but I had to pay for the medication and cruches. Finally I can’t find any family doctor, that I can go reguarly the once a year thing, or if I have some illness I can’t have a family doctor.
Now I’ve been living in Brazil for 3 years now, and we have here two systems the private and public. Now I went thru both, the private I say was excellent no wait times nothing. Doctor treated me with respect and looked after me. Now for the public which people complained about it, well I had a biking accident nothing serious, but had to get also stiches. I was actuall closer to a public place than a private, so I went there. Didn’t have to have any ID just showed up, and as soon as I got there the nurse told me to go to the doctor’s office. I waited there for 2 minutes and the nurse showed up and looked at my knee, well he cleaned it up, and said the doctor will come and see you shortly, 10 minutes later the doctor showed up, and said well we have to give you anesthetic to your knee so we can remove all the small debrees in it, then also stich it up. Well he did it, and after stiching me up he bandaged my knee, and said to go to the other room to get a tetanus shot. He was really friendly, and told me some jokes. Finally on the other room the nurse showed up right away and gave me the shot. And told me to come back tommorow to change the bandage, and I went there for 7 days, to change it and after the 10th day they removed the stiches. I say I was impressed, and I don’t know why people complained about it, and I even told the doctor how it was in Canada, and he just chuckled. Well I know now where I can go and where I don’t have to spend a dime on medicines shots and doctors consultation.
Bruno,
It’s interesting to note that Brazil has both a private and public health care system. Public health care, whether it’s in Canada or Brazil, is not free. At least in Brazil you can exercise your freedom of choice in health care and pay to access medical services in the private system. Thanks for sharing your experiences.
Reverse comparisons, with the US being slow, inattentive and rude but Canada being prompt cheerful and efficient are easily found. This is why statistics matter.
this information is dead wrong… Brazil is on 125 place? How come? They have socialized universal health care and Brazilians never had any problem reaching for doctors or treatment of any kind without being charged for… USA should the on the very bottom of the list, since besides being awfully expensive, they have all the technology but no experience or touch.
I am Brazilian and I have to say you people had great experiences with our health care that do not correspond to the true thing. Indeed we have a universal health care system that is amazing in theory, but does not work how it should.
This list is somewhat BS…….but aside from that….lol……I dont have healthcare, and I live in the U.S.A. …..I go to Canada…….I have healthcare. …….Any questions?……. Something is better than nothing at all.
Taiwan is not a part of the United Nations. The W.H.O. (World Health Organization) only rated members of the U.N.
if saudi arabia is better than jordan, y are all saudis coming to jordan when they can be treated in their country for free.
“Improving the Canadian Healthcare System does not mean we must emulate the American system” thank you for saying this. Canadians have a tendancy to obsessively make comparisons with the U.S., especially on the topic of healthcare. both systems have their flaws, no doubt, but what bothers mw the most about the Canadian system is that you have NO CHOICE in how you are treated. You only have what the government is offering, and it’s often mediocre at best. Canada is supposedly of free country, we have the freedom to purchase whatever house, car, etc we want, but we have NO CHOICE on how our health will be managed. This essentially means that the government owns our bodies and decides how we will be cared for, this is exactly how the soviet union healthcare system was managed. To my knowledge there are only 3 countries in the world where you have no private options of health care: Cuba, North Korea, and Canada!
It is problematic that we are talking about the “Canadian Health Care” system, when in fact there is no such thing. With notable exceptions where health care pertains to First Nations treaty guarantees, the federal government has a very limited involvement in health care.
I have lived in several provinces, and can tell you from experience that Ontario has, by far, the best system within Canada. Living in Saskatchewan, well, I frankly have more confidence in the health care system of Zambia, where I also lived for a time. It’s a weird mix of socialism (no second opinions!), Baptist morality (my wife was actually asked why she wanted a routine ultrasound and questioned upon what conditions she would terminate her pregnancy), incompetence (botched test results, nurses overriding medical procedures ordered by physicians), and negligence (Ativan is perfectly safe for the first trimester baby!).
It’s unfair to everyone that Canada is clustered all together, when incompetent provinces drag those numbers down.
Evertime I hear this quoted- that the US is anything but number one in national healthcare systems- I have to wonder about the judgement of most people. WHO puts these tables together by asking each country to fill out the statistics and takes them as reported without any effort to confirm. Therefore, when Uzbakistan reports a lower infant mortality than the US, WHO accepts that. Never mind that what the US calls a low birth weight infant (subject to many complications and high mortality) most of the world calls a stillbirth. In other words, these tables are not just worthless, but they are dangerously wrong. As an emergency physician of 32 years, I have cared for thousands of international people who have come to my ED from the airport. They vote with their feet. I know of people going abroad to have elective procedures done cheaper than in the US- all that government regulation does add much to the cost after all- but I never have heard of anyone who went outside the US for better healthcare. When elected officials and monarchs worldwide need medical care, they come to the US. It is expensive being number one. The first in technology, pharmaceuticals, etc comes with a big price tag.
When someone reads reports like the WHO put out, they must exercise a little common sense and ask a few questions rather than blindly accept ridiculous statements. Incidentally, this same rubbish was used to argue for a national healthcare reform that has become a shameful boondoggle.
The objective of the World Health Organization, as stated in their constitution, is health for all. They will “…take all necessary action to attain the objective of the Organization.” Since 1948 they have been working to socialize medicine worldwide.
Actually, I have friends from abroad who love their own country’s national healthcare better than USA, and even travel back home for better procedures, and at lower cost. According to Commonweath survey, the USA now leads the world in most medical errors and patient deaths, which after my own experiences, I am not surprised. In the future, if I need major surgery, I am seeking help outside the USA.
I’m from the UK and live in the states. The US health system is a nation wide scam and you’ve all fallen for it.
The reason why not many people leave the states for health care is simple: the nearby countries have worse care. This I suspect has shaped American ideas of just how good health care can be. I wouldn’t leave the states to go to Mexico for example.
Many counties have terrible socialized medicine, and many have great socialized medicine. The experiment has been done however, all the top health systems, not just by the metrics in this chart, are not mostly through private insurance companies.
You seem confused about three things:
1) Yes, many countries have socialized medicine and this is part of a vaguely more socialist view of the role of the state. Look at the data (not just from here of course), which thing is working better in general per dollar? What ever rational sounding argument can be given, the experiment has been done and repeated and the results are in. The name of the system is irrelevant, universal healthcare/socialize medicine doesn’t have to be a step towards any type of socialism in any other part of government. Nor is it part of any government take over. Americans seem less free than Europeans in many senses btw, for example I enjoy the freedom not to die from greed of an insurance company. It seems to me that you have simply fallen for scare tactics by people who only want to take your money by playing on your values.
2) Universal health care doesn’t at all remove the chance of private insurance if you want it. Bupa is a popular choice in the UK for private insurance and you can also pay for specific procedures if you prefer or the wait will be shorter. Many people do this and we really just get the best of both while still all paying much much less (a third on average I think).
3) In no sense do Americans get more “choice” about their doctors. Living in the US was my first experience of a doctor I couldn’t go to! Also, so what if you could choose if most people couldn’t afford all but the cheapest, that sort of choice is a total illusion. In France, the UK and Germany (these are the only ones I know, but I’m sure it’s true for many) you can choose your doctor freely, get second opinions and sue for any negligence (at much lower cost). Which doctors are “in plan” is way way more restrictive than the European system and if you don’t think it is, then just spend one year in France!
If I were ill, I’d instantly leave to get free and better care in Germany, the UK or France. I am so grateful that I’m an EU citizen and can do this after seeing both systems first hand. I can only imagine what living with the fear of instant bankruptcy caused by serious illness would be like and sitting in the doctors office after hearing half what you need isn’t ‘in plan’, that you have a massive bill and hearing the doctor you should be trusting trying to sell you product placements that you obviously don’t need.
Total. Obvious. Scam.
I see that Canadian healthcare is on a relatively high position in the WHO ranking. I am interested if the healthcare system in Canada is founded only on a private basis or it is a social healthcare system. Are the doctors and hospitals merchants under the laws of Canada or they are a part of the state apparatus? Are the doctors state (civil) servants or they are private persons/merchants? My personal opinion is that it is not ethic to commercialise the healthcare and to transform the healthcare into commercial activity. According me the state has to guarantee optimal health services in favour to its citizens. I am from Eastern Europe (Bulgaria) where the healthcare is just a commerce and the life of the patients is not appreciated at all. The doctors and the hospitals in Bulgaria are commercial entities. Some of them are commercial entities with state (public) share but this cannot change the commercial essence. There is a big corruption in the healthcare of my country and the quality of the service is at the lowest point. Many people die because of lack of therapy or bad and incorrect therapy. So can you describe in brief is the healthcare of Canada commerce or it is in the state dominated public sector?
Canada has universal health care which is socialized medicine. By way of legislation and regulations the government controls access to doctors and hospitals. Doctors are prohibited from setting their own prices and charging for medically necessary services. Patients are prohibited from paying doctors directly for medically necessary services. The government, as single-payer, decides the quantity and quality of medical services patients will receive. Certain individuals, groups and corporations are granted special privileges and benefits under socialized medicine.
I believe that every individual should have the freedom to pursue their own health care interests. I believe that every individual should have the freedom to spend their own money on their own health care.
The WHO 2000 study is a hilarious piece of data construction. I like how part of their data comes from health surveys passed out to WHO employees. Something that any statistician knows can completely contaminate the data.
People should really just stop using this study.
The WHO report ranking health systems was widely criticized – and I believe even the WHO acknowledged it was flawed. The Wall Street Journal reported “Few people who cite the ranking are aware that some public-health officials were skeptical of the report from the outset. The ranking was faulted because it judges health-care systems for problems — cultural, behavioral, economic — that aren’t controlled by health care.” This is true.
Both domestic and international evidence shows that parallel private systems cause longer wait times for patients in the public queue – because doctors have higher incentives to treat patients paying more in private clinics than the fees medical associations negotiate with public payers. Access to care in the private sector is based on ability to pay rather than need.
Canada’s public system has challenges, especially in regard to non-hospital and non-physician services which are too costly for many people. And wait times for some services are too long. However a study in Alberta found that nearly 30% of the patients on wait lists for knee and hip replacements were no longer waiting – many had already had the surgery or had been able to address their problems with alternative treatments (eg., physiotherapy). The point here is that surgeons are not known to be good wait list managers. They have an obligation to refer patients who may want faster access to another surgeon but seldom do. And patients often don’t exercise the options available to them in the public system – for example, asking to see another surgeon.
The wait list is a good issue to stir people’s sense of injustice but unfortunately the “solutions” identified by groups like the Fraser Institute and CIMCA lead us over a cliff. These are not “government wait lists” – they are the doctors’ wait lists.
Access to medical care in the public system is not based on need. Which patients on surgical waiting lists don’t need surgery? Who decides need in the public health care system? Under a single-payer system the government controls the doctor/patient relationship. Politicians and bureaucrats decide how many surgeries will be performed annually, how many OR hours will be allocated to each doctors, etc. Waiting lists are wrong. Preventing people from paying for their own health care needs is wrong.
You are forgetting to list TAIWAN which has an excellent healthcare system, much better than most of the top 10 countries of your list. Or is it that out of ignorance you included in the Chinese’s system?
The rankings are more than just socialized vs non-socialized medicine. The type of medicine practiced has a huge factor into this. If people are not going to the doctor because they are in a state of wellness, then you are not burdening the system.
Fact is, any health care system will work just fine if its funded appropriately. Socialized medicine comes down to how much the government allocates and how efficient they are. It could work just fine, however, most governments really don’t care about the citizen.
Some of the countries which rank higher than the USA use different remedies to treat ailments and their perspective on health is much different. France, the largest consumer of homeopathy, ranks 1st. The Netherlands, where 45% of the practicing physicians believe in homeopathy, ranks 17th. Some of these places use natural therapies which work to strengthen and tonify the body rather than suppress symptoms.
The philsophy of what disease is and how to treat it play a greater role in the ranking than whether or not socialized medicine is best. Also, the system in the USA would just fine if Big Pharma wasn’t involved and people were ethical.
Of course the quality, technologies, facilities and skills are far below France (we’re ranked 92nd), but this system has gotten better over the years. I hope my country will be on top 5 by 2030 for the sake of the people.
yea, im sure with 4 bucks a month your healthcare will be better than the top 5 in 2030 hahahaha
also, you said the words, “free healthcare coverage by paying…” i hope you see the flaw in this…
For being a french living in USA
so over all i have a bit bigger paycheck in USA but
– bad retirement
– bad medical coverage
– college to pay for the kids
=> if you are single and get a degree you benefit living in USA
if you have kids and a wife you are better in France.
I am trying to write an article about this for a class/my blog.
Could you tell me how much, if anything, you have to pay to go to the emergency room (in different countries) as well as how much it costs to take an ambulance?
Thank you so much for the help
The profit motive is what I say on television Hawking a new drug every other commercial. The maddening thing is that it’s like junk mail because every once in awhile you get a check so you have to go through the letters and the vast majority of it is just trying to take your money.
There are and will be incredible medical breakthroughs in the next years to come but in the US only the folks that can afford it will be able to have good health.
Here’s a REAL representation of healthcare in Canada (Toronto, Ontario). I’m going to try to be as brief as possible while considering points that others have made:
Shawn & others of a similar mindset:
If you are a Canadian citizen, health care is provided at “no cost” (taxes cover it). As well, you DO have many options to increase / modify the level of care you receive. This is done primarily by paying private insurance companies or taking part in a benefit program through your employer.
As an Ontario resident, OHIP covers most of my (and all Ontarians) medical needs, and my employer covers all of my family’s basic (non-emergency) health and dental needs, even when we travel abroad. To give you some real, personal examples of the coverage:
From OHIP (Province of Ontario health care within Canada – for those who don’t know):
– I had kidney surgery and treatment for 1.5 YRS – at no out of pocket cost (This would cost hundreds of thousands in the US – true). Treatment was successful and I’m better now.
– I’ve had 5 broken bones and about 100 stitches over the years – at no cost.
– I’ve been to the ER many times and treated for everything from vomiting to systemic infections – at no cost.
The fact is, in most situations, if you go to a hospital or even a walk-in clinic, they will treat you at “no cost”, however they will also PRIORITIZE the necessity of your treatment. If you show up to the ER with a leg cramp while there are people being treated for gunshot wounds, yes, you will have to wait. You WILL be treated though and again, it wont cost you anything directly (taxes) – even if it requires months in the hospital for you to get better.
I don’t understand how some people can complain about a system that provides top-level care without bankrupting families. Do those that don’t appreciate this know what it can be like without it? Many of you commenters come across as seeming very entitled without justification.
If you want to be more financially responsible for your family’s healthcare, then pay a private insurer a premium amount and you will be treated similarly to those in the US.
If you are unsatisfied and unwilling to try to contribute to Canadian society and rights of citizenship – leave.
In this GREAT country, even the homeless get the same level of care if in need. It doesn’t matter about your status, you are treated equally whether or not you have insurance backing you. It’s a lot more “doing what’s right and preserving humanity” than “let’s save a life only if we can make a buck”.
Lastly, prescriptions are generally not covered by the Gov., but medication and diagnosis while in the hospital is typically completely covered (anesthetic, pain meds, MRIs, etc…), and employer benefits almost always cover a large percentage (80%+) of prescribed medication and most other things.
If you are an Injured Worker, it is a VERY DIFFENENT SITUATION.
Many go Bankrupt, Families are Broken, they go homeless, and some commit suicide- because the WCB System is run by Employers.
The World Health Organization Global Benchmarking Tool an Instrument to Strengthen Medical Products Regulation and Promote Universal Health Coverage
National regulatory authorities (NRAs) are the gatekeepers of the supply chain of medical products, and they have a mandate to ensure the quality, safety and efficacy of medicines, vaccines, blood, and blood products, medical devices, including diagnostics and traditional, or herbal medicines. However, the majority of the world’s regulators are still struggling to reach a level of maturity, whereby they have a stable, well-functioning and integrated regulatory system. The World Health Organization (WHO) has developed a Global Benchmarking Tool (GBT) as part of its five-step capacity building program to assist NRAs, using the tool, they can benchmark their own strengths and areas of weakness, and then engage in a formal benchmarking process together with WHO and international experts in order to formulate an effective and workable institutional development plan. The GBT is comprehensive across the entire product life cycle and allows benchmarking to be customized to the needs of the NRA. It has evolved from decades of experience using a variety of benchmarking tools, within WHO and other stakeholder organizations. By the end of December 2019, 26 countries had undergone formal benchmarking, and a further 54 countries had used the GBT to conduct self-benchmarking exercises assisted by WHO.
Introduction
National regulatory authorities (NRAs) are the gatekeepers of the supply chain of medical products, and they have a mandate to ensure the quality, safety and efficacy of medicines, vaccines, blood and blood products, medical devices, including diagnostics, and traditional or herbal medicines. They work within a legal framework and set of regulatory functions spanning the medical product lifecycle, from clinical trial oversight, product marketing authorization and registration, licensing establishments, regulatory inspections, testing products, post-marketing surveillance, and vigilance activities.
When a national regulatory system is independent, efficient, science based transparent, and well-managed, it supports robust and effective medical products regulation, and medicines and other health technologies entering the market are safe, efficacious, and of assured quality. This in turn protects the population from harm due to unregulated supplies, including substandard and falsified medical products, and thus fosters confidence in the health care delivery system. A well-functioning NRA creates an environment in which medical products are appropriately manufactured, stored, distributed, and dispensed. It ensures that health professionals and patients are in a position to use medical products rationally because they have the information they need to do so, and ensures promotion and advertising is fair and balanced. It supports local production of medical products, which is key to affordability, helps create a transparent, and well-organized market for pharmaceuticals and other medical products, and enables post-marketing surveillance and integrity of the supply chain. All these facets of regulation help ensure timely access to essential medicines and enable NRAs to be prepared for better response to emergencies. Moreover, at its best, a strong NRA will perform all of these functions without creating an unnecessary regulatory burden on itself and any of the stakeholders.
As the value chain for medical products is becoming increasingly globalized, a weakness in one part of the supply chain can have adverse consequences for patients thousands of miles away. In pharmaceuticals manufacturing, for example, active pharmaceutical ingredients may be sourced from multiple countries and used for medicines production in another, before being globally distributed. A secure supply chain can be an important enabler to reduce the problem of substandard and falsified medical products.
An efficient and reliable regulatory system is also a key component of the WHO prequalification program for vaccines, as the NRA assessing providing oversight of a product applying for prequalification must be operating at an acceptable level of maturity (1). Overall, effective regulatory systems are an essential component of health systems and contribute significantly to universal health coverage.
A Lack of Mature Regulatory Agencies
However, many countries still lack this basic building block of a well-functioning health system. According to the World Health Organization (WHO) regulatory systems strengthening database, among its 194 Member States, only 50 countries (26%) have what are considered to be mature regulatory agencies (the top or second-highest level of maturity), whilst 144 countries have suboptimal regulatory systems. Just over half, 51% (99 countries) are at the lowest level of maturity, whilst 23% (45 countries) are at the second lowest level of maturity. Although not all countries were benchmarked against WHO GBT, but the maturity level status of remaining countries have been estimated based on previous assessments done by WHO using other tools or being a Stringent Regulatory Authority (SRA). In these countries, when manufacturers of medical products want to bring their products to market, they face a landscape of disparate regulations, unclear regulatory pathways, frequent delays in accessing essential medicines and limited transparency. This suppresses innovation, drives up medicine prices and opens the door for substandard and falsified medical products. It also leaves regulators ill-prepared to deal with public health emergencies, where, for example a vaccine or medicine may need to be fast-tracked through the regulation process.
In many low- and middle-income countries, regulatory systems strengthening can be extremely challenging. NRAs are often overburdened and under-staffed, with fragmented structures or insufficient legal frameworks systems which may be difficult to reform. The first step–knowing the current state of the regulatory system where the weaknesses and gaps lie and how to go about addressing them–can be a critical task.
World Health Assembly Resolution WHA67.20 on regulatory system strengthening was adopted in May 2014 (2). This Resolution emphasized the WHO mandate and requested both WHO and Member States of low- and middle-income countries to invest more in this area and to address all health products and technologies.
The WHO Global Benchmarking Tool
WHO supports its Member States in strengthening their regulatory systems for medical products by setting norms and standards, promoting smart regulation, identifying strengths and gaps, providing specialized technical assistance, and capacity building opportunities and advising them on issues related to quality assurance of medicines for national and international markets.
In 1997, WHO began benchmarking regulatory systems as part of its regulatory system strengthening program, initially using a set of indicators designed to evaluate regulatory oversight for vaccines. This was to address the pressing challenge of how to ensure that vaccines meet the appropriate standards of quality, safety and efficacy, whether they were used domestically in the country of manufacture, or in receiving countries. Later on, WHO expanded this programme to evaluate regulatory oversight for medicines, blood and blood products and medical devices. In 2013, WHO started to unify these parallel programs and integrate various tools developed in this regard through the development of a harmonized tool, the Global Benchmarking Tool (GBT), representing the primary means by which the WHO objectively evaluates regulatory systems (3).
The creation of the GBT also came at a time when other tools were being developed and used, including one by the Pan-American Health Organization (PAHO), as well as other non-UN agencies. The concurrent development of a plethora of tools was confusing and burdensome for NRAs and individuals responsible for using them. There were overlaps between the tools, and they had similar regulatory requirements. Unification of the WHO vaccine, medicine and broader PAHO tool, and alignment with non-WHO tools underpinned the creation of the GBT (4).
The GBT enables regulatory authorities to self-evaluate their own strengths and areas for improvement; facilitates the formulation of an institutional development plan to build upon strengths and address the identified gaps and prioritizes interventions; and facilitates the monitoring of progress and achievements. It helps countries to develop strong legal foundations and political leadership to underpin a regulatory system with a clear focus on patient safety and transparency in decision-making; and to identify and develop a core set of regulatory functions to meet country and regional needs.
The GBT evolved through a process of wide and deep consultation with WHO Member States and other stakeholders, and piloting in different regulatory settings. The consultation conducted through four face-to-face meetings and many hours of virtual discussions as well as a public consultation on the draft tool to solicit comments from a wide range of Member States and stakeholders and incorporating them into the current version. The GBT was field-tested in 2018 and the first use of the current version were conducted in March and April 2019 in Ghana and El Salvador, respectively.
One of the significant additions to the latest version of the tool, GBT Rev VI, is benchmarking modules that look at the NRA’s ability to tackle the problem of substandard and falsified medical products. This is covered under several modules of the tool including the national regulatory system, market surveillance, and laboratory testing, as well as regulatory inspection, and marketing authorization The latest revision of the tool also promotes other principles of Good Regulatory Practices, including legality, impartiality, consistency, proportionality, flexibility, effectiveness, efficiency, clarity, and transparency as well as the need for implementation of risk and quality management in regulatory systems, and regulatory preparedness to face emergencies (5). Several sub indicators in the tool look at the NRA capacity and preparedness for managing emergencies.
The WHO Regulatory Systems Strengthening programme, which aims to strengthen capacity of regional, sub-regional and national regulatory systems, works with countries to apply the GBT, as part of a five-step approach to improvement and NRA capacity building, with priority given to regulatory systems strengthening for developing countries (Figure 1).
Figure 1. WHO five-step approach to national regulatory agency capacity building.
Structure of the Global Benchmarking Tool
The GBT is divided into four levels: (1) national regulatory system and regulatory functions; (2) indicators, (3) sub-indicators, and (4) fact sheets. In addition to the national regulatory system component that provides the framework, there are eight core regulatory functions, which between them cover the whole product life cycle of medical products (6). Core functions are agreed during the consultation process with the NRA include the following:
Registration and Marketing Authorization
Marketing authorizations (also known as product licensing or registration) are the procedures for approval of a medical product for marketing after it has been evaluated for safety, efficacy, and quality of the product, and the appropriateness of the product information (7).
Vigilance
Vigilance is the science and activities relating to the detection, assessment, understanding, and prevention of adverse effects or any other medical product-related problems (8).
Market Surveillance and Control
An NRA’s market surveillance and control function activities are primarily concerned with control of import activities, prevention, detection, and response to substandard and falsified medical products, quality monitoring throughout the supply chain, and control of promotional, marketing, and advertising activities (9).
Licensing Establishments
The NRA is responsible for ensuring that all establishments throughout the medical products supply chain are licensed to undertake the respective activities (e.g., manufacturing, distribution, wholesale, retail) (10).
Regulatory Inspection
Regulatory inspections ensure that operations are carried out in accordance with approved standards, norms, and guidelines and are in compliance with the national medical products legislation and regulations. These, in turn, should be consistent with WHO recommendations and other internationally recognized guidelines (11).
Laboratory Testing
The laboratory testing regulatory function is intended to ensure that the National Regulatory Authority (NRA) is able to assess the quality of medical products by performing quality tests when needed (12).
Clinical Trials Oversight
Clinical trials oversight is aimed at protecting the safety and rights of humans participating in clinical trials, ensuring that trials are adequately designed to meet scientifically sound objectives, and preventing any potential fraud, and falsification of data (13).
National Regulatory Authority Lot Release
Lot release (also called official authority batch release) is a non-common regulatory function that does not apply to all medical products. Rather, it applies only to some specific products (e.g., vaccines) (14).
Within each regulatory function, the GBT uses a set of indicators, each with their own sub-indicators. For the sake of structural consistency across the regulatory functions and to assist benchmarking or one or more specific theme across the functions, the GBT indicators are categorized into nine categories:
1. legal provisions, regulations, and guidelines
2. organization and governance
3. policy and strategic planning
4. leadership and crisis management
5. transparency, accountability, and communication
6. quality and risk management system
7. regulatory process
8. resources (human, financial infrastructure, equipment, and information management system)
9. monitoring progress and assessing impact.
Fact sheets for each sub-indicator provide further details and clarify the scope of each sub-indicator, and there are also indicators for input, process and output. This can bring more consistency and quality to process and outcome of benchmarking. There are 268 sub-indicators in total. A four-tier scoring system measures the level of implementation and monitors the progress of each sub-indicator. The rating scale of each single sub-indicator ranges from not implemented, ongoing implementation, partially implemented, and fully implemented.
By walking through this methodical, step-wise benchmarking process, first through pre-visit of the NRA followed by self-benchmarking and subsequently through WHO formal benchmarking by an international team of experienced assessors, assembled and trained by WHO, it is possible to clearly understand the capacity of the system and the level of maturity an NRA has already reached, and from that formulate an institutional development plan to address areas for improvement and enhancing regulatory capacity of Member State.
The four performance maturity levels were adopted from the International Standard ISO 9004 (Quality management—Quality of an organization –Guidance to achieve sustained success) and are an expression of the extent to which a regulatory system has been formalized as stable, well-functioning and integrated (Figure 2). In a Level 1 NRA, some elements of regulatory system exist, whilst a Level 2 NRA will be an evolving national regulatory system that partially performs essential regulatory functions. Level 3 represents the minimum target for most NRAs to reach: a stable, well-functioning and integrated regulatory system. Level 4 NRAs exceed this required standard, and represent a regulatory system operating at advanced level of performance and continuous improvement. It is worth mentioning that the overall maturity level of a system, calculated based on the lowest maturity level of individual regulatory functions. For example, if a regulatory system is scored for all functions as ML 3 and only one function is scored as ML 2 then the overall maturity level of the regulatory system will be calculated as ML2. However, as there are many different models of regulatory systems that can fit the purpose at national level, the tool, scoring system, and methodology are adapted with some flexibility to accommodate these differences.
Figure 2. WHO global benchmarking tool performance maturity levels. Source: World health Organization.
Countries requesting assistance from WHO to benchmark their regulatory system using the GBT all follow a clear process, from planning and pre-screening, including a pre-visit mapping of the regulatory system (Figure 3). Self-benchmarking is then validated ahead of the formal benchmarking process, which can include enhanced performance evaluation of specific regulatory functions, for example observed audit for evaluation of regulatory inspection function, and vigilance field visits for evaluation of vigilance function (15).
Figure 3. Benchmarking process.
In addition to the GBT itself, WHO maintains a database of reports and IDPs of the NRAs that have been benchmarked against the GBT and this is supported by a computerized platform to facilitate the benchmarking, including the calculation of maturity levels (16). The computerized GBT (cGBT) is available upon request to Member States and organizations working with the WHO under the Coalition of Interested Parties. From January 2016 to December 2019, 26 countries underwent formal benchmarking (including Tanzania, see box 1), and 54 countries used the GBT to conduct self-benchmarking exercises (Figure 4).
Figure 4. Countries/areas targeted for WHO regulatory system strengthening program and benchmarked against GBT indicators, January 2016- September 2019.
Tanzania’s Milestone Achievement a First for Africa
In December 2018, Tanzania became the first confirmed country in Africa to achieve a well-functioning, regulatory system for medical products. The Tanzania Food and Drug authority made considerable improvements in recent years in ensuring medicines in the healthcare system are of good quality, safe and produce the intended health benefit.
WHO’s assessment of the Tanzania Food and Drug authority was based on its Global Benchmarking Tool, which evaluated regulatory functions against a set of 251sub-indicators, such as product authorization, market surveillance and the detection of potential adverse-effects, to establish their level of maturity. One regulatory function namely “NRA lot release” was not assessed during the benchmarking of Tanzanian NRA given the scope of the benchmarking which was limited to medicines and imported vaccines.
The benchmarking of Tanzanian regulatory authorities was carried out in phases by a WHO-led team of international experts. During the first and second quarter of 2018, WHO facilitated self-assessments and conducted a formal evaluation of the Tanzania Food and Drug Authority on the mainland and the Zanzibar Food and Drug Agency and required the regulatory authorities to make a number of adjustments. In the last assessment, Tanzania FDA met all indicators that define a maturity level 3 agency, the second highest on WHO’s scale and the target for regulatory systems globally.
Looking Ahead
The integration of blood and blood products into the GBT has been completed by the end of 2019, and work on integrating medical devices (including diagnostics) into the GBT is still ongoing. Once the integration process is completed, the tool will be known as GBT plus. WHO intends to use Revision VI of the GBT to evaluate and publicly designate national regulatory authorities as WHO-Listed Authorities (WLAs) that have been objectively documented to perform at Maturity Level 3 or 4. A concept note presenting a proposed framework for using the GBT to generate and analyze evidence of regulatory system performance, and to allow for the public listing of regulatory authorities as WLAs, has been made available for public consultation in May 2019. As a result of aforementioned consultation, a policy document was developed and posted for public consultation in December 2019.
Author Contributions
All authors were involved in developing the concept and methodology as well as drafting and editing the manuscript. All authors developed the figures.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors appreciate the assistance of many WHO colleges, experts from member states, donor community, and technical partners who contributed into development of the Global Benchmarking Tool. Considering the long list of contributors, the authors are not mentioning the name of any individuals.
References
1. Dellepiane N, Wood D. Twenty-five years of the WHO vaccines prequalification programme (1987-2012): Lessons learned and future perspectives. Vaccine. (2015) 33:52–61. doi: 10.1016/j.vaccine.2013.11.066
2. Sixty-seventh World Health Assembly. WHA 67.20: Regulatory Systems Strengthening for Medical Products. Geneva: World Health Organization (2014).
3. Regulatory system strengthening. World Health Organization. Available online at: https://www.who.int/medicines/regulation/rss/en/ (accessed October 4, 2019).
4. World Health Organization. Essential Medicines and Health Products. Assessing National Medicines Regulatory Systems. Available online at: https://www.who.int/medicines/areas/quality_safety/regulation_legislation/assesment/en/ (accessed July 19, 2019).
5. Good Regulatory Practices: Guidelines for National Regulatory Authorities for Medical Products. Geneva: World Health Organization (2016). Available online at: https://www.who.int/medicines/areas/quality_safety/quality_assurance/GoodRegulatory_PracticesPublicConsult.pdf (accessed October 22, 2019).
6. WHO. Global Benchmarking Tool (GBT) for Evaluation of National Regulatory System of Medical Products National Regulatory System (RS): Indicators and Fact Sheets Revision VI version. (2018). Available online at: https://www.who.int/medicines/areas/regulation/01_GBT_RS_RevVI.pdf?ua=1 (accessed July 28, 2019).
7. WHO. Global Benchmarking Tool (GBT) for Evaluation of National Regulatory System of Medical Products Registration and Marketing Authorization (MA): Indicators and Fact Sheets Revision VI Version. (2018). Available online at: https://www.who.int/medicines/regulation/02_GBT_MA_RevVI.pdf?ua=1 (accessed July 28, 2019).
8. WHO. Global Benchmarking Tool (GBT) for Evaluation of National Regulatory System of Medical Products Vigilance (VL): Indicators and Fact Sheets Revision VI version. (2018). Available online at: https://www.who.int/medicines/regulation/03_GBT_VL_RevVI.pdf?ua=1 (accessed July 28, 2019).
9. WHO. Global Benchmarking Tool (GBT) for Evaluation of National Regulatory System of Medical Products Market Surveillance and Control (MC): Indicators and Fact Sheets Revision VI Version. (2018). Available online at: https://www.who.int/medicines/regulation/04_GBT_MC_RevVI.pdf?ua=1 (accessed July 28, 2019).
10. WHO. Global Benchmarking Tool (GBT) for Evaluation of National Regulatory System of Medical Products Licensing Establishments (LI): Indicators and Fact Sheets Revision VI Version. (2018). Available online at: https://www.who.int/gho/medicines/regulation/05_GBT_LI_RevVI.pdf?ua=1 (accessed July 28, 2019).
11. WHO. Global Benchmarking Tool (GBT) for Evaluation of National Regulatory System of Medical Products Regulatory Inspection (RI): Indicators and Fact Sheets Revision VI Version. (2018). Available online at: https://www.who.int/medicines/regulation/06_GBT_RI_RevVI.pdf?ua=1 (accessed July 28, 2019).
12. WHO. Global Benchmarking Tool (GBT) for Evaluation of National Regulatory System of Medical Products Laboratory Testing (LT): Indicators and Fact Sheets Revision VI Version. (2018). Available online at: https://www.who.int/medicines/regulation/07_GBT_LA_RevVI.pdf?ua=1 (accessed July 28, 2019).
13. WHO. Global Benchmarking Tool (GBT) for Evaluation of National Regulatory System of Medical Products Clinical Trials Oversight (CT): Indicators and Fact Sheets Revision VI Version. (2018). Available online at: https://www.who.int/medicines/regulation/08_GBT_CT_RevVI.pdf?ua=1 (accessed July 28, 2019).
14. WHO. Global Benchmarking Tool (GBT) for Evaluation of National Regulatory System of Medical Products NRA Lot Release (LR): Indicators and Fact Sheets Revision VI Version. (2018). Available online at: https://www.who.int/medicines/regulation/09_GBT_LR_RevVI.pdf?ua=1 (accessed July 28, 2019).
15. World Health Organization. Manual for Benchmarking of the National Regulatory System of Medical Products, Draft Version 2. Geneva: World Health Organization (2019).
16. WHO. Regulatory Systems Strengthening Database. Geneva: World Health Organization.
Keywords: global benchmarking tool, GBT, regulatory systems strengthening, regulation, regulation of medical products, national regulatory authority, RSS, NRA
Citation: Khadem Broojerdi A, Baran Sillo H, Ostad Ali Dehaghi R, Ward M, Refaat M and Parry J (2020) The World Health Organization Global Benchmarking Tool an Instrument to Strengthen Medical Products Regulation and Promote Universal Health Coverage. Front. Med. 7:457. doi: 10.3389/fmed.2020.00457
Received: 19 April 2020; Accepted: 09 July 2020;
Published: 19 August 2020.
Hilde Stevens, Université Libre de Bruxelles, Belgium
Lise Aagaard, Independent Researcher, Copenhagen, Denmark
Lawrence Liberti, Centre for Innovation in Regulatory Science, United Kingdom
Copyright © 2020 Khadem Broojerdi, Baran Sillo, Ostad Ali Dehaghi, Ward, Refaat and Parry. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
The World Health Organization
A History
This book has been cited by the following publications. This list is generated based on data provided by CrossRef.
Email your librarian or administrator to recommend adding this book to your organisation’s collection.
Book description
According to its Constitution, the mission of the World Health Organization (WHO) was nothing less than the ‘attainment by all peoples of the highest possible level of health’ without distinction of race, religion, political belief, economic status, or social condition. But how consistently and how well has the WHO pursued this mission since 1946? This comprehensive and engaging new history explores these questions by looking at its origins and its institutional antecedents, while also considering its contemporary and future roles. It examines how the WHO was shaped by the particular environments of the postwar period and the Cold War, the relative influence of the US and other approaches to healthcare, and its place alongside sometimes competing international bodies such as UNICEF, the World Bank, and the Gates Foundation. The authors re-evaluate the relative success and failure of critical WHO campaigns, from early malaria and smallpox eradication programs to struggles with Ebola today.
Reviews
‘Finally, an up-to-date history of the World Health Organization. This deft account spans the institution’s aspirational post-World War II beginnings, the tensions and turnarounds of the Cold War period, and the embattled contemporary era of private encroachment on WHO turf. The authors bring together the contentious politics, personae, and programs through a grand narrative and little-known inside stories.’
‘This long-awaited volume by three distinguished historians of public health, does not disappoint. Though the general lines of this history are familiar, this extensively researched, clearly written volume greatly enriches this history, providing new details on nearly every page, and situating the WHO within the wider history of global political change.’
‘… the authors are to be congratulated, not only for presenting us with this splendid, up-to-date and excellently contextualized history of the WHO, which constitutes a reference work about this international agency; but also for inviting us to engage in a historical reflection, and for drawing lessons from this history to be applied to the present and future of the mission of the WHO.’
María‑Isabel Porras‑Gallo Source: Metascience
What is The World Health Organization (WHO)?
The flag of the World Health Organization.
I. Relevance of the WHO
The World Health Organization has a special holiday celebrated the world over on April 7, which serves as a testament to its successful leadership as a steward working for global health. It is also a day when people and nations take a single health issue and find ways to protect people from its health threats. The organization respects all individuals’ freedoms, and also their governments’ responsibilities to protect earth’s citizens from health hazards and diseases by working to provide safe water and ensure clean air.
The World Health Organization’s relevance continues into the 21 st Century, with its hope and driven dedication being to promote and help people attain the highest possible level of health in the world today and into the future. The organization has defined its objectives under its constitution as being at the forefront of major international health-related initiatives. It also further states that, whenever and wherever health is threatened, it would be there to restore the people’s well being.
The WHO is bent on providing leadership in accomplishing good health all over the globe, doing so in partnership and cooperation with other organizations in its duty to ensure the continued overall good health of all the world’s people. Over time, the organization has come to know what avenues it has to take to continually be of service in improving the health of the global population. The objective of the organization for this, set forth in Millennium Development Goals (MDGs), is to act in cooperation with its member countries, and synchronize its actions with other concerned countries and agencies in the international health system.
II. History of the World Health Organization
The year 1851 saw the conceptualization of the idea ( and for a need) to establish a World Health Organization. However, this concept did not firmly take root until almost a century later, after the Second World War. Prior to the organization’s formation, it’s constitution was signed by 61 UN member countries on July 22,1946, establishing its headquarters in Geneva, Switzerland. The World Health Organization is under the World Health Assembly, and its yearly meetings take place in Geneva every May. Its Director General is appointed to a five-year term, and its executive board is composed of 34 members each serving on a three-year term. The current leader of the WHO is Director General Margaret Chan.
On April 7, 1948, the United Nations Development Group formalized the creation of the World Health Organization. The new organization then took under its wings two UN health agencies. Namely, these were the League of Nations Health Organization and the Office International d’Hygiene Publique. The WHO was created to take care of the world’s health problems, and it has 194 member states that also belong to the United Nations. One of its first concerns was the eradication of small pox.
The organization also publishes the World Health Report, the Worldwide Health Survey, and World Health Day. These health reports were first published in 1995, and continue to give member countries updates on information that influences each country’s funding and health policies. On a wider scope, the published data and information on health are also available to the public, including everyday citizens, journalists, research institutions, and universities alike. The topics and themes also vary for every issue, from health system financing for health care, to health security and mental health. Notably, one published research on those persons over 50 years old, in its “Study on Global Ageing and Adult Health”. The survey involved 50,000 people in 23 countries.
The World Health Organization also started an online database on people with mental disabilities, with the aim of eradicating human rights abuses toward this group of people. It is called MiNDbank (just as it is spelled), and it went live on the World Wide Web on Human Rights Day. The website and database contains varied information regarding human rights, mental disability, substance abuse, and other relevant topics. It also has information about the laws in many countries regarding policies, strategies, and service standards for people with these conditions.
Today, the WHO is a specialized agency concerned with finding ways to stop infectious diseases, such as Ebola, malaria, HIV/AIDS, and tuberculosis. Some of the successful programs run by the WHO were the inoculation drive for tuberculosis (1950), that for the eradication of malaria (1955), and the first global look at diabetes mellitus. The organization also spawned the International Agency for Research on Cancer in 1965. In 1979, the WHO declared the total eradication of small pox. Then, in 1998, infant survival increased and life expectancy increased, and was defined as such by the organization as well.
III. Main Functions of the WHO
The World Health Organization has made its purpose known from the first day of its creation. However, every year or so, its main agenda may see changes, adjusted accordingly to the transforming health needs of the world. Its many functions are a result of careful analyses of the organization’s leadership roles on the international stage. That it always maintains a neutral stand, and honors its universal membership as well, are just as important as its well-known convening power. The Eleventh General Program of Work 2006-2015 defines the six main functions of the organization, and these are listed immediately below.
1. Acts as leader on matters important to health and cooperates with other countries.
2. Creates the research agenda and follows the generation, translation, and dissemination of important knowledge.
3. Creating norms and standards and implementing their promotion and monitoring as well.
4. Explaining ethical and evidence-based policy options.
5. Giving technical assistance, catalyzing change, and creating sustainable institutional capacity.
6. Watching over the health conditions and addressing the health trends.
Millennium Development Goals
In September of 2000, the United Nations’ 191 member countries also set goals for 2015 under the banner of ‘Millennium Development Goals’. These continuing goals are:
1. To stop poverty and famines.
2. To implement universal primary education.
3. To make gender equality a reality and give women responsibility.
4. To improve child survival.
5. To improve the mothers’ health.
6. To fight malaria, HIV/AIDS, and other illnesses.
7. To help in protection of the environment.
8. To foster cooperation between countries in development.
There is no question that all 191 member countries support the Millennium Development Goals. The Association of Southeast Asian Nations (ASEAN) and the European Union (EU) have both reshaped their own respective policies and workings around the larger demands of the MDGs. The OXFAM and Red Cross are two other international charities that have focused their aims on helping to achieve the MDGs. There are many more civil society organizations that are in the international, regional, and local levels that have adopted these very same MDGs as well.
IV. Controversies & Setbacks
The World Health Organization is a United Nations agency that promotes and gives healthcare for people that need them around the world. It has made many achievements, and garnered accolades on the international scene. Still, especially lately, it has been criticized for financial mismanagement, as well as partisan politicking.
One of the major accusations that seems to be persistent is the issue relating to the appointments of those in key positions in the organization. Many feel that political patronage factors too much into the choice of these appointees. In 1993, the cause of criticism was vote buying in the election of its Director General, which is a crucial position inside the organization that would be responsible for guiding the WHOs objectives and policies into the next century. Thus, many member countries were concerned about the WHO’s processes and integrity.
There have also been the failures to reach stated goals, such as the failures to eradicate Malaria, Cholera, Diarrhea, and Tuberculosis. These problematic areas have been subsequently addressed, though still seem to be major obstacles to hurdle yet. Tuberculosis has sprung back due to resistance caused by the overuse of antibiotics. The WHO then started a new TB plan to follow up the original initiative. Diarrhea also remains as killers of children and adults in most developing countries in the world today.
The many failures to achieve health goals in the past have been directed to the organization as being caused by its bureaucratic nature and internal politicking. History shows that, in the 10 years that Dr. Hiroshi Nakajima was Director General of the World Health Organization, he was accused both internally and externally of such mismanagement. Dr. Nakajima was accused of lacking in communication abilities, and further allegations pointed to his autocratic and bureaucratic behavior inside the organization. He was also accused as employing vote-buying techniques. Although he was re-elected to the post again, the initial confidence he enjoyed with many major Western countries rapidly went sour.
As disbelief and loss of confidence grew from the major donors, increasingly their donations failed to materialize as well. Many of the WHO’s projects were under tight budget constraints, which ultimately led to the creation of another UN agency to handle an international AIDS program. The transfer began the deterioration of the WHO’s role as a major leader in world health affairs, as other UN agencies were tasked to take similar roles thereafter as well. However, today the World Health Organization has taken on new challenges under new leadership for the 21 st Century. Hopefully, it can regain confidence and remain on course in reaching it most important objective: ensuring and promoting better health for all.
The World Health Organization and Pandemic Politics
The good, the bad, and an ugly future for global health
From the start, the World Health Organization (WHO) has been at the center of the COVID-19 storm—and the target of criticism. The pandemic and the controversies associated with it have created an immediate crisis for WHO as COVID-19 rages on. But it’s also created a prospective crisis because the outbreak and political reactions to it will shape the future of WHO. The present back-and-forth between WHO’s critics and defenders previews the coming tussle over how to repair global health governance and reform WHO in light of this disaster. Although the pandemic is not over, the pillory and praise of WHO are worth exploring now so that the coming tsunami of demands for change do not destroy the organization in order to save it.
WHO and the COVID-19 Pandemic
Much of the criticism of WHO asserts that it failed to exercise global health leadership and instead became a tool of Chinese politics, power, and propaganda. This critique holds that WHO had the ability to question China’s handling of the outbreak in Wuhan so that the organization could better prepare the world for a dangerous disease—but that WHO failed to act decisively. The criticism raises questions about WHO’s authority to challenge states during serious outbreaks for the good of global health. In contrast, praise for WHO often highlights how it has its deployed scientific skills, epidemiological expertise, medical know-how, outbreak-response capacities, and global networks in helping China and other countries. These commendations emphasize the imperative for WHO to work with governments in battling outbreaks.
In essence, WHO’s critics and defenders are talking past each other. But both perspectives are core to the International Health Regulations (IHR), the leading international agreement on infectious diseases and other serious disease events adopted by WHO member states in 2005.
Deploying these capabilities tends not to generate political problems because the focus is on fighting outbreaks
The IHR’s success depends on WHO using its scientific, medical, and public health capabilities to help countries prevent, protect against, and respond to disease events. Deploying these capabilities tends not to generate political problems because the focus is on fighting outbreaks with measures based in science, medicine, and public health. This pattern appears again in the COVID-19 pandemic. WHO’s efforts to advance development of coronavirus vaccines and therapeutics have not generated acrimony. The organization’s sharing of information and its attempts to counter online misinformation and disinformation have earned widespread praise. The medical and public health expertise that WHO can offer countries to combat COVID-19 is appreciated. Its warnings about the pandemic’s threat to low-income countries are acknowledged as important.
Authority of the World Health Organization to Take Action
International Health Regulations grant the ability to challenge how governments exercise sovereignty
Claims that WHO turned a blind eye to China’s dissembling about its outbreak suggest that WHO failed to act on information it had from other sources
Criticism of WHO during the COVID-19 pandemic has emerged exactly in the context of these authorities. Claims that WHO turned a blind eye to China’s dissembling about its outbreak suggest that WHO failed to act on information it had from other sources, including the failure to share that information with other countries. Critics pilloried WHO Director-General Tedros Adhanom Ghebreyesus for declaring the COVID-19 outbreak in China a public health emergency of international concern at a time and in a manner that appeared indecisive and deferential to the Chinese government. The explosion of travel restrictions that countries implemented to counter COVID-19 prompted arguments that these restrictions violated the IHR, violations that the WHO did not probe despite having authority to do so. Complaints also arose about WHO’s silence in the face of the human rights consequences of harsh government responses, such as mandatory quarantine and isolation measures.
A Tale of Two Decades: WHO and the IHR
Explaining why criticism and praise of WHO’s performance focus on different aspects of the IHR requires understanding how perspectives at WHO and among global health experts about the role of these regulations in global health governance have shifted. The initial decade of this century witnessed astonishing changes in global health that reflected heightened political interest from state and non-state actors, policy and governance innovation, and unprecedented levels of funding. These changes include the transformation of international law on infectious diseases accomplished with the adoption of the IHR in 2005.
The first test after the International Health Regulations entered into force was the H1N1 influenza pandemic in 2009.
WHO leadership during the SARS pandemic in 2003 made this transformation possible. The WHO Director-General, Gro Brundtland, confronted China over its SARS outbreak and, without approval from the countries concerned, issued warnings against travel to SARS-affected places. Brundtland acted without authority to take these steps. In addition, WHO took the lead in efforts to advance scientific understanding of the SARS coronavirus, develop public health strategies, and establish clinical treatment protocols. In adopting the IHR in the aftermath of SARS, WHO member states gave WHO unprecedented authority vis-à-vis state sovereignty and expanded the need for WHO’s scientific, medical, and public health capabilities.
The first test after the IHR entered into force in 2007 was the H1N1 influenza pandemic in 2009. The WHO Director-General, Margaret Chan, declared the world’s first public health emergency of international concern and issued recommendations that, among other things, advised against trade and travel measures. WHO coordinated scientific, medical, and public health efforts to understand the H1N1 virus, share information, treat people, and develop a vaccine. Post-pandemic analysis identified problems with WHO’s performance and the IHR’s functioning, but, overall, the response underscored the importance of WHO’s leadership and functional capabilities and the IHR’s role in global health governance.
However, controversies about WHO’s leadership, the organization’s capabilities, and the IHR dominated the conversation over the next decade. Concerns began after the H1N1 pandemic as WHO and its member states struggled from the damage done by the Great Recession. Facing a financial crisis, WHO cut the budget for its outbreak preparedness and response capacities, and distracted by economic turmoil, member states showed little interest in the recommendations made after the H1N1 pandemic to strengthen WHO and bolster the IHR.
The Ebola outbreak in West Africa in 2014 was a disaster for WHO and the International Health Regulations
The next major crisis was an Ebola outbreak in the Democratic Republic of the Congo that started in late 2018. WHO’s response to this outbreak demonstrated that it had re-invigorated its functional capacities. Indeed, the Democratic Republic of the Congo, with WHO’s help, brought the outbreak under control in difficult circumstances during 2019, with an anticipated declaration of the end of the outbreak expected this month.
Director-General Tedros eventually declared a public health emergency of international concern—but only after the outbreak became even more dangerous
However, WHO’s response to the Ebola outbreak in the Democratic Republic of the Congo exhibited resistance to exercising the power to declare a public health emergency under the IHR. A controversy emerged when the emergency committee—established under the IHR to advise the director-general on whether to declare a public health emergency —repeatedly concluded that the worsening outbreak did not qualify as a public health emergency of international concern. For many, the emergency committee’s reasoning, which Director-General Tedros accepted, did not accord with the IHR. Director-General Tedros eventually declared a public health emergency of international concern—but only after the outbreak became even more dangerous.
Lost in this back-and-forth over the IHR was something important—global health leaders expressed, and based their actions on, skepticism about key aspects of the IHR. The outbreak in the Democratic Republic of the Congo increased interest in the director-general having more options than the “declaration, no declaration” choice that the IHR provides. The emergency committee’s assertions that countries would implement unjustified measures after a declaration of a public health emergency of international concern suggested the committee believed that the exercise of this authority would do more harm than good. The committee also clearly had no confidence in the IHR rules designed to address problematic trade and travel measures imposed in response to outbreaks. In the end, the controversies about the IHR distracted from WHO’s impressive on-the-ground efforts to help the Democratic Republic of the Congo overcome Ebola.
This Pandemic was Politicized Before it Started
Understanding WHO’s behavior over the past decade helps us see that, before the novel coronavirus emerged in Wuhan, WHO was predisposed for global health reasons to exhibit leadership through deployment of its functional capabilities rather than by exercising authority it had to challenge governments politically. Leaving aside this strategy’s merits, the approach put WHO in a difficult position with COVID-19 because the disease emerged into a context that was already hyper-politicized within and beyond China.
China had imposed at home and promoted abroad a version of sovereignty intolerant of domestic dissent and foreign criticism
Well before the Wuhan outbreak, China had imposed at home and promoted abroad a version of sovereignty intolerant of domestic dissent and foreign criticism. China’s perspective on sovereignty constituted one of the most important features of the country’s rise to great-power status and its global ambitions. For China, the outbreak’s domestic and international implications were so serious that the response, including WHO’s involvement, had to reflect China’s position on sovereignty and its global stature.
Unsurprisingly, the official narratives from the Chinese government and WHO about the outbreak response scrupulously reflected China’s political requirements and calculations. This outcome reflects the convergence of WHO’s non-confrontational approach and China’s intolerance of any divergence from the party line. This convergence meant China’s political needs overwhelmed WHO’s desire to avoid politics in working with China in the interests of global health, leaving the organization vulnerable to questions about its interactions with China.
China’s political needs overwhelmed WHO’s desire to avoid politics in working with China in the interests of global health
Other countries—especially the United States—that are wary of China’s expanding power and intentions were also primed to interpret this disease event through a political lens. From the beginning, commentary in the United States framed the epidemic in China in geopolitical terms, used it to blame China’s political leaders and system for the tragedy, and faulted WHO for complicity with China’s perceived deception and propaganda. Such criticism implies that WHO’s interactions with China should have reflected U.S. political perspectives rather than China’s. The lack of convergence between U.S. interests and WHO’s actions left WHO exposed to attacks that intensified as the United States struggled with COVID-19 once it reached American shores.
The Westphalian Virus
The manner in which China and the United States politicized COVID-19 for geopolitical purposes bodes ill for international health cooperation
We do not know whether WHO’s functional contributions to the COVID-19 fight will protect it from recriminations about its interactions with China when the pandemic ends and the world evaluates this disaster. The manner in which China and the United States politicized COVID-19 for geopolitical purposes bodes ill for international health cooperation. What happened in this pandemic is a harbinger for what WHO will confront and have to navigate over the next decade. Further, balance-of-power politics will shape WHO’s future as much or more than the well-intentioned recommendations that post-pandemic reviews by experts will produce.
In this sense, COVID-19 has not changed the world as much as clarified how much the world has changed since the first decade of this century. Perhaps, then, the acrimony over what to call the novel coronavirus behind the pandemic should be ended by dubbing it the “Westphalian virus.”
David P. Fidler is a senior fellow for global health and cybersecurity at the Council on Foreign Relations.
EXCLUSIVE U.S. opposes plans to strengthen World Health Organization
The World Health Organization logo is pictured at the entrance of the WHO building, in Geneva, Switzerland, December 20, 2021. REUTERS/Denis Balibouse
Register now for FREE unlimited access to Reuters.com
The proposal, made by the WHO’s working group on sustainable financing, would increase each member state’s standing annual contribution, according to a WHO document published online and dated Jan. 4.
The plan is part of a wider reform process galvanised by the COVID-19 pandemic, which has highlighted the limitations of the WHO’s power to intervene early in a crisis.
Register now for FREE unlimited access to Reuters.com
But the U.S. government is opposing the reform because it has concerns about the WHO’s ability to confront future threats, including from China, U.S. officials told Reuters.
It is pushing instead for the creation of a separate fund, directly controlled by donors, that would finance prevention and control of health emergencies.
Four European officials involved in the talks, who declined to be named because they were not authorised to speak to the media, confirmed the U.S. opposition. The U.S. government had no immediate comment.
Supporters say that the current reliance on voluntary funding from member states and from charities such as the Bill and Melinda Gates Foundation forces the WHO to focus on priorities set by the funders, and makes it less able to criticise members when things go wrong.
An independent panel on pandemics that was appointed to advise on the WHO reform had called for a much bigger increase in mandatory fees, to 75% of the core budget, deeming the current system «a major risk to the integrity and independence» of the WHO.
LONG-STANDING SCEPTICISM
The WHO itself responded to a query by saying that «only flexible and predictable funds can enable WHO to fully implement the priorities of the Member States».
Top European Union donors, including Germany, back the plan, along with most African, South Asian, South American and Arab countries, three of the European officials said.
The proposal is to be discussed at the WHO’s executive board meeting next week but the divisions mean no agreement is expected, three of the officials said.
The WHO confirmed there was currently no consensus among member states, and said talks were likely to continue until the annual meeting in May of the World Health Assembly, the agency’s top decision-making body.
European donors in particular favour empowering, rather than weakening, multilateral organisations including the WHO.
One European official said the U.S. plan «causes scepticism among many countries», and said the creation of a new structure controlled by donors, rather than by the WHO, would weaken the agency’s ability to combat future pandemics.
Washington has been critical of the WHO for some time.
Former president Donald Trump pulled the United States out of the WHO after accusing it of defending China’s initial delays in sharing information when COVID-19 emerged there in 2019.
The Biden administration rejoined soon after taking office, but officials told Reuters they think the WHO needs significant reform, and raised concerns about its governance, structure and ability to confront rising threats, not least from China.
One of the European officials said other big countries, including Japan and Brazil, were also hesitant about the published WHO proposal.
A Brazilian official with knowledge of the discussions said Brazil agreed that WHO funding needed to be looked at, but said it opposed the proposal to raise contributions as it had run up deficits tackling the virus and was now facing a fiscal crunch.
Instead, the official said the WHO needed to investigate other ways to raise funds, such as charging for its services, cutting costs or relocating operations to cheaper countries.
«Raising contributions should be the last resort,» said the official, who was not authorized to speak publicly about the discussions.
Two of the European officials said China had not yet made its position clear, while a third official listed Beijing among the critics of the proposal.
The governments of Japan and China had no immediate comment.
Explainer: How the World Health Organization might face future pandemics
The World Health Organization logo is pictured at the entrance of the WHO building, in Geneva, Switzerland, December 20, 2021. REUTERS/Denis Balibouse
Register now for FREE unlimited access to Reuters.com
A new pact is among more than 200 recommendations for shoring up the world’s defences against new pathogens made by various reviewers following the COVID-19 pandemic that has killed more than 6.2 million people in two years.
The WHO itself is facing calls for reform after an independent panel described it as «underpowered» when COVID-19 struck, with limited powers to investigate outbreaks and coordinate containment measures. read more
Register now for FREE unlimited access to Reuters.com
A Washington-led effort to build a global pandemic prevention fund hosted by the World Bank is among initiatives that could determine the future of the 74-year old body.
WHAT IS THE PANDEMIC TREATY?
The WHO already has binding rules known as the International Health Regulations (2005) which set out countries’ obligations where public health events have the potential to cross borders. These include advising the WHO immediately of a health emergency and measures on trade and travel.
Adopted after the 2002/3 SARS outbreak, these regulations are still seen as functional for regional epidemics like Ebola but inadequate for a global pandemic.
Suggested proposals for the pact include the sharing of data and genome sequences of emerging viruses and rules on equitable vaccine distribution. read more
The European Union is pushing for a ban on wildlife markets and incentives for reporting of new viruses or variants, an EU official told Reuters. read more
Member states have an August deadline to decide on an initial version of the pact, which is backed by WHO director-general Tedros Adhanom Ghebreyesus. He is likely to be elected unopposed for a second term in May.
It would be only the second such health accord after the 2003 Framework Convention on Tobacco Control, a legally-binding treaty which aims to reduce smoking via taxation and rules on labelling and advertising.
HOW DO COUNTRIES VIEW THE PACT?
The EU proposed the treaty and is its biggest backer, with support from Britain, Indonesia, Kenya and others.
The United States will take part in the talks but has opposed a binding treaty. India and Brazil have also voiced reservations.
With so many member countries involved, securing agreement is likely to be tricky.
HOW WOULD IT WORK?
It is not yet clear how the 2005 regulations and the new pandemic treaty might fit together.
It remains to be determined whether negotiators will include compliance measures such as sanctions.
WHAT OTHER REFORMS ARE IN THE WORKS?
Separate talks on a U.S. initiative to overhaul the 2005 rules are taking place this week.
Washington’s proposals aim to boost transparency and grant the WHO quicker access to outbreak sites. Several diplomats said they are likely to prove too ambitious, with opposition from China and others expected on national sovereignty grounds.
China did allow WHO-led expert teams to visit the COVID-19 epicentre in Wuhan, but the WHO says it is still withholding clinical data from early cases that may hold clues about the origins of the SARS-CoV-2 virus. read more
Reforms to the WHO funding structure to make it more sustainable and flexible in the event of a pandemic are being discussed by WHO member states in another working group.
So far the United States, which until the pandemic was the WHO’s top donor, has opposed plans to increase member countries’ annual contributions. read more
Thanks for contacting us. We’ve received your submission.

More On: world health organization
WHO recommends new way to treat Ebola
NYC monkeypox madness repeats ugly COVID story
Spain confirms country’s second monkeypox death in as many days
The abuses could spook potential donors and partners as the organization begins its week-long annual meeting Monday in Geneva, seeking increased support to fight a devastating outbreak of Ebola in Congo and other deadly diseases including polio, malaria and measles.
But recent documents show WHO auditors found some WHO staffers were still brazenly misrepresenting the reasons for their travel to exploit loopholes in the organization’s policies and flying business class, which can be several times more expensive than economy, even though they did not meet the criteria to do so.
The agency’s inability to curb its expenses could undermine its credibility and make it more difficult to raise money to fight health crises, according to Sophie Harman, a global health professor at Queen Mary University in London. She said the problem wasn’t so much the amount that WHO was spending on travel, but how it was being used.
“WHO needs to get its own house in order to legitimately go to the international community saying, ‘We need more money for Ebola,’” she said.
In a statement on Monday, WHO said “travel is often essential to reaching people in need” and noted more than half of its travel spending went to bring outside experts and country representatives, often from developing countries, to technical meetings.
“When staff travel, they do a range of things, including responding to emergencies, assessing countries’ emergency preparedness, implementing vaccine and other public health campaigns, training health workers and more,” the agency said.
It added that a range of new measures were adopted in 2018 that aimed to make sure “staff travel is necessary, economical, appropriate and efficient.”
“WHO’s travel policy prohibits first-class travel for all staff,” the agency said, adding that Tedros prioritizes trips “where he can make a difference on the ground.”
WHO said a host of initiatives have helped cut travel costs. For non-emergency travel, the proportion of business class flights dropped to 18 percent last year, from 27 percent the previous year. Yet other international aid agencies, including Doctors Without Borders and the US Centers for Disease Control and Prevention, explicitly forbid staff from traveling in business class.
While overall spending has fallen, abuses continue, documents show. In one report provided to the AP, external WHO auditors analyzed 116 randomly selected travel claims that were flagged as “emergency” requests and therefore exempt from stricter UN travel controls. They found proof that in more than half of the claims, the travel was instead for regular duties like attending workshops or speaking engagements.
“We see therefore a culture of non-compliance by staff involved in emergency operations,” the report authors said. “Raising a (travel request) as emergency, even if it is not compliant with the criteria for emergency travel, shows a breakdown in controls and results (in a) waste of resources.”
WHO’s external auditors said when some staffers flew business class even though they didn’t meet the UN criteria to do so, they failed to submit paperwork justifying the exception.
“Based on the difference in ticket costs for business class and economy class, savings could have been realized by the organization,” the report said, citing more than 500 travel requests last year that may have broken the rules.
In a series of anonymous emails sent to WHO directors last year, a whistleblower alleged there were numerous instances of “senior staff travelling with girlfriends on fabricated missions,” including during the 2014 Ebola outbreak in West Africa. One message claimed a senior staffer flew to Australia from Geneva “on a trumped-up trip at WHO expense” that cost the organization 11,000 Swiss francs ($10,889).
In December, Tedros ordered an internal probe into these and other misconduct allegations.
The WHO auditors’ report comes at time of critical financial need for the agency.
Harman said WHO needs to pay more attention to staff needs on the front lines of deadly outbreaks. Health workers, many of them poorly equipped, have been killed in Congo by militants rejecting vaccination efforts and other attempts to prevent or treat Ebola.
“There’s a disconnect between the fact that people who are doing safe burials in (Congo) aren’t getting paid, yet someone is using WHO’s travel budget to fund their business-class ticket,” she said.
From Wikipedia, the free encyclopedia
Tell your friends about Wikiwand!
Gmail Facebook Twitter Link
Suggest as cover photo
Would you like to suggest this photo as the cover photo for this article?
Thank you for helping!
Your input will affect cover photo selection, along with input from other users.
Thanks for reporting this video!
This browser is not supported by Wikiwand 🙁
Wikiwand requires a browser with modern capabilities in order to provide you with the best reading experience.
Please download and use one of the following browsers:
An extension you use may be preventing Wikiwand articles from loading properly.
If you’re using HTTPS Everywhere or you’re unable to access any article on Wikiwand, please consider switching to HTTPS (https://www.wikiwand.com).
An extension you use may be preventing Wikiwand articles from loading properly.
If you are using an Ad-Blocker, it might have mistakenly blocked our content. You will need to temporarily disable your Ad-blocker to view this page.
world health organization
1 World Health Organization
2 World Health Organization
ВОЗ
Всемирная Организация Здравоохранения
Одна из специализированных организаций системы ООН, являющаяся полномочным руководящим и координирующим органом в сфере международной деятельности по охране здоровья. Организация была основана в 1948 году.
[МУ 64-01-001-2002]
Тематики
Обобщающие термины
Синонимы
Всемирная организация здравоохранения
ВОЗ
Специализированное учреждение системы ООН.
[Англо-русский глоссарий основных терминов по вакцинологии и иммунизации. Всемирная организация здравоохранения, 2009 г.]
Тематики
Синонимы
3 World Health Organization
4 World Health Organization
5 world health organization
6 World Health organization
7 World Health Organization
8 World Health Organization
9 World Health Organization
10 World Health Organization
11 World Health Organization
12 world health organization
13 World Health Organization
14 WHO World Health Organization
15 (the) World Health Organization
16 European Regional Bureau of the World Health Organization
17 WHO (World Health Organization)
18 Organization
19 organization
to ban an organization — объявлять вне закона / запрещать организацию
to disband / to dissolve an organization — распускать организацию
to eliminate smb from an organization — исключать кого-л. из организации
to establish an organization — основывать / учреждать организацию
to expel smb from an organization — исключать кого-л. из организации
to extend one’s organization — ( somewhere) создавать филиал своей организации (где-л.)
to found an organization — основывать / учреждать организацию
20 world
the whole [entire\] world — весь мир
to travel around the world — путешествовать вокруг света, путешествовать по миру
Are there any other inhabited worlds? — Есть ли еще обитаемые миры, кроме нашего?
the world of sport, the sports world — спортивный мир
the animal [the vegetable\] world — животный [растительный\] мир
the ancient [the medieval\] world — древний [средневековый\] мир
to know the world — иметь опыт, знать жизнь
to come up [to rise, to make one’s way\] in the world — сделать карьеру, преуспеть в жизни
world championship — первенство [чемпионат\] мира
См. также в других словарях:
World Health Organization — n. An agency of the United Nations that works to promote international public health. abbrv. WHO The Essential Law Dictionary. Sphinx Publishing, An imprint of Sourcebooks, Inc. Amy Hackney Blackwell. 2008 … Law dictionary
World Health Organization — WHO redirects here. For other uses, see Who (disambiguation). World Health Organization منظمة الصحة العالمية 世界卫生组织 Organisation mondiale de la Santé Всемирная организация здравоохранения Organización Mundial de la Salud … Wikipedia
World Health Organization — Flagge der WHO Weltgesundheitsorganisation, Genf Die Weltgesundheitsorganisation (engl. World Health Organization, WHO) ist eine Sonderorganisation der … Deutsch Wikipedia
World Health Organization — A part of the United Nations that deals with major health issues around the world. The World Health Organization sets standards for disease control, health care, and medicines; conducts education and research programs; and publishes scientific… … English dictionary of cancer terms
World Health Organization — Weltgesundheitsorganisation; WHO * * * I World Health Organization [wəːld helθ ɔːgənaɪ zeɪʃn, englisch], Abkürzung WHO, englische Bezeichnung für die Weltgesundheitsorganisation. II World Health Organization (Abkürzung WHO): englische… … Universal-Lexikon
World Health Organization — Organisation mondiale de la santé Pour les articles homonymes, voir OMS (homonymie) et Who. Organisation mondiale de la santé … Wikipédia en Français
World Health Organization — World Health Or|ga|ni|za|tion, the WHO an international organization that is part of the ↑UN (United Nations), which helps countries improve their people s health by giving medicines and providing information and education about diseases,… … Dictionary of contemporary English
World Health Organization Framework Convention on Tobacco Control — The World Health Organization Framework Convention on Tobacco Control (abbreviated WHO FCTC) is a treaty adopted by the 56th World Health Assembly on May 21, 2003. cite web | url=http://www.who.int/fctc/en/index.html | title=WHO Framework… … Wikipedia
World Health Organization Goodwill Ambassador — WHO Goodwill Ambassadors are celebrity advocates of the World Health Organization (WHO) and utilize their talent and fame to advocate for health and well being.WHO Goodwill Ambassadors, and the year they were appointed:*Yohei Sasakawa, chairman… … Wikipedia
World Health Organization — WHO or, in French, OMS (Organisation Mondiale de la Sante), a specialized agency of the United Nations established in 1948 to further international cooperation for improved health conditions. Although it inherited specific tasks relating to… … Medical dictionary
World Health Organization — an agency of the United Nations, established in 1948, concerned with improving the health of the world s people and preventing or controlling communicable diseases on a worldwide basis through various technical projects and programs. Abbr.: WHO * … Universalium
Open letter to World Health Organisation
The below open letter was sent to Dr Tedros Adhanom Ghebreyesus and Dr Zhang Qi of the World Health Organisation on the 6th April to coincide with World Health Day and on the 21st April for World Earth Day. Please find the covering emails and open letter below.
Covering email dated 6 th April 2020
On behalf of the Lion Coalition, I am sending the attached joint letter signed by 241 leading animal welfare and conservation organisations to World Health Organisation.
In the midst of a global pandemic and on the occasion of World Health Day, this letter calls upon WHO to state the proven link between wildlife markets and their serious threats to human health. We outlined concrete measures that WHO and its member States should take to be able to avert another pandemic.
We are looking forward to hear your response and stand ready to assist.
Covering email dated 21st April 2020
Further to our joint letter sent on the 6 th April 2020, to which we are eagerly awaiting a response, please find attached said letter now signed by 339 leading animal welfare and conservation organisations from all around the world.
Subsequent to the original release of our letter, on the 17 th April Dr Tedros Adhanom Ghebreyesus held a media briefing to clarify among others the WHO’s position on “wet markets”. He stated:
We applaud WHO for stating that governments must rigorously enforce bans on the sale and trade of wildlife for food. However, in most countries such bans don’t exist. We also note that there are many ways in which wildlife is utilised, like the use of wild animals for the production of traditional medicine, that could pose a risk to human health.
Elizabeth Maruma Mrema, acting Executive Secretary of the UN Convention on Biological Diversity, is another of dozens of experts, who have shared these concerns in recent weeks. She stated:
“The message we are getting is if we don’t take care of nature, it will take care of us. It would be good to ban the live animal markets as China has done and some countries.”
In addition to the concrete measures that WHO and its member States should take in order to avert future zoonotic pandemics (as outlined in the attached letter) and in light of the statements by Dr. Nabarro (WHO Special Envoy on COVID-19), Ms. Mrema, and other public health experts, scientists and political leaders, we call on the WHO to release a formal position statement containing clear advice to governments to institute comprehensive and rigorously enforced bans on live wildlife markets and to close down the commercial wildlife trade which poses a risk to public health.
We would like to emphasise our focus on the need to tackle the commercial trade in wildlife, and to close markets that sell live wild animals or products, rather than markets at which other types of fresh produce might be traded.
We are looking forward to receiving your response and stand ready to assist.
Open Letter sent on both occasions
Dear Dr Tedros Adhanom Ghebreyesus and Dr Zhang Qi,
The undersigned organisations acknowledge and commend the World Health Organisation’s current efforts to contain the pandemic spread of the coronavirus disease (COVID-19).
On the occasion of World Health Day, in the midst of a global pandemic believed to have originated in a live wildlife market, we call upon the WHO to publicly and unequivocally state the proven link between these markets and serious threats to human health. In line with its stated mission to serve public health at all times, we urge the WHO to recommend that governments worldwide permanently ban live wildlife markets and the use of wildlife in traditional medicine. This decisive action, well within the WHO’s mandate, would be an impactful first step in adopting a highly precautionary approach to wildlife trade that poses a risk to human health.
While a robust global response is critical in detecting, treating and reducing transmission, it is equally necessary to take vital measures to prevent similar emerging infectious diseases developing into pandemics with the associated threats to human life, and social and economic well-being.
Zoonotic diseases are responsible for over two billion cases of human illness and over two million human deaths each year. [5] How many of these cases directly or indirectly originate from wildlife is hard to calculate, due to overlapping reservoirs in livestock and wild animal populations. However, considering the significance of wildlife as a reservoir of emerging infectious diseases, wildlife origins of zoonoses must be of primary concern. Sixty percent (60%) of emerging infectious diseases are zoonotic and 70% of these are thought to originate from wildlife. [6]
The risk of zoonotic disease transmission is heightened further by the unregulated and unhygienic conditions associated with wildlife markets, where close proximity between humans and animals provide the perfect opportunity for pathogens to spread. This risk is further exacerbated by the conditions in which animals are typically farmed or collected from the wild, transported to and held at such markets, which inevitably result in large numbers of animals of different species being held in crowded conditions in close proximity, causing immense stress and weakening their immune systems. Such conditions, coupled with close proximity to people at wildlife markets, provide the ideal situation for pathogens to replicate, spread, and potentially infect people.
Pangolins, which are considered likely by some researchers to be involved in the transmission chain of COVID-19, are commonly used as ingredients for Traditional Medicine, as are many other wildlife species such as turtles, leopards, tigers, lions and bears, with bear bile injections being officially recommended as a treatment for COVID-19. [7] These animals are either farmed or poached from the wild to supply the demand – a practice that is entirely unnecessary given the viable plant or non-wildlife based alternatives recognized by Traditional Medicine. Risk of disease transmission is prevalent across all aspects of wildlife trade, which supplies products to the Traditional Medicine industry. For example, bovine tuberculosis has been documented among wild and captive-bred lions, posing a substantial risk of zoonosis to consumers and people involved in the lion bone trade, particularly those who work in breeding farms, slaughter and processing facilities in South Africa. Reptiles such as snakes and geckos, which are also used in Traditional Medicine, are frequent sources of Salmonellosis infections in people. [8]
Any policies and practices that sustain the wildlife trade carry a huge and unpredictable public health risk that could lead to future outbreaks and pandemics of zoonotic diseases among human populations.
In conclusion, the demand for wildlife and wildlife products is a primary cause of the emergence and spread of zoonotic diseases and a severe risk to global health. We call on the World Health Organisation to recognise that it has a significant role to play to mitigate such global health risks.
We therefore strongly urge the World Health Organisation to:
We welcome your consideration of this important matter and stand ready to assist.
For and behalf of the following 339 organisations
| AAP Animal Advocacy and Protection |
| Aaranyak – India |
| Action for Dolphins |
| Action for Elephants |
| Advocates4Earth |
| Africa Network for Animal Welfare |
| African Pangolin Working Group |
| Albert Schweitzer Stiftung für unsere Mitwelt |
| All Life In A Viable Environment |
| Alliance for Earth, Life, Liberty & Advocacy |
| Amboseli Trust for Elephants |
| Ananta Jyoti Dhayn Kendra |
| Andean Cat Alliance |
| Anima International |
| Animal Aid International |
| Animal Alliance of Canada |
| Animal Concerns Research & Education Society |
| Animal Defenders International |
| Animal Friends Croatia |
| Animal Friends Jogja |
| Animal Guardians |
| Animal Kingdom Foundation |
| Animal Law Reform South Africa |
| Animal Legal Defense Fund |
| Animal Liberation Sanctuary |
| Animal People Forum |
| Animal Projects & Environmental Education Sdn Bhd |
| Animal Protection Agency |
| Animal Protection and Environmental Sanctuary |
| Animal Protection Denmark / Dyrenes Beskyttelse |
| Animal Protection Party of Canada |
| Animal Rescue Cambodia |
| Animal Research Connections |
| Animal Rights Center Japan |
| Animal Sanctuary Trust Indonesia |
| Animal Society for the Protection of Animals (Macau) |
| Animal Talk Africa |
| Animal Welfare And Anti Harassment Society |
| Animals Asia Foundation |
| Animals Australia |
| Animals Lebanon |
| Annamiticus |
| Ape Alliance |
| ARCA Brasil |
| Association Daridibó |
| Association de Défense des Ressources Marines |
| AWARE: Animal Welfare Awareness, Research and Education |
| Baboon Matters |
| Bali Animal Welfare Association |
| Bali Street Dog Fund Australia |
| Ban Animal Trading |
| Bat Conservation Africa |
| Bat Conservation Trust |
| BatLife Europe |
| BatLife Ghana |
| Bats without Borders |
| Bears in Mind |
| Beauty Without Cruelty – South Africa |
| Big Cat Rescue |
| BIOCONCIENCIA A.C. |
| Biofuelwatch |
| Blood Lions |
| Blue Cross of India |
| Blue Sky Society Trust |
| Bolivian Bat Conservation Program |
| Bonobo Conservation Initiative |
| Born Free Foundation |
| Born Free USA |
| Bornean Sun Bear Conservation Centre |
| Borneo Nature Foundation |
| Brighter Green |
| Bring the Elephant Home |
| Campaign to Ban Trophy Hunting |
| Campaigns and Activism for Animals in the Industry (CAAI) |
| Cape Leopard Trust |
| Captured in Africa Foundation |
| CATCA Environmental and Wildlife Society |
| Center for Biological Diversity |
| Centre for Animal Rehabilitation and Education |
| Centre for Wildlife Studies |
| Cetacean Society International |
| Change for Animals Foundation |
| Cheetah Conservation Botswana |
| Chelui4lions |
| Coalition of African Animal Welfare Organisations |
| Code Animal |
| Community Dog Welfare Kopan |
| Compassion in World Farming |
| Compassion Unlimited Plus Action |
| Compassion Works International |
| Conservación de Mamíferos Marinos de Mexico |
| Conservation Action Trust India |
| Countryside Management Association |
| CPR Environmental Education Centre |
| Danau Girang Field |
| David Shepherd Wildlife Foundation |
| Defenders of Wildlife |
| Department of Forestry and Wildlife Management, Taraba State University Jalingo |
| Deutscher Tierschutzbund e.V. (Germany) |
| Djurskyddet Sverige (Animal Welfare Sweden) |
| Dogstop |
| Dutch Gorilla Foundation |
| Dutch Society for the Protection of Animals (Dierenbescherming) |
| Dynamic Planet |
| Earth Island Institute Asia Pacific |
| Earth Island Institute Int’l Marine Mammal Project |
| Eco Activists for Governance and Law Enforcement (EAGLE Network) |
| Elephanatics |
| Elephant Human Relations Aid |
| Elephant Reintegration Trust |
| Elephants Alive |
| Elephants DC |
| ElephantVoices |
| Elephation |
| EMS Foundation |
| Endangered Species Coalition |
| Environmental Investigation Agency |
| Equilibrium Futures |
| Eurogroup for Animals |
| FAADA, Spain |
| Federation of Indian Animal Protection Organisations |
| FIAPO |
| Fish Welfare Initiative |
| FLIGHT |
| Fondation Brigitte Bardot |
| Fondation Franz Weber |
| For Elephants |
| For the Love of Wildlife (FLOW) |
| For Tigers |
| Foundation Chimbo |
| Four Paws – International |
| Four Paws – South Africa |
| Franciscan Order – Hong Kong |
| Frankfurt Zoological Society |
| Fraternité pour le respect animal |
| Freeland |
| Friendicoes SECA |
| Friendicoes SECA – India |
| Friends of Animals |
| Friends of Conservation UK |
| Friends of the Orangutans Malaysia |
| Future 4 Wildlife |
| Future for Elephants e.V. |
| Gearing Up 4 Gorillas |
| Gibbon Conservation Society |
| Global Action in the Interest of Animals |
| Global Animal Law |
| Global Biodiversity Youth Network – Kenya |
| Global March for Elephant and Rhino Poaching |
| Global Sanctuary for Elephants |
| Global White Lion Protection Trust |
| Global Youth Biodiversity Network – Kenya |
| Gordon Consulting New Zealand |
| Great Ape Project |
| Great Apes Film Initiative |
| Greek Animal Welfare Fund |
| Green Girls in Africa |
| GREY2K USA Worldwide |
| Greyhound Compassion |
| Hands Off Fernkloof |
| Help Animals India |
| Himalayan Animal Rescue Trust |
| Hollow Paws |
| Humane Research Australia |
| Humane Society International – Africa |
| Humane Society International – Australia |
| Humane Society International – Global |
| HUTAN – Kinabatangan Orang-utan Conservation Programme |
| In Defence of Animals – India |
| In Defence of Animals – USA |
| In Defense of Animals – International |
| Institute for Critical Animal Studies – Africa |
| International Aid For Animal Foundation |
| International Animal Rescue |
| International Otter Survival Fund |
| International Primate Protection League |
| International Wildlife Bond |
| Irish Society for the Prevention of Cruelty to Animals |
| Israeli Primate Sanctuary |
| Jakarta Animal Aid Network |
| Japan Anti-Vivisection Association |
| Japan Tiger and Elephant Fund |
| Japan Wildlife Conservation Society |
| Kasanka Trust Limited |
| Korea Animal Rights Advocates |
| KYMA sea conservation & research |
| La Fondation Droit Animal, Ethique et Sciences (LFDA) |
| Lady Freethinker |
| Landmark Foundation |
| Latin American and Caribbean Network for Bat Conservation (RELCOM) |
| Lawrence Anthony Earth Organization |
| Lawyers for Animal Protection in Africa |
| Liberia Chimpanzee Rescue & Protection |
| Lifelong Animal Protection |
| Loomus (Estonia) |
| Love Animal House Thailand |
| LUSH UK |
| Mabula Ground Hornbill Project |
| Melbourn Dolphin |
| Monkey Helpline |
| Moving Animals |
| National Association of Areas of Outstanding Natural Beauty |
| National Council of Societies for the Prevention of Cruelty to Animals |
| National Council of SPCAs – South Africa |
| National Park Rescue |
| Natural Resources Conservation Network |
| Neotropical Primate Conservation |
| Nepal Animal Welfare and Research Center |
| New Zealanders for Endangered Wildlife |
| NOAH – For Animal Rights |
| Nsefu Wildlife Conservation Foundation |
| NY4Whales |
| Oceanic Preservation Society |
| Ol Pejeta Conservancy |
| One Nature Films |
| One Voice (France) |
| OneKind |
| ONG Sante Animale Afrique |
| Orangutan Appeal UK |
| Orangutan Foundation |
| Orca Rescues Foundation |
| OSCAP |
| Outraged South African Citizens Against Rhino Poaching |
| Painted Dog Conservation – Zimbabwe |
| Pan African Sanctuary Alliance |
| Panthera |
| Panthera Africa |
| PEACE (Put an End to Animal Cruelty and Exploitation) |
| Pegasus Foundation |
| Penguin Global Society |
| People for Animal Care and Kindness |
| People for Animals, Odisha |
| People for the Ethical Treatment of Animals (PETA) |
| Performing Animal Welfare Society |
| PETA Asia 亚洲善待动物组织 |
| Pettus Crowe Foundation |
| Pit-Track K9 Conservation & Anti-Poaching |
| Plants and Animals Welfare Society (PAWS Asia) |
| Pro Elephant Network |
| Pro Wildlife |
| Protecting African Lions |
| Pup Aid |
| Rapad Maroc (Morocco) |
| reEarth |
| Responsabile Nazionale Diritti Animali |
| Rettet den Regenwald (Rainforest Rescue) |
| Royal Society for the Prevention of Cruelty to Animals |
| RSPCA Australia |
| SAI (Save Animals Initiative) Sanctuary Trust |
| Sanctuary Education Advisory Specialists |
| Sanctuary for Health & Reconnection to Animals & Nature |
| Santuário de Elefantes Brasil |
| Sarawak Society for the Prevention of Cruelty to Animals |
| Save The Asian Elephants |
| Scorpion Foundation Indonesia |
| Sea Shepherd Legal |
| Sea Shepherd South Africa |
| SEY Animal Welfare Finland |
| Shark Research Institute |
| Showing Animals Respect and Kindness |
| Small Mammal Conservation Organisation |
| Snow Leopard Conservancy |
| Society for Dolphin Conservation, Germany |
| Society for the Prevention of Cruelty to Animals – Selangor |
| Society for the Prevention of Cruelty to Animals – Singapore |
| Society for the Protection of Animals Ljubimci |
| Society for Travelers Respecting Animal Welfare |
| Soi Dog Foundation |
| South Peninsula Customary Khoisan Council |
| Southern African Fight for Rhinos |
| Species Survival Network |
| Stichting Painted Dog Conservation |
| Stichting SPOTS |
| Sumatran Orangutan Society |
| Sun Bear Centre – Kalimantan |
| Sustainable Travel and Tourism Agenda – Kenya |
| Taiwan SPCA台灣防止虐待動物協會 |
| Tanglewood Foundation |
| Taraba Nature Conservation Initiative – Nigeria |
| Teyeliz, A.C |
| The Corbett Foundation |
| The Elephants and Bees Project |
| The Emergent Disease Foundation |
| The Gorilla Foundation |
| The Humane League Japan |
| The Humane Society of Canada |
| The Jane Goodall Institute – Nepal |
| The Kerulos Center for Nonviolence |
| The Philippines Animal Welfare Society |
| The Rufford Foundation |
| The Wildlife and Environmental Protection of Trinidad and Tobago |
| The Winsome Constance Kindness Trust |
| Transfrontier Africa |
| Tree of Compassion |
| Trésor Foundation |
| TRUNKS & LEAVES Inc |
| Tusk Trust |
| Two Million Tusks |
| Ulinzi Africa Foundation – Kenya |
| Unexpected Wildlife Refuge |
| Vancouver Humane Society |
| Vervet Monkey Foundation |
| Vogelgat Private Nature Reserve |
| Voice for Asian Elephants Society |
| Voice for dogs abroad |
| Voice4Lions – South Africa |
| Voice4Lions – UK |
| Voices for Animals – Russia |
| VShine Animal Protection Association |
| Water and Environment Media Network – Uganda |
| Wellbeing International |
| Wild Futures |
| Wild Law Institute |
| Wild Welfare |
| WildAid |
| WildAid Southern Africa |
| Wildlife ACT |
| Wildlife Alliance |
| Wildlife and Environmental Society of Malawi (WESM) |
| Wildlife At Risk International |
| Wildlife Impact |
| Wildlife Protection Society of India |
| Wildlife Rescue |
| Wildlife Rescue and Conservation Association, Guatemala |
| Wildlife Rescue and Rehabilitation Centre |
| Wildlife SOS |
| Wildlife SOS – India |
| WildlifeDirect |
| Working Wild |
| World Animal Net |
| World Animal Protection – Africa |
| World Animal Protection – International |
| World Cetacean Alliance |
| World For All Animal Care And Adoptions |
| World Parrot Trust |
| Yangon Animal Shelter |
| Zimbabwe Elephant Foundation |
| Zoocheck Canada |
[1] In this document the term ‘wildlife’ refers to fauna in the wild or bred in captivity.
[2] Shereen, M.A., Khan, S., Kazmi, A., Bashir, N. and Siddique, R., 2020. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. Journal of Advanced Research.
[3] Andersen, G.A., Rambaut, A., Lipkin, W.I. et al. The proximal origin of SARS-CoV-2. Nat Med (2020)
[4] World Health Organisation. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. https://www.who.int/csr/sars/country/table2004_04_21/en/
[5] Grace, D., Mutua, F., Ochungo, P., et al. Mapping of poverty and likely zoonoses hotspots. Zoonoses Project 4. Report to the UK Department for International Development. 2012
[6] Jones, K.E., Patel, N.G., et al. Global trends in emerging infectious diseases. Nature. 2008
[7] Office of the Chinese Medicine Bureau, General Office of the Health and Health Commission. Notice on Issuing a New Coronary Virus Pneumonia Diagnosis and Treatment Plan (Trial Version 7). issued March 03 2020. Available as PDF on http://www.gov.cn/zhengce/zhengceku/2020-03/04/content_5486705.htm
[8] Mermin, J., Hutwagner, L., Vugia, D., et al. Reptiles, Amphibians, and Human Salmonella Infection: A Population-Based, Case-Control Study. Clinical Infectious Diseases 38 (Supp 3). 2004
[9] World Animal Protection. Cruel Cures – The industry behind bear bile production and how to end it. 2020
[10] Moorhouse, T.P., Coals, P.G.R., D’Cruze, N., Macdonald, D.W. Reduce or redirect? Which social marketing interventions could influence demand for traditional medicines? Biological Conservation 242.2020
[11] Wang, H., Shao, J., Chuai, Z., et al. Wildlife consumption ban is insufficient. Science. Vol 367, Issue 6485. 2020
Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors
Non-communicable diseases (NCDs) are of increasing concern for society and national governments, as well as globally due to their high mortality rate. The main risk factors of NCDs can be classified into the categories of self-management, genetic factors, environmental factors, factors of medical conditions, and socio-demographic factors. The main focus is on the elements of self-management and to reach a consensus about the influence of food on risk management and actions toward the prevention of NCDs at all stages of life. Nutrition interventions are essential in managing the risk of NCDs. As they are of the utmost importance, this review highlights NCDs and their risk factors and outlines several common prevention strategies. We foresee that the best prevention management strategy will include individual (lifestyle management), societal (awareness management), national (health policy decisions), and global (health strategy) elements, with target actions, such as multi-sectoral partnership, knowledge and information management, and innovations. The most effective preventative strategy is the one that leads to changes in lifestyle with respect to diet, physical activities, cessation of smoking, and the control of metabolic disorders.
Introduction
Non-communicable diseases (NCDs), also known as chronic diseases, are medical conditions that are associated with long durations and slow progress (Figure 1). Most NCDs are non-infectious and are the result of several factors, including genetic, physiological, behavioral, and environmental factors (1). According to the World Health Organization (WHO), NCDs are the leading cause of death worldwide, responsible for 71% of the total number of deaths each year. The top four killers among NCDs with the highest number of deaths are cardiovascular diseases (17.9 million deaths annually), cancers (9.0 million), respiratory diseases (3.9 million), and diabetes (1.6 million) (Figure 1) (1). However, the term of NCDs has been extended to cover a wide range of health problems, such as hepatic, renal, and gastroenterological diseases, endocrine, hematological, and neurological disorders, dermatological conditions, genetic disorders, trauma, mental disorders, and disabilities (e.g., blindness and deafness) (2). The main risk factors contributing to NCDs involve unhealthy diets, physical inactivity, tobacco use, and alcohol misuse. Hence, most of these diseases are preventable as they eventually progress in early life due to lifestyle aspects (3). There is an increasing concern that poor diet has increased the potential risk, causing chronic diseases, and nutrition problems in the public health sector (4). Historically, many NCDs have been directly linked to economic growth and were called “diseases of the rich.” Now, the burden of NCDs in developing countries has increased. Further, mortality in low and middle-income countries has doubled the burden of NCDs. The growing interest in population well-being and economic growth, based on Gross National Happiness (GNH), has recently attracted more attention. The epidemic of NCDs hinders the progress of GNH because good health is necessary in order to achieve happiness (5). Bhutan’s experience suggests that strategic opportunities to minimize NCDs and to promote population well-being can be taken advantage of by joining the health sector with other sectors at the individual and organizational levels (5).
Figure 1. List of non-communicable diseases (NCDs) [Created with BioRender].
Health and well-being are the primary goals of society in regards to food choice (6). Researchers have pointed out that the core of the health-conscious lifestyle is directed toward a wellness-oriented lifestyle (5) and the behavior of people determines their health status (7). Nutritionists have been reported to be associated with many chronic diseases, but designed studies exploring the association between diet, nutrition, and NCDs are rare (8). Thus, lifestyle modifications and interventions to reduce the risk of NCDs is the priority in the primary prevention of diseases. Hence, finding answers to the following questions can significantly contribute to a better and healthier society:
• What are NCDs and their risk factors?
• What are the most used interventions in managing the risk of NCDs?
• What are the contemporary prevention strategies for NCDs?
The current review focuses on the answers to the previous questions and highlights several strategic models in the contemporary management of NCDs.
Key Risk Factors of NCDs
Several factors can increase the amount of opportunities to develop NCDs and can be classified in different ways. In one approach, risk factors are classified as modifiable or non-modifiable factors that can have changeable or non-changeable conditions, respectively. The modifiable risk factors involve high blood pressure, smoking, diabetes mellitus, physical inactivity, obesity, and high blood cholesterol, while the non-modifiable risk factors involve age, gender, genetic factors, race, and ethnicity (9–12). Interestingly, although age and gender are non-modifiable factors, most of their associated factors are modifiable. Figure 2 represents a model to classify the risk factors of NCDs. The non-modifiable factors can also be classified into three classes: (i) biological factors, such as being overweight, dyslipidemia, hyper-insulinaemia, and hypertension; (ii) behavioral factors, such as diet, lack physical activity, tobacco smoking, and alcohol consumption; and (iii) societal factors, which involve complex combinations of interacting socioeconomic, cultural and environmental parameters (13). In the next section, examples of the identified risk factors for NCDs, including age, diet, and economic context, are highlighted.
Figure 2. A proposed model to classify the risk factors of NCDs.
While NCDs are usually associated with elderly people, all ages are at risk, even before birth. These diseases may start in the earliest years of life and keep progressing during childhood, adolescence, and old age (14). However, 15 million deaths due to NCDs were recorded from people aged between 30 and 69 years of age and more than 82% of these “premature” deaths were from low and middle-income countries (15). The life-course perspective is evidence of the origin of adult NCDs, which are determined in uterus. Barker (16) showed that maternal nutrition plays a significant role in adult diseases. He found that adapting human fetuses to a limited supply of nutrients resulted in permanent structure and metabolism changes. Subsequently, such programmed changes may have attributed to several diseases, such as heart disease, diabetes and hypertension in later life (16, 17). Moreover, unborn babies are not only negatively influenced by maternal habits, such as diet, drug, stress, alcohol and tobacco consumption during pregnancy, but environmental factors, such as air pollution, also have an effect. These factors influence the fetal and early brain development, for example, a low birth weight is attributable to poor long-term health and poor cognition (14, 18).
In the period of childhood, new risks of NCDs may appear due to the easy access to unhealthy food and drinks in kindergartens and schools. Thus, this leads to a high number of overweight and obese children (19). After that stage of life, young people in the adolescence stage can acquire new and harmful habits, such as smoking and drinking alcohol, which can significantly contribute to NCD risk (20, 21). These bad habits may continue during adulthood with additional aspects facing adults in workplaces, including financial stressors, unemployment, unsatisfying careers, and low social engagement, which influence the progress of NCDs (20, 22). Retirement and leaving a workplace can provide new challenges among elderly people and influence the development of NCDs. Poor nutrition, lack of physical activity, alcohol and tobacco use, social isolation, and financial stress directly affect older people and strongly promotes NCDs (20).
The prevention and control of NCDs can be achieved at all ages. The health status of women before and during pregnancy influences the susceptibility of children to NCDs in later life (20, 23). This is the most important strategy to control NCDs because it targets the root of the problem. Applying high standards for food and drinks, increased physical activity in schools and workplaces, in addition to monitoring air quality and offering smoke-free zones can largely prevent NCDs at all stages of life. However, taxation and creating restricted policy for the marketing of unhealthy food, sugary drinks, tobacco, and alcohol can largely improve health statistics. Further, as obese children and elderly people are at a high risk of social isolation, it is important, for their mental and physical health, to be involved in social activities (20, 24).
Diets and Lifestyle
In the past, infectious and parasitic diseases were the main causes of death, but in the recent decades, NCDs have replaced them and have become the main cause of deaths (25). This may be attributed to the change of diet habits and lifestyle over the years, which can be classified as a shift of disease patterns in humans. Various dietary factors, such as meat, whole grain products, healthy dietary patterns, sugar-sweetened beverage consumption, and iron-based diets have an obvious relationship with NCDs (11, 12). Additionally, the high consumption of processed meat and sugar-sweetened beverages, combined with other unhealthy lifestyle factors, such as a high body mass index (BMI), physical inactivity, and smoking have a marked association with NCDs (26, 27). Whole-grain products are independent of the BMI and have protective effects, due to their high fiber contents and ability to slowly release glucose into circulation; subsequently, this reduces the postprandial insulin response and may improve insulin sensitivity (26, 28–31).
Dietary transition describes the changes in production, processing, availability, dietary consumption, and energy expenditure. Further, the concept becomes wider and involves body composition, anthropometrical parameters, and physical activity (32, 33). The use of dietary transition terms arises due to the shift to western diets in developing countries in particular. Traditional food in most countries is healthier, natural, and richer in fiber, and cereal has been replaced by unhealthy processed food that is rich in sugars and fats, animal-source foods, and refined carbohydrates. Hence, low and middle-income countries have seen rapid changes in nutrition transition and rapid increases in NCDs (34). High food consumption and declining physical activity rates occur simultaneously, resulting in NCDs. The main factor, attributable to physical inactivity, is the rapid and continuous development in technology. The easy access to modern technology and manufacturing in houses and workplaces, including machines, vehicles and labor-saving technology, make life easier but unhealthier from the perspective of reducing the risk of NCDs (34).
The Economic Context
NCDs are already common in developed countries and rapidly propagate. Spreading western lifestyle in low and middle-income countries, due to global population aging and commercial pressures for unhealthy diets and cigarettes, contributes to the increasing rate of NCDs in these countries (35). There is a direct relationship between poor health and low-income, which contributes to food poverty, purchasing of cheaper and unhealthy dietary products, and expensive treatments, in addition to psychosocial factors. People with low-incomes have the feeling that they occupy a lower status in society, which prevents them from participating in social life (36). However, food poverty, poor mobility and lack of physical activity are also serious problems in high-income countries (37).
There is a growing trend to consider social, political, and economic systems as critical factors that impact NCDs besides individual behavior/lifestyle (38, 39). Krieger’s Ecosocial theory highlights ecosocial disease distribution which describes how diversity between historical, societal, and ecological conditions significantly contributes to changes in the health outcomes of various social groups (39). For example, the bad side of economic and health inequality that already exists for many years becomes obvious with the current coronavirus COVID-19 pandemic. According to Krieger’s research, the higher number of COVID-19 deaths in African American than whites in the US is attributed to several factors involve living in crowded places, using public transportation to commute to work, working in service jobs in close contact with others, and shortage of protective equipment at workplaces. Furthermore, the lack of access to health care and health insurance, and pre-existing health conditions may be increased the risk from COVID-19 in the African American population (40).
Key Diseases
Cardiovascular Diseases (CVDs)
CVDs are the leading contributors to the global burden of disease among the NCDs and account for the most deaths worldwide each year—even more than the number of deaths from cancer and chronic respiratory diseases combined (41, 42). CVDs are a group of disorders that are not only related to heart conditions, such as ischaemic heart disease (IHD), stroke, congenital heart disease, coronary heart disease, cerebrovascular disease, peripheral arterial disease, and rheumatic heart disease, but also to blood vessels that involve hypertension, and conditions associated with cerebral, carotid, and peripheral circulation (43). While CVDs equally affect both sexes, men suffer from higher incidences than women. Still, CVDs are the leading cause of death of women in developed countries (44). Moreover, many epidemiological studies show the relationship between periodontal disease (PD) and cardiovascular disease. Mild forms of PD affect 75% of adults in the US, and more severe forms affect 20 to 30% of adults. Since PD is common, it is responsible for a significant proportion of proposed infection-associated risks of cardiovascular diseases (45, 46).
According to the American Heart Association, there are seven key health factors and behaviors that contribute to the increasing risks of heart disease and stroke: nutrition, smoking, overweight/obesity, physical inactivity, uncontrolled blood pressure, elevated levels of cholesterol, and blood sugar (42).
Most CVDs can be prevented by addressing the seven risk factors, which involves healthy diets, regular physical activity, avoiding smoking and second-hand smoking, reaching and maintaining a healthy weight, and keeping blood pressure, cholesterol, and blood sugar levels under control (42).
Cancer
Cancer is the main public health problem and the second main cause of death globally [who]. It shares the common risk factors with other key diseases of NCDs and several identified and unidentified factors can be attributed to cancer. The causes of cancer can be classified into three categories, including: (i) biological carcinogens (e.g., viral, bacterial, or parasites infections, hormonal and genetics factors); (ii) chemical carcinogens (such as food and water contamination, and tobacco smoking); and (iii) physical carcinogens (such as ultraviolet and ionizing radiation). However, tobacco smoking is considered to be the main cause of cancer, followed by poor diets (47–49). Moreover, together, body weight and lack physical activity are also associated with the most common cancers, including breast (postmenopausal), colon, endometrium, kidney, and esophagus cancers (50). According to WHO report in 2018, the most common cancers are lung, breast, colorectal, prostate, skin, and stomach, while the most cancer deaths are from cancer of the lung, colorectal, stomach, liver, and breast (48). A noticeable decrease in the cancer death rates of lung, breast, colon/rectum, and prostate is achieved in high-income countries, but are still high in low and middle-income countries (51). Further, the incidence of several cancers, including lung, breast, prostate, colon, and rectum, is commonly elevated concurrently with economic development. In contrast, the incidence of stomach cancer declines with economic development (48). The guidelines for oncological disease prevention and early detection are based on cancer risk assessment, including past medical history, lifestyle factors, family diseases history, and genetic testing (10).
Lung cancer, which is the most common cancer in the world, is mainly the result of smoking and the risk increases in heavy smokers (52). Further, several studies reported low intakes of fruits, vegetables and related nutrients in lung cancer patients (53, 54). Hence, it is possible to prevent lung cancer by stopping the prevalence of smoking and by increasing fruit and vegetable consumption. Furthermore, dietary habits and physical activity contribute to breast cancer, which is the second most common cancer in the world and the most common cancer among women. Excess adiposity and hormonal mechanisms appeared to play key roles in breast cancer progress, and are effected by dietary intake during childhood and adolescence (51, 55, 56). Hence, maintaining a healthy weight throughout life can minimize the chances of breast cancer. Another type of cancer that is strongly associated with diet is colorectal cancer. High intakes of meat and fat, and low intakes of fruits and vegetables, dietary fiber, vitamins and minerals are related to an increased risk of colorectal cancer (57). Hence, minimizing or stopping the consumption of meat, especially preserved meats, can reduces the risk of this cancer. Stomach cancer was the main cause of mortality globally, but is currently decreasing in industrialized countries. It is associated with dietary habits and vitamin C intake (48). Helicobacter pylori infection is considered to be a type I carcinogen and as the strongest known risk factor of gastric cancer (58). Cancers caused by infections are three times lower in developed countries than in developing ones. It is important to avoid the infection in order to prevent cancer, and that can be achieved by eating food that is properly prepared, drinking water from clean sources, taking vitamins according to the recommended dietary allowance, and avoiding the extensive use of antibiotics in order to reduce antibiotic resistant strains (51).
Chronic Respiratory Diseases (CRDs)
CRDs cover a wide range of diseases in the airways and the other structures of the lungs. Most of the morbidity and mortality of CRDs is increased with age. CRDs include chronic obstructive pulmonary disease (COPD), occupational lung diseases, asthma and respiratory allergies, sleep apnoea syndrome, and pulmonary hypertension. Asthma and COPD account for most of the deaths among CRDs in low and middle-income countries (59–61). Genetic and environmental factors are the risk factors of CRDs; environmental factors are more dominant. These factors include air pollution exposure, including tobacco smoke and second-hand tobacco smoke, indoor and outdoor air pollution, occupational exposures, and socioeconomic factors (62, 63).
CRDs are not fully reversible and are partially preventable (64). During pregnancy, maternal smoking contributes to lung dysfunction in children at birth. Further, in early life, a child’s health affects their subsequent respiratory health. Thus, following a healthy lifestyle in the early ages of life, avoiding respiratory infections, and avoiding environmental and occupational agents can effectively prevent CRDs. Preventing exposure to indoor and outdoor pollutants can be achieved by filtration and ventilation, in addition to the use of natural gas (27).
Diabetes Mellitus
Diabetes has attracted global attention due to its elevating prevalence and incidence. It is not only a chronic disease, but also an acutely life-threatening condition. Further, it may cause other serious diseases such as heart diseases, kidney failure, and eye damage, which may subsequently lead to blindness, and foot ulcers, which may require limb amputation. The main two types of diabetes are both lead to hyperglycemia. In type 1, the pancreatic β-cells cannot produce a sufficient amount of insulin, while in type 2, the body cells cannot respond properly to insulin (64). Other types of diabetes involve gestational diabetes mellitus, which occurs in pregnant women with glucose intolerance (65), and type 3 diabetes, which is associated with Alzheimer’s disease, where neurons in the brain cannot respond to insulin (66). While diabetes can be partially inherited, several lifestyle factors, such as obesity, high sugar consumption, and lack of physical activity can significantly contribute to the progress diabetes. However, lifestyle changes can prevent diabetes and the long-term complications of diabetes. Patients with type 2 diabetes can control or even reverse the diabetes by changing their lifestyle and eating habits. The term “healthy dietary pattern” includes a variety of diets and nutritional factors, for example, reducing the consumption of red and processed meat, sugar-sweetened beverages and alcohol, while increasing the consumption of whole-grain products (67).
Management of Risk Factors and NCDs
The following sections outline the developed and proposed strategies to manage NCDs and their risk factors from several perspectives.
Management of Risk Factors
The most common causes of NCDs are metabolic and behavioral risk factors and can be largely preventable by several available means. Most global discussions concern the risk factors of self–management (tobacco and alcohol consumption, physical activity, weight, food, and dental health care) and focus on the role of individual responsibility to manage the risk factors of NCDs. Health care specialists should educate patients about their nutrition value and raise the profile of didactics, practicums, and workshops in daily practice (68). Further, the management of NCDs is the priority of the public health sector in most countries, because management in society is the main direction of NCD prevention strategies. Interventions are used in public health management in an effort to promote good health behavior. For example, India, with its wide sociocultural, economic, and geographical diversity, is implementing multi-sectoral (partnership between different sectors) actions to prevent NCDs, including school health programs, initiatives of National Cancer Control Programme, National Trauma Control program, National Program for Control of Blindness, National Mental Health Programme, the National Tobacco Control Program, and the National Program for Control of Diabetes, Stroke, and Cardiovascular Diseases initiatives (69). From another approach, researchers also highlight the environmental factors (air pollution, climate changes, sunlight) and their impact on NCD development. Air pollution will be an important challenge in the future and new technologies, such as microchips, will have more of an impact in air monitoring (27).
Since diet is a common risk factor among most NCDs, it attracts more attention in an effort to find effective strategies to provide healthy food to the community and at all stages of life. Evidence-based nutrition interventions should be a global health priority and the role of the dietary fat studied should be a modifiable variable in the prevention of NCDs (29). Recent evidence suggests that a diet that is high in healthy fat and rich in unsaturated fatty acids prevents the development of metabolic diseases and reduces cardiovascular events (29). Many interventions addressing poverty and development have an impact on NCD prevalence and risk (69). The current evidence is limited to diets, and a positive effect of agricultural-based food security programs on diet indicators has been suggested (7). A suboptimal diet is the leading risk factor for NCDs and consumption of specific foods, rather than macronutrients or micronutrients; it may be the most significant risk factor for NCDs (70). Strategic health communication in the population-wide intervention includes engaging the food industry in order to reduce the salt content in foods (71). The concept of a sustainable diet combines health and environmental concerns and includes the abovementioned risk factors as part of the recommendations to reduce processed meat consumption and to increase whole-grain consumption (72). Lifestyle activities include healthy diets and focus on limiting the use of salt, sugar, and saturated fats (73). While our body can synthesize many of the molecules required to function properly, essential nutrients are obtained from food. Carbohydrates, proteins, and fats are the primary components of food. Minerals are inorganic essential nutrients that must be obtained from food. The omega−3 alpha-linolenic and the omega−6 linoleic acids are essential fatty acids that are needed to make some membrane phospholipids. Vitamins (B, C, A, D, E, and K) are the classes of essential organic molecules (such as cofactors) that are required in small quantities for most enzymes to function properly. The absence or low levels of vitamins can have a dramatic effect on health. A focus on the need to meet adequate dietary intakes of essential nutrients (74) through a healthy diet is considered to be very significant for the aging society (74). Food supplements are concentrated sources of nutrients (minerals and vitamins) or other substances with a nutritional or physiological effect, which are marketed in the form of pills, capsules, and/or liquids (Table 1). These dietary supplements offer many benefits, including the maintaining of an adequate intake of certain nutrients, to correct nutritional deficiencies, or to support specific physiological functions. Recently, researchers have been looking for new solutions to implement an efficient food production process and to discover the benefits of starch waste on human health.
Table 1. Types of food supplements.
Management of NCDs
A dramatic decrease in all cardiovascular disease-related deaths has been recorded in high-income countries, whereas a significant increase was registered in low and middle-income countries (93, 94). Checkley et al. reported on NCDs’ management in low and middle-income countries (95). While some people in these countries can access the same treatments that are available in high-income countries, the majority of the population lacks access. The main obstacle causes an increase in the number of patients with NCDs in low and middle-income communities is the absence of a well-designed plan to stop disease occurrence and spreading. Each country needs to prepare its management plan, not just with coping models from high-income countries. Several successful models have been verified, taking into consideration the low-cost strategies to prevent, diagnose and treat NCDs. For example, a cost-effective strategy has been developed in Kenya to diagnose diabetes and hypertension in the early stages of life. While health workers are visiting homes to examine human immunodeficiency virus (HIV) infection, they also measure blood glucose levels and blood pressure. Further, type 2 diabetes is a global pandemic that highly affects human health and global economic development (96). The International Diabetes Federation reported that there were 415 million people living with type 2 diabetes in 2015, and estimated that the number by 2040 might increase to 642 million, which is attributable to genetic and environmental factors (96). The genetic–environmental interaction induces insulin resistance and β-cell dysfunction (96). The epidemic of type 2 diabetes in recent decades has not only attributed to the alteration of the gene pool, but environmental changes also play significant roles in the rapid increase in the prevalence of type 2 diabetes (96). However, global diabetes mellitus epidemics require the looking for innovative approaches to prevention (7).
Contemporary Prevention Strategy of NCDs
The prevention strategies of NCDs can include small and large-scale human cooperation (Figure 3). The importance of preventing NCDs arises from the direct impact of NCDs on the decreasing rate of national income. Loss productivity on a large-scale is the result of the inability to work and the frequent absence threats to the national economy. The management strategy to prevent NCDs is based on risk factor management that addresses individual, society, country, and global levels, with actions, such as resource allocation, multi-sectoral partnership, knowledge and information management and innovations. The most critical dimension of the prevention strategy is lifestyle management at the individual level and with a focus on actions, such innovations, which can help the society to increase the awareness of risk factors management, to take health policy decisions at a country level and to develop a health strategy at the global level. The importance of leadership for the change management process is underscored and requires the creation of new approaches to the prevention of NCDs (96, 97).
Figure 3. The proposed prevention management of NCDs with small and large-scale human cooperation.
At the global level, WHO and UN agencies can work together to design policies and strategies to reduce the risk of NCDs (98, 99). It is important to monitor NCDs and to assess their progress at the national, regional and global levels. These organization can support research and encourage collaborations among national and international health agencies and academic institutions. Further, tobacco smoke, as a common factor of the four main types of NCDs, must be put under control. The WHO offers help to smokers who have the desire to stop using tobacco products and to implement rules to propose a smoke-free environment. Further, WHO can, by law, protect tobacco control policies from the commercial interests of the tobacco industry. At the country level, each government needs to design its plan based on its economy. Several low-cost and highly effective strategies are available to prevent and manage NCDs (100–103). For example, encouraging people to play sports for physical activity is the most effective factor that can easily influence the prevention of NCDs, and at the same it is time and cost-effective. Moreover, improved budgetary allocations to support primary health care systems should be put in place in order to provide health services to all community members. To achieve large-scale progress, collaboration between governments and various non-governmental organizations, schools, and universities, to provide advice on lifestyle modifications and to warn people about the risks of NCDs, is in high demand. At the society level, research centers and institutes can significantly contribute to the prevention of NCDs by conducting research projects and programs. Focusing research on food biotechnology and agriculture has a direct influence on NCDs risk (7, 104). The development of diagnostic tools allows for the rapid detection of NCDs biomarkers with high sensitivity to help detect diseases at their early stages, which subsequently contributes to easier treatment and fast cures (105–107). However, in order to reach the highest attainable standard of health, it is important to encourage individuals and families to follow a healthy lifestyle in order to get an effective response for prevention and the control of NCDs and to improve health outcomes (100, 108).
Conclusions
In modern society, NCDs are the main challenge in health systems. Risk factor management is essential in NCDs’ management. The management of NCDs requires many strategies from several perspectives and on different levels, including the individual and country levels. Based on the hypotheses that were raised during the above scientific discussion, it can be concluded that modern strategies for the management of NCDs should be oriented toward the individual level, where the individual is responsible for their health by simply following a healthy lifestyle. It is important to combine modern scientific achievements and innovative decisions, with regard to the rationality of nutrition and positive effects on human health. Governments and international organizations should make people aware of their health and their environment to make the world a safe and healthy place. From another perspective, support research to find new techniques to improve food biotechnology is in high demand. Further, finding rapid and sensitive diagnostic platforms to detect NCDs at the point-of-care offers huge benefits to personnel and the healthcare system. The innovations are vital to address the growing crisis of NCDs successfully, and most often use lifestyle projects, the promotion of healthy eating behaviors and smoking cessation. We believe that there is a need to look for further innovations to build better lives in society.
Author Contributions
The manuscript was prepared by AB, SD, and RK. Writing review and editing was done by AB, SD, DS, KO, PS-G, GP, AK, SK, and RK. Final revision and approval was done by RK. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by the European Regional Development Fund according to the supported activity Attracting scientists from abroad to carry out research (RK) under Measure No. 01.2.2-LMT-K-718 (project No. 01.2.2-LMT-K-718-02-0012).
Conflict of Interest
KO was employed by the company Procomcure Biotech, GmbH.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. World Health Organization. Noncommunicable Diseases (NCD). (2019). Available online at: https://www.who.int/gho/ncd/mortality_morbidity/en/ (accessed January 03, 2020).
2. World Health Organization. Global Action Plan: For the Prevention and Control of Non-communicable Diseases. (2013–2020). Available online at: https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf (accessed January 13,2020).
3. Noor NAM, Yap SF, Liew KH, Rajah E. Consumer attitudes toward dietary supplements consumption: implications for pharmaceutical marketing. Int J Pharm Healthc Mark. (2014) 8:6–26. doi: 10.1108/IJPHM-04-2013-0019
4. Sithey G, Li M, Thow MA. Strengthening non–communicable disease policy with lessons from Bhutan: linking gross national hapiness and health policy action. J Public Health Policy. (2018) 39:327–42. doi: 10.1057/s41271-018-0135-y
5. Goetzke BI, Spiller A. Health-improving lifestyles of organic and functional food consumers. Brit Food J. (2014) 116:510–26. doi: 10.1108/BFJ-03-2012-0073
6. Yang ZY, Yang Z, Zhu L, Qiu C. Human behaviors determine health: strategic thoughts on the prevention of chronic non-communicable diseases in China. Int J Behav Med. (2011) 18:295–301. doi: 10.1007/s12529-011-9187-0
7. Pullar J, Allen L, Townsend N, Williams J, Foster C, Roberts N, et al. The impact of poverty reduction and development interventions on non-communicable diseases and their behavioural risk factors in low and lower-middle income countries. a systematic review. PLoS ONE. (2018) 13:e0193378. doi: 10.1371/journal.pone.0193378
8. Na L, Wu X, Feng R, Li J, Han T, Lin L, et al. The harbin cohort study on diet, nutrition and chronic non communicable diseases: study design and baseline characteristics. PLoS ONE. (2015) 10:e0122598. doi: 10.1371/journal.pone.0122598
9. International Diabetes Federation. IDF Diabetes Atlas. 7th Edn. Brussels: International Diabetes Federation (2015).
10. Kahn SE, Cooper ME, Del PS. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet. (2014) 383:1068–83. doi: 10.1016/S0140-6736(13)62154-6
11. Aune D, Ursin G, Veierød MB. Meat consumption and the risk of type 2 diabetes: a systematic review and meta-analysis of cohort studies. Diabetologia. (2009) 52:2277–87. doi: 10.1007/s00125-009-1481-x
12. Imamura F, O’Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, et al. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ. (2015) 351:h3576. doi: 10.1136/bmj.h3576
13. World Health Organization Technical Report Series. Diet, Nutrition and the Prevention of Chronic Diseases. Geneva: WHO (2003). p. 1–149.
14. Fair Society. Healthy Lives: Strategic Review of Health Inequalities in England Post 2010. London, UK: Marmo Review (2010).
15. World Health Organization. Noncommunicable Diseases: Key Facts. (2018). Available online at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
16. Barker DJP. In utero programming of chronic disease. Clin Sci. (1998) 95:115–28. doi: 10.1042/cs0950115
17. Gluckman PD, Hanson MA. Adult disease: echoes of the past. Euro J Endocrin. (2006) 155 (Suppl. 1):S47–50. doi: 10.1530/eje.1.02233
18. Jefferis BJMH, Power C, Hertzman C. Birth weight, childhood socioeconomic environment, and cognitive development in the 1958 British birth cohort study. BMJ. (2002) 325:305. doi: 10.1136/bmj.325.7359.305
19. Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. (1998) 101 (Suppl. 2):518–25.
20. Mikkelsen B, Williams J, Rakovac I, Wickramasinghe K, Hennis A, Shin HR, et al. Life course approach to prevention and control of non-communicable diseases. BMJ. (2019). 364:l257. doi: 10.1136/bmj.l257
21. Pechmann C, Levine L, Loughlin S, Leslie F. Impulsive and self-conscious: adolescents’ vulnerability to advertising and promotion. J Public Policy Mark. (2005) 24:202–21. doi: 10.1509/jppm.2005.24.2.202
23. World Health Organization. (2016). Good Maternal Nutrition the Best Start in Life. WHO. Available online at: http://www.euro.who.int/__data/assets/pdf_file/0008/313667/Good-maternal-nutrition-The-best-start-in-life.pdf?ua=1 (accessed January 13, 2020).
24. Billingsley M. New advice on physical activity aims to prevent chronic disease from early years. BMJ. (2016) 343:d4457. doi: 10.1136/bmj.d4457
25. Martorell R, Kettel Khan L, Hughes ML, Grummer-Strawn LM. Overweight and obesity in preschool children from developing countries. Int J Obesity. (2000) 24:959–67. doi: 10.1038/sj.ijo.0801264
26. Stein CJ, Colditz GA. Modifiable risk factors of cancer. Br J Cancer. (2004) 90:299–303. doi: 10.1038/sj.bjc.6601509
27. Schultze F, Gao X, Virzonis D, Damiati S, Schneider MR, Kodzius R. Air quality effects on human health and approaches for its assessment through microfluidic chips. Genes. (2017) 8:244. doi: 10.3390/genes8100244
28. Kumar A. The impact of obesity on cardiovascular disease risk factor. Asian J Med Sci. (2019) 10:21294. doi: 10.3126/ajms.v10i1.21294
29. Billingsley HE, Carbone S, Lavie CJ. Dietary fats and chronic noncommunicable diseases. Nutrients. (2018) 10:1385. doi: 10.3390/nu10101385
30. Katileviciute A, Plakys G, Budreviciute A, Onder K, Damiati S, Kodzius RA. Sight to wheat bran: high value-added products. Biomolecules. (2019) 9:887. doi: 10.3390/biom9120887
31. WHO/FAO. Diet, Nutrition and the Prevention of Chronic Diseases. Draft Joint WHO/FAO Consultation on Diet Nutrition and the Prevention of Chronic Disease. (2003). Available online at: https://www.who.int/dietphysicalactivity/publications/trs916/en/ (accessed January 13, 2020).
32. WHO. (2002). The World Health Report 2002. Geneva: WHO.
33. Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nut Rev. (1997) 55:31–43. doi: 10.1111/j.1753-4887.1997.tb01593.x
34. Popkin BM. Nutrition transition and the global diabetes epidemic. Curr Diab Rep. (2015) 15:64. doi: 10.1007/s11892-015-0631-4
35. The Lancet Global Health. Getting to the heart of non-communicable diseases. (2018) 6:e933. doi: 10.1016/S2214-109X(18)30362-0
36. Marmot M. Social causes of social inequalities in health. In: Anand S, Fabienne P, Sen A, editors. Public Health, Ethics, and Equity. Oxford: Oxford University Press (2004). p. 37–46.
37. Lundberg O, Åberg YM, Stjärne M, Björk L, Fritzell J. The Nordic Experience: Welfare States and Public Health. Stockholm. Centre for Health Equity Studies (2008). Available online at: https://www.chess.su.se/polopoly_fs/1.54170.1321266667!/menu/standard/file/NEWS_Rapport_080819.pdf
38. Yang JS, Mamudu HM, John R. Incorporating a structural approach to reducing the burden of non-communicable diseases. Global Health. (2018) 14:66. doi: 10.1186/s12992-018-0380-7
39. Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol. (2001) 30:668–77. doi: 10.1093/ije/30.4.668
40. Krieger N. COVID-19 Pandemic Highlights Longstanding Health Inequities in U.S. Harvard T.H. Chan School of Public Health (2020). Available online at: https://www.hsph.harvard.edu/news/hsph-in-the-news/covid-19-pandemic-highlights-longstanding-health-inequities-in-u-s/ (accessed August 11, 2020).
41. Blundell HJ, Hine P. Non-communicable diseases: ditch the label and recapture public awareness. Int Health. (2019) 11:5–6. doi: 10.1093/inthealth/ihy063
42. World Health Organization. Noncommunicable Diseases: Key Facts. (2018). Available online at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed January 22, 2020).
43. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics−2018 update: a report from the american heart association. Circulation. (2018) 137:e67–492. doi: 10.1161/CIR.0000000000000573
44. Popkin BM, Horton SH, Kim S. The Nutrition Transition and Prevention of Diet-Related Diseases in Asia and the Pacific. Washington, DC: International Food Policy Research Institute (IFPRI) (2001).
45. Brands A, Yach D. NMH Reader. Women and the Rapid Rise of Noncommunicable Diseases. World Health Organization (2002). Available online at: https://apps.who.int/iris/bitstream/handle/10665/67256/WHO_NMH_02.01.pdf;jsessionid=92EE99BB43827D58A0DFDCD7A7E5F5AE?sequence=1 (accessed January 22, 2020).
46. Aune D, Norat T, Romundstad P, Vatten LJ. Whole grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur J Epidem. (2013) 28:845–58. doi: 10.1007/s10654-013-9852-5
47. Fung TT, Hu FB, Pereira MA, Liu S, Stampfer MJ, Colditz GA, et al. Whole-grain intake and the risk of type 2 diabetes: a prospective study in men. Amer J Clin Nutr. (2002) 76:535–40. doi: 10.1093/ajcn/76.3.535
48. Centers for Disease Control and Prevention(US) National Center for Chronic Disease Prevention and Health Promotion(US) Office on Smoking and Health(US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention (2010).
49. Joint WHO/FAO. Expert Consultation on Diet, Nutrition and the Prevention of Chronic Diseases. Geneva, Switzerland (2002). Available online at: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed January 22,2020).
50. Willet MC. Diet, nutrition, and avoidable cancer. Environ Health Perspect. (1995) 103:S165–70. doi: 10.1289/ehp.95103s8165
51. Vainio H, Bianchini F. Weight control and physical activity. In: IARC Handbooks of Cancer Prevention. Vol. 6. Lyon: IARC Press (2002).
52. International Agency for Research on Cancer. Cancer: causes, occurrence and control. In: Thomas L, Aitio O, Day NE, Heseltine E, Kadlor J, Miller AB, Parkin DM, Riboli, editors. Lyon, International Agency for Research on Cancer. Lyon: IARC Scientific Publications (1990).
53. Ferlay J. Globocan 2000: Cancer Incidence, Mortality and Prevalence Worldwide. Version 1.0. Lyon: International Agency for Research on Cancer (2001).
54. Potter J. Food, Nutrition and the Prevention of Cancer: A Global Perspective. Washington, DC: World Cancer Research Fund/American Institute for Cancer Research (1997).
55. Nutritional Aspects of the Development of Cancer. Report of the working group on diet and cancer of the committee on medical aspects of food and nutrition policy. Rep Health Soc Subj. (1998) 48:i–xiv:1–274.
56. Key TJ, Verkasalo PK, Banks E. Epidemiology of breast cancer. Lancet Oncol. (2001) 2:133–40. doi: 10.1016/S1470-2045(00)00254-0
57. Norat T, Lukanova A, Ferrari P, Riboli E. Meat consumption and colorectal cancer risk: a dose–response meta-analysis of epidemiological studies. Int J Cancer. (2002) 98:241–56. doi: 10.1002/ijc.10126
58. Wroblewski LE, Peek RM J, Wilson KT. Helicobacter pylori and gastric cancer: factors that modulate disease risk. Clin Microbio Rev. (2010) 23:713–39. doi: 10.1128/CMR.00011-10
59. Navarro-Torné A, Vidal M, Trzaska DK, Passante L, Crisafulli A, Laang H, et al. Chronic respiratory diseases and lung cancer research: a perspective from the European Union. Eur Resp J. (2015) 46:1270–80. doi: 10.1183/13993003.00395-2015
60. Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global burden of disease study 2015. Lancet. (2016) 388:1459–544. doi: 10.1016/S0140-6736(16)31012-1
61. de-Graft Aikins A, Unwin N, Agyemang C, Allotey P, Campbell C, Arhinful D. Tackling Africa’s chronic disease burden: from the local to the global. Global Health. (2010) 6:5. doi: 10.1186/1744-8603-6-5
62. Bousquet J, Dahl R, Khaltaev N. Global alliance against chronic respiratory diseases. Eur Respir J. (2007) 29:233–9. doi: 10.1183/09031936.00138606
63. Leynaert B, Sunyer J, Garcia-Esteban R, Svanes C, Jarvis D, Cerveri I, et al. Gender differences in prevalence, diagnosis and incidence of allergic and non-allergic asthma: a population-based cohort. Thorax. (2012) 67:625–31. doi: 10.1136/thoraxjnl-2011-201249
64. Bellou V, Belbasis L, Tzoulaki I, Evangelou E. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta-analyses. PLoS ONE. (2018) 13:e0194127. doi: 10.1371/journal.pone.0194127
65. Gilmartin AB, Ural SH, Repke JT. Gestational diabetes mellitus. Rev Obstet Gynecol. (2008) 1:129–34.
66. De la Monte SM, Wands JR. Alzheimer’s disease is type 3 diabetes-evidence reviewed. J Diabetes Sci Technol. (2008) 2:1101–13. doi: 10.1177/193229680800200619
67. Esposito K, Chiodini P, Maiorino MI, Bellastella G, Panagiotakos D, Giugliano D. Which diet for prevention of type 2 diabetes? a meta-analysis of prospective studies. Endocrine. (2014) 47:107–16. doi: 10.1007/s12020-014-0264-4
68. Johnston E, Mathews T, Aspry K, Aggarwal M, Gianos E. Strategies to fill the gaps in nutrition education for health professionals through continuing medical education. Curr Atheroscler Rep. (2019) 21:13. doi: 10.1007/s11883-019-0775-9
69. Arora M, Chauhan K, John S, Mukhopadhyay A. Multi-sectoral action for addressing social determinants of noncommunicable diseases and mainstreaming health promotion in national health programmes in India. Indian J Commun Med. (2011) 36:S43–9. doi: 10.4103/0970-0218.94708
70. Mutie PM, Giordano GN, Franks PW. Lifestyle precision medicine: the next generation in type 2 diabetes prevention? BMC Med. (2017) 15:171. doi: 10.1186/s12916-017-0938-x
71. Micha R, Khatibzadeh S, Shi P, Andrews KG, Engell RE, Mozaffarian D. Global, regional and national consumption of major food groups in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys worldwide. BMJ Open. (2015) 5:e008705. doi: 10.1136/bmjopen-2015-008705
72. Webster J, Pillay A, Suku A, Gohil P, Santos JA, Schultz J, et al. Process evaluation and costing of a multifaceted population-wide intervention to reduce salt consumption in fiji. Nutrients. (2018) 10:155. doi: 10.3390/nu10020155
73. Springmann M, Wiebe K, Mason-D’Croz D, Sulser TB, Rayner M, Scarborough P. Health and nutritional aspects of sustainable diet strategies and their association with environmental impacts: a global modelling analysis with country-level detail. Lancet Planet Health. (2018) 2:e451–61. doi: 10.1016/S2542-5196(18)30206-7
74. Bruins MJ, van Dael P, Eggersdorfer M. The role of nutrients in reducing the risk for noncommunicable diseases during aging. Nutrients. (2019) 11:85. doi: 10.3390/nu11010085
75. USDA. (2020). U.S.D.o.A. Dietary Guidelines and MyPlate. Available online at: https://www.choosemyplate.gov/dietary-guidelines (accessed Feburary 16, 2020).
76. Fletcher RH, Fairfield KM. Vitamins for chronic disease prevention in adults. JAMA. (2002) 287:3127–9. doi: 10.1001/jama.287.23.3127
77. Castiglione D, Platania A, Conti A, Falla M, D’Urso M, Marranzano M. Dietary micronutrient and mineral intake in the mediterranean healthy eating, ageing, and lifestyle (MEAL) study. Antioxidants. (2018) 7:79. doi: 10.3390/antiox7070079
78. Higdon J. An evidence-based approach to vitamins and minerals: health benefits and intake recommendations. United States: Thieme Medical Publishers (2003). 253p.
79. Huskisson E, Maggini S, Ruf M. The role of vitamins and minerals in energy metabolism and well-being. J Int Med Res. (2007) 5:277–89. doi: 10.1177/147323000703500301
80. Damodaran S Parkin KL Fenema OR. Fennema‘s Food Chemistry. Boca Raton, FL: Taylor and Francis Group (2007). 1144p.
81. Wu G. Amino acids: metabolism, functions, and nutrition. Amino Acids. (2009) 37:1–17. doi: 10.1007/s00726-009-0269-0
82. Applegate EA, Grivetti LE. Search for the competitive edge: a history of dietary fads and supplements. J Nutr. (1997) 127:869–73. doi: 10.1093/jn/127.5.869S
83. Helms ER, Aragon AA, Fitschen PJ. Evidence-based recommendations for natural bodybuilding contest preparation: nutrition and supplementation. J Int Soc Sports Nutr. (2014) 11:20. doi: 10.1186/1550-2783-11-20
84. Simopoulos AP. Essential fatty acids in health and chronic disease. Am Clin Nutr. (1999) 70:560–9. doi: 10.1093/ajcn/70.3.560s
85. Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation. (2002) 106:2747–57. doi: 10.1161/01.CIR.0000038493.65177.94
86. Harvey AL. Natural products in drug discovery. Drug Discov Today. (2008) 13:894–901. doi: 10.1016/j.drudis.2008.07.004
87. Dias DA, Urban S, Roessner U. A historical overview of natural products in drug discovery. Metabolites. (2012) 2:303–36. doi: 10.3390/metabo2020303
88. Kaur IP, Chopra K, Saini A. Probiotics: potential pharmaceutical applications. Eur J Pharm Sci. (2002) 15:1–9. doi: 10.1016/S0928-0987(01)00209-3
89. Parvez S, Malik KA, Kang SA, Kim HY. Probiotics and their fermented food products are beneficial for health. J App Microbiol. (2006) 100:1171–85. doi: 10.1111/j.1365-2672.2006.02963.x
90. Curry S, Byers T, Hewitt M. Fulfilling the Potential of Cancer Prevention and Early Detection. Washington DC: National Academy Press (2003).
91. Jhajharia S, Verma S, Kumar R. Risk factors, susceptibility, and machine learning techniques for cancer prediction. Drug Intervent Today. (2018) 10:580–92.
92. Thun MJ, DeLancey JO, Center MM, Jemal A, Ward EM. The global burden of cancer: priorities for prevention. Carcinogenesis. (2010) 31:100–10. doi: 10.1093/carcin/bgp263
93. Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. (2017) 70:1–25. doi: 10.1016/j.jacc.2017.04.052
94. Rarau P, Pulford J, Gouda H, Phuanukoonon S, Bullen C, Scragg R, et al. Socio-economic status and behavioural and cardiovascular risk factors in Papua New Guinea: a cross-sectional survey. PLoS ONE. (2019) 14:e0211068. doi: 10.1371/journal.pone.0211068
95. Checkley W, Ghannem H, Irazola V, Kimaiyo S, Levitt NS, Miranda JJ, et al. Management of NCD in low- and middle-income countries. Glob Heart. (2014) 9:431–43. doi: 10.1016/j.gheart.2014.11.003
96. International Diabetes Federation. IDF Diabetes Atlas. 7th ed. Brussels: International Diabetes Federation (2015).
97. World Health Organization (WHO). Global Action Plan for the Prevention and Control of NCDs 2013-2020. (2013). Available online at: https://www.who.int/nmh/events/ncd_action_plan/en/ (accessed January 22, 2020).
98. Lim J, Chan MM, Alsagoff FZ, Ha D. Innovations in non-communicable diseases management in ASEAN: a case series. Glob Health Action. (2014) 7:25110. doi: 10.3402/gha.v7.25110
99. World Health Organization (WHO). Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low-resource Settings. (2010). Available online at: https://www.who.int/nmh/publications/essential_ncd_interventions_lr_settings.pdf (accessed January 22,2020).
100. Rogge J. Statement by Dr Jacques Rogge. In: Proceedings of High-level meeting of the UN General Assembly on the Prevention and Control of Non-communicable Diseases, New York, NY: New York (2018).
101. Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. (2012) 380:219–29. doi: 10.1016/S0140-6736(12)61031-9
102. Phillips CM, Chen LW, Heude B, Bernard JY, Harvey NC, Duijts L, et al. Dietary inflammatory index and non-communicable disease risk: a narrative review. Nutrients. (2019) 11:1873. doi: 10.3390/nu11081873
103. Zarocostas J. Need to increase focus on non-communicable diseases in global health, says WHO. BMJ. (2010) 341:c7065. doi: 10.1136/bmj.c7065
104. Francesco R, Anna L, Stineke O, Victor A, Gunhild S, Ruth R, et al. Transforming the food system to fight non-communicable diseases. BMJ. (2019) 364:l296. doi: 10.1136/bmj.l296
105. Damiati S, Küpcü S, Peacock M, Eilenberger C, Zamzami M, Qadri I, et al. Acoustic and hybrid 3D-Printed electrochemical biosensors for the real-time immunodetection of liver cancer cells (HepG2). Biosens Bioelectron. (2017) 94:500–6. doi: 10.1016/j.bios.2017.03.045
106. Damiati S, Peacock M, Leonhardt S, Baghdadi MA, Damiati L, Becker H, et al. Embedded disposable functionalized electrochemical biosensor with a 3D-printed flow-cell for detection of hepatic oval cells. Genes. (2018) 9:89. doi: 10.3390/genes9020089
107. Damiati S, Hersman C, Søpstad S, Peacock M, Whitley T, Davey P, et al. Sensitivity comparison of macro- and micro-electrochemical biosensors for human chorionic gonadotropin (hCG) biomarker detection. IEEE Access. (2019) 7:94048–58. doi: 10.1109/ACCESS.2019.2928132
108. Matheson GO, Klugl M, Engebretsen L, Bendiksen F, Blair SN, Borjesson M, et al. Prevention and management of noncommunicable disease: the IOC consensus statement, Lausanne 2013. Clin J Sport Med. (2013) 23:419–29. doi: 10.1097/JSM.0000000000000038
Keywords: risk factors, non-communicable diseases, health policy, prevention strategies, healthcare-management
Citation: Budreviciute A, Damiati S, Sabir DK, Onder K, Schuller-Goetzburg P, Plakys G, Katileviciute A, Khoja S and Kodzius R (2020) Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Front. Public Health 8:574111. doi: 10.3389/fpubh.2020.574111
Received: 18 June 2020; Accepted: 26 October 2020;
Published: 26 November 2020.
Rosemary M. Caron, University of New Hampshire, United States
Nilesh Chandrakant Gawde, Tata Institute of Social Sciences, India
Iuliana Denetiu, King Abdulaziz University, Saudi Arabia
Copyright © 2020 Budreviciute, Damiati, Sabir, Onder, Schuller-Goetzburg, Plakys, Katileviciute, Khoja and Kodzius. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rimantas Kodzius, kodzius@envirola.com
† These authors have contributed equally to this work