World health network
World health network
World health network
Communities across Europe and the US are engaged in this project focused on empowering parents and teachers to help make schools safer. We work with parents and teachers advocating and engaging in improving school safety and remote options. The effort involves writing and share petitions, write to school and government officials, organize local communities, and engaging with the press.
US: We won’t sacrifice our children. Together, we keep us safe:
«>
The group is looking at applying practical solutions, notably, ventilation, filtration, CO2 monitoring or DIY Air-Cleaners. We’re working on simple and low-cost solutions for higher risk settings (confined, closed spaces, poorly ventilated) that would benefit from such quick, yet safe fixes to Improve Indoor Air Quality and to further minimize risks on top of the other Covid precautions. The task force also investigates procurement, decision making and multiple Do-It-Yourself designs.
This WHN IAQ group is a work-in-progress, an ongoing effort to help parents, teachers, schools or workplaces to materialize DIY airborne precautions to better protect children, staff, families and communities.
«>
«>
World health network
The growth of Monkeypox in 58 countries through local community transmission around the world, with 3,417 confirmed Monkeypox cases reported across 58 countries, and the rate of growth of cases increasing week by week across multiple continents
The severe pain, scaring, blindness, and death, which has been observed in cases of Monkeypox historically.
The greater severity of Monkeypox in children, who have thus far been spared during the current outbreak but are likely to be infected increasingly as community transmission expands.
The danger of transmission to wildlife, including rodents such as mice, rats, squirrels, and domesticated pets, which would become a reservoir that will expand across the world leading to ongoing risk of human infection and the need to modify daily life due to this ongoing risk to avoid exposure in many contexts.
The World Health Network (WHN) declares the monkeypox outbreak a Public Health Emergency of Global Concern, by which it indicates that this outbreak is not limited to a single country or region and should be addressed by immediate actions taken wherever community transmission is taking place in order to ensure that the least effort is needed and the smallest impact is suffered due to this outbreak.
Guidelines for Individuals and Institutions
We have a new wiki that features all of our resources and guidelines that are free for everyone to use and share.
We are a global community devoted to protecting health and minimizing harm to individuals and society formed as a people’s task force in response to the COVID-19 pandemic. We advocate for an effective response to achieve progressive elimination of the disease globally.
The World Health Network includes independent scientific advisory and advocacy teams and citizens’ action initiatives. Our members have guided successful elimination efforts, advised governments, built accessible data platforms, advocated for airborne precautions and school safety, produced scientific consensus documents, and engaged in public communication and community-based efforts to promote individual and public health.
We are independent from any political body or government, though individual members may have such affiliations. We are guided by compassion, scientific rigor, transparency, social responsibility, and value for life, which have been lacking in many pandemic strategies.
Join our community
As an active WHN member, you are connected to scientists and community members who can collaborate to strengthen, leverage and complement your activities. This includes resources, practical tools, and support from others as well as access to our virtual collaborative space. Within the space you can collaborate on projects, join team efforts, attend and host meetings, take part in campaigns addressing current challenges, and connect with the network of like-minded experts and passionate advocates of public health who value human life.
MEMBER ORGANIZATIONS
World Health Network Charter
WHN is a network devoted to the development and execution of science based global, national and local pandemic response. Motivated by compassion, WHN values innovation, new ideas and new members and aspires to excellence, transparency, and trust.
WHN was formed by many cross-disciplinary and country based teams and hundreds of advocates and scientists, to meet the challenge of saving lives, health, livelihoods and liberty.
WHN is organized under the aegis of the New England Complex Systems Institute, a US non-profit 501c3 research and educational institute.
WHN Values
We envision a world in which we, the global community, together save lives, health, livelihoods and liberty.
The world has learned that while outbreaks are inevitable, pandemics are optional.
We know now that early prevention is better than delayed efforts at cure.
We experienced our global organizations and many nations’ leaders lack of preparedness for a predicted global pandemic and then, their inability to adapt to end it, as it progressed.
We can do better. We know how to do better. We will do better. Together. How?
By connecting people in our interdependent world, to collaborate to end this pandemic effectively, and to ensure we are ready for the next.
By creating a space where our individual aspirations to make the world a better place, are harnessed. Where our unique talents, abilities and knowledge are valued and connected to create a powerful tapestry of humanity.
By building trust through telling the truth (authenticity), with logic (integrity) and empathy.
By using care, compassion and success to motivate us, and allowing science to guide us. Science tells us the consequences of our decisions – our actions, policies and strategies.
By knowing that pandemic response starts and ends with communities. That they are mostly sociological (rather than political) or biological.
The world is what we choose to make of it. We dismantle the specific wishful thinking that we can live with deadly viruses. We disagree that the deaths of our elders, our most physically, socially or geographically vulnerable, and our frontline workers are acceptable. We acknowledge those deaths are a result of our collective failure to act – as a lack of care. We show proof that the economy is the people and is not in competition with them.
We will work to reverse this diminishing of the value of life, the sacrifice of loved ones through lack of care, the exploitation of others or their injury, the promotion of misinformation, and distraction from what is important.
World health network
For Immediate Release
NOVEMBER 27, 2021
Global Response to Omicron Variant:
Better but needs to be stronger
November 27, 2021: In response to the new variant outbreak growing in the southern part of the African continent, Europe as a unit, the US and many other countries, have limited travel from South Africa and adjacent countries. The World Health Network thanks South Africa for sounding the alarm and congratulates countries for responding rapidly, much faster and more decisively than with the original spread of the Coronavirus and the successive variants.
The new variant has been rapidly growing in an expanding region of Johannesburg leading to an increase from 1% to 30% in positivity in just two weeks. This increase is likely due to both evasion of prior immunity as well as a higher underlying transmissibility. Locally the effective R value increased from less than 1 to almost 2 in less than a month.
The variant has many more mutations than previous variants, at least 30 of which are reported to be associated with the spike protein, potentially allowing evasion of prior immunity whether due to infection or vaccination. Beta had three mutations in the critical receptor binding area, Delta had two, Omicron has ten.
An infected traveler to Hong Kong is reported to have infected another in a room across the hall. One of two travelers to Belgium came there infected from Egypt. Five infected travelers arriving in Israel included one arriving from Malawi. These travelers included transits in Turkey, Dubai, Ethiopia and Jordan.
Although empirical data is still lacking, Omicron’s extensive mutations imply a high risk that this variant evades vaccine immunity, which would bring us back to square one, but with a much faster spreading virus.
What is to be done to prevent Omicron from spreading?
Given that the Omicron variant may at least partially evade the protection offered by vaccines, it is important that all countries expand public health and social measures to limit COVID-19 transmission. The public must be warned about the importance of public health measures in addition to vaccination to safeguard their own health and family members’.These measures include mask use, ventilation and filtration and other airborne precautions, as well as physical distancing to reduce transmission; and testing and contact tracing to limit the size of clusters.
It is crucial that all countries introduce risk-based border controls. These measures include:
Implementing travel restrictions from all countries with known or suspected cases.
Introducing universal quarantine and at least 2 testings (at arrival and exit) for travel across borders, for example, requiring a minimum 10 days quarantined in a government facility, pre-travel PCR tests, and testing on arrival and during quarantine
Expanding contact tracing to identify all persons who may have come in contact with the traveller since his/her entry through establishment of Omicron specific surveillance
Creating awareness and increased voluntary disclosure of travel to affected countries, especially during the last two weeks, through involvement of Media
South Africa’s early warning should be acknowledged and help should be provided to them with the challenge of responding to the Omicron outbreak.
FOR INFORMATION OR INTERVIEWS, CONTACT
USA: Yaneer Bar-Yam, Founder, World Health Network
USA: Eric Feigl-Ding, New England Complex Systems Institute
USA: Nassim Nicholas Taleb, New York University
France: Cécile Philippe, President, Institut économique Molinari
Germany: Matthias F. Schneider, WHN, Department of Physics, Technical University of Dortmund, Germany,
+ 49 231 744 4139
Iberoamerica: Carlos Gershenson, Universidad Nacional Autónoma de México, info@worldhealthnetwork.global
India: Sunil Raina, Head of the Department of Community Medicine at the Dr. Rajendra Prasad Government Medical College in Himachal Pradesh, India
New Zealand: Michael Baker, Professor of Public Health and Epidemiology, University of Otago, Wellington New Zealand,
Israel: Meir Rubin, Executive Director, Kohelet Policy Forum
Canada: Stephane Bilodeau, WHN Indoor Air Quality Task Force
Taiwan : Shu-Ti Chiou, Founder & President, Health & Sustainable Development Foundation, Taiwan College of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan,
Norway: Gunhild Alvik Nyborg, Covid Action Group, WHN
ABOUT THE WORLD HEALTH NETWORK
The World Health Network (WHN) is a global community devoted to protecting health and minimizing harm to individuals and society. It was formed as a people’s task force in response to the COVID-19 pandemic and includes independent scientific advisory and advocacy teams and citizens’ action initiatives. The WHN is guided by compassion, scientific rigor, transparency, social responsibility, and value for life. The WHN advocates for an effective response to achieve progressive elimination of the disease globally.
World Health Network
The WHN declaration is available on The Lancet
Pour publication immédiate
27 NOVEMBRE 2021
Réponse au variant Omicron:
du mieux mais il faut être plus radical
27 novembre 2021 : En réponse au nouveau variant Omicron découvert dans la partie sud du continent africain, l’Europe dans son ensemble, les États-Unis et de nombreux autres pays ont limité les voyages en provenance d’Afrique du Sud et des pays voisins. Le World Health Network remercie l’Afrique du Sud d’avoir tiré la sonnette d’alarme rapidement et félicite les nombreux pays qui ont réagi de manière beaucoup plus rapide et déterminée que lors des précédents épisodes.
Le nouveau variant se développe ultra rapidement dans la région de Johannesburg. En seulement deux semaines, les taux de positivité y sont passés de 1% à 30%. Cette augmentation est probablement liée à une plus grande capacité de ce variant à échapper à l’immunité naturelle et vaccinale des individus associée à une possible plus grande transmissibilité. Au niveau local, le Ro est passé de moins de 1 à presque 2 en moins d’un mois.
Ce variant est très préoccupant car il présente beaucoup plus de mutations que les variants précédents. Une trentaine d’entre elles seraient associées à la protéine spike, ce qui lui permettrait potentiellement d’échapper aux immunités construites lors des épisodes précédents. Dans la zone critique du domaine de fixation au récepteur (RBD), Beta a 3 mutations, Delta en présente 2, Omicron en a 10.
Un voyageur infecté à Hong Kong et isolé semble avoir pu en infecter une autre résidant dans la chambre en face de la sienne dans l’hôtel quarantaine. Un des deux voyageurs détectés en Belgique était en provenance d’Egypte. Cinq voyageurs infectés sont arrivés en Israël, l’un d’eux venant du Malawi. Ces voyageurs ont notamment transité par la Turquie, Dubaï, l’Éthiopie et la Jordanie.
Bien que les données empiriques fassent encore défaut, les nombreuses mutations que présente Omicron laissent penser que ce variant présente un risque d’échappement important à l’immunité offerte par les vaccins. Si tel était le cas, cela nous ramènerait à la case départ, avec un virus se propageant beaucoup plus rapidement.
Le rétablissement des mesures barrière de base sont essentielles : port du masque, ventialtion, filtration de l’air, distanciation, dépistage et recherche active des contacts.
Dans cette phase critique de découverte d’un nouveau variant « préoccupant », le contrôle aux frontières est clé pour l’empêcher de se propager. Cela implique de :
— Suspendre tous les voyages en provenance de tous les pays où des cas sont connus ou suspectés,
— Réaliser des tests et mettre en quarantaine les voyageurs se déplaçant d’un pays à l’autre, en exigeant par exemple un minimum de 10 jours de quarantaine dans un établissement public à cet effet, des tests PCR avant le voyage et des tests à l’arrivée et pendant la quarantaine,
— Intensifier rapidement la recherche des cas contacts afin d’identifier toutes les personnes susceptibles d’avoir été en contact avec une personne ayant voyagé récemment avec une surveillance spécifique d’Omicron,
— Encourager, en y associant les media, la déclaration volontaire des personnes ayant voyagé au cours des 2 dernières semaines dans les pays touchés.
Il convient aussi de soutenir tous les efforts de l’Afrique du Sud dans sa lutte contre Omicron dont elle a eu le courage d’alerter rapidement le monde entier.
POUR TOUTE INFORMATION OU INTERVIEW, CONTACTEZ
USA : Yaneer Bar-Yam, fondateur, World Health Network
USA: Eric Feigl-Ding, New England Complex Systems Institute
USA: Nassim Nicholas Taleb, New York University
Allemagne : Matthias F. Schneider, Département de physique, Université technique de Dortmund, Allemagne, matthias-f.schneider@tu-dortmund.de.
+ 49 231 744 4139
France : Cécile Philippe, Présidente, Institut économique Molinari
Ibéro-Amérique : Carlos Gershenson, Universidad Nacional Autónoma de Mexico, info@worldhealthnetwork.global
Inde : Sunil Raina, chef du département de médecine communautaire du Dr. Rajendra Prasad Government Medical College à Himachal Pradesh, en Inde. info@worldhealthnetwork.global
Nouvelle-Zélande : Michael Baker, professeur de santé publique et d’épidémiologie, Université d’Otago, Wellington Nouvelle-Zélande.
Israël : Meir Rubin, directeur exécutif, Kohelet Policy Forum.
Canada: Stephane Bilodeau, Groupe sur la qualité de l’air intérieur du WHN
Taiwan : Shu-Ti Chiou, Founder & President, Health & Sustainable Development Foundation, Taiwan College of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan
Norway: Gunhild Alvik Nyborg, Covid Action Group, WHN
À PROPOS DU WORLD HEALTH NETWORK
Le WHN est une communauté internationale qui se consacre à la protection de la santé et à la réduction des dommages causés aux individus et à la société. Le WHN est guidé par la compassion, la rigueur scientifique, la transparence, la responsabilité sociale et la valeur de la vie. Le WHN plaide pour une réponse efficace afin de parvenir à l’élimination progressive de la maladie dans le monde. Il s’est formé pour répondre efficacement à la pandémie de COVID-19 et comprend aussi bien des scientifiques indépendants que des groupes d’initiative citoyennes.
The World Health Network
La déclaration du WHN a été publiée dans The Lancet.
Para su publicación inmediata
27 de noviembre, 2021
Respuesta Global a la Variante Omicron:
Positiva, pero necesita ser más fuerte
27 de noviembre, 2021: En respuesta al nuevo brote de la variante Omicron que ha estado creciendo en el sur del continente africano, Europa en su conjunto, EEUU y varios países más han limitado los viajes desde Sudáfrica y otros países cercanos. La Red Mundial de la Salud agradece a Sudáfrica por haber comunicado la alarma y felicita a los países que han respondido de manera veloz, mucho más rápido y más decisivamente que con la propagación inicial del coronavirus y sus variantes sucesivas.
La nueva variante ha estado creciendo rápidamente en una región que incluye a Johannesburgo, teniendo un aumento del 1% al 30% de positividad en tan solo dos semanas. Este incremento probablemente se deba tanto a la evasión de inmunidad previa como a una mayor transmisibilidad. Localmente, la R efectiva se incrementó de menos de 1 a casi 2 en menos de un mes.
La variante Omicron tiene muchas más mutaciones que las variantes previas, por lo menos 30, que se reporta que están asociadas con la proteína pico, potencialmente permitiendo la evasión de inmunidad previa, ya sea por infección o vacunación. La variante Beta tenía tres mutaciones en el área crítica de unión al receptor, Delta tenía dos, Omicron tiene diez.
Se ha reportado que un viajero a Hong Kong infectado contagió en un hotel a otro que estaba en un cuarto del otro lado del pasillo. De dos viajeros a Bélgica, uno llegó infectado de Egipto. Cinco viajeros infectados llegando a Israel incluyen a uno llegando de Malawi. Estos viajeros hicieron escalas en Turquía, Dubai, Etiopía y Jordania.
Aunque todavía hacen falta datos empíricos, las mutaciones extensivas de Omicron implican un riesgo alto de que esta variante evada la inmunidad por vacunas, lo cual nos regresaría al inicio de la pandemia, pero con un virus que se propaga mucho más rápido.
¿Qué se debe hacer para prevenir que se propague la variante Omicron?
Dado que la variante Omicron podría evadir por lo menos parcialmente la protección ofrecida por vacunas, es importante que todos los países amplíen las medidas de salud pública y sociales para limitar la transmisión de COVID-19. El público debe ser advertido sobre la importancia de estas medidas adicionales a la vacunación para salvaguardar su salud y la de sus familias. Estas medidas incluyen el uso de mascarillas; ventilación, filtración de aire y otras precauciones de transmisión aérea; distanciamiento físico para reducir transmisión y pruebas y rastreo.
Es crucial que todos los países implementen controles de fronteras basados en riesgos. Estas medidas incluyen:
Restricciones de viaje de todos los países con casos conocidos o sospechosos.
Introducir cuarentena universal y por lo menos dos pruebas (al llegar y al salir) para viajes entre fronteras. Por ejemplo, requiriendo 10 días mínimo de cuarentena, pruebas PCR antes de viajar y pruebas al llegar y durante la cuarentena.
Expandir el rastreo de contactos para identificar a todas las personas que pudieron haber estado en contacto con los viajeros desde su entrada a través del establecimiento de una vigilancia específica para Omicron.
Crear conciencia y aumentar la divulgación voluntaria de quienes han viajado a los países afectados, especialmente durante las últimas dos semanas, involucrando a medios.
La alerta temprana de Sudáfrica debe de ser reconocida y se les debe de proporcionar ayuda para responder al reto del brote de Omicron.
PARA INFORMACIÓN Y ENTREVISTAS, CONTACTAR
EEUU: Yaneer Bar-Yam, Fundador, World Health Network
EEUU: Eric Feigl-Ding, New England Complex Systems Institute
EEUU: Nassim Nicholas Taleb, New York University
Francia: Cécile Philippe, Presidenta, Institut économique Molinari
Alemania: Matthias F. Schneider, Departamento de Física, Universidad Técnica de Dortmund matthias-f.schneider@tu-dortmund.de
+ 49 231 744 4139
Iberoamérica: Carlos Gershenson, Universidad Nacional Autónoma de México, info@worldhealthnetwork.global
India: Sunil Raina, Jefe del Departamento de Medicina Comunitaria en el Colegio Gubernamental de Medicina Dr. Rajendra Prasad en Himachal Pradesh, India
Nueva Zelanda: Michael Baker, Profesor de Salud Pública y Epidemiología, Universidad de Otago, Wellington,
Israel: Meir Rubin, Director Ejecutivo, Kohelet Policy Forum
Canadá: Stephane Bilodeau, WHN Indoor Air Quality Task Force
Taiwan : Shu-Ti Chiou, Fundadora y Presidenta, Health & Sustainable Development Foundation, Taiwan College of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan
Noruega: Gunhild Alvik Nyborg, Covid Action Group, WHN
SOBRE LA RED MUNDIAL DE LA SALUD
La Red Mundial de la Salud (World Health Network, WHN) es una comunidad global dedicada a proteger la salud y minimizar el daño a individuos y sociedades. Fue formada como una grupo de trabajo popular en respuesta a la pandemia por COVID-19 e incluye equipos independientes de asesoría y abogacía científica y de iniciativas de acción ciudadana. La WHN está guiada por compasión, rigor científico, transparencia, responsabilidad social y valor por la vida. La WHN aboga por una respuesta efectiva para alcanzar una eliminación progresiva de la enfermedad a nivel global.
World Health Network
La declaración de la WHN está disponible en The Lancet
Pressemitteilung
27. November 26, 2021
Globale Reaktion auf die Omicron-Variante:
Verbesserungen ja, aber noch konsequenteres Handeln erforderlich
27. November 2021: Als Reaktion auf den Ausbruch der neuen Variante, die sich im südlichen Teil des afrikanischen Kontinents ausbreitet, haben die europäische Union, die USA und viele andere Länder Reisen aus Südafrika und den angrenzenden Ländern eingeschränkt. The World Health Network (WHN) dankt Südafrika dafür, dass es Alarm geschlagen hat, und beglückwünscht die Länder dazu, dass sie rasch, viel schneller und entschlossener als bei der ursprünglichen Ausbreitung des Coronavirus und der nachfolgenden Varianten reagiert haben.
Die neue Variante hat sich in einer expandierenden Region von Johannesburg rasch ausgebreitet, was zu einem Anstieg der positiven Ergebnisse von 1 % auf 30 % in nur zwei Wochen führte. Dieser Anstieg ist wahrscheinlich sowohl auf die Umgehung einer früheren Immunität (sogenannte escape) als auch auf eine höhere zugrundeliegende Übertragbarkeit zurückzuführen. Auf lokaler Ebene stieg der effektive R-Wert in weniger als einem Monat von weniger als 1 auf fast 2.
Die Variante weist viel mehr Mutationen auf als frühere Varianten, von denen mindestens 30 mit dem Spike-Protein in Verbindung gebracht werden, was möglicherweise eine Umgehung der Immunität aufgrund einer Infektion oder Impfung ermöglicht. Beta hatte drei Mutationen im kritischen Rezeptorbindungsbereich, Delta zwei und Omicron zehn.
Ein infizierter Hongkong-Reisender hat Berichten zufolge einen anderen Reisenden in einem Zimmer auf der anderen Seite des Flurs angesteckt. Einer von zwei Reisenden nach Belgien kam infiziert aus Ägypten. Unter den fünf infizierten Reisenden, die in Israel ankamen, befand sich auch einer, der aus Malawi einreiste. Diese Reisenden reisten unter anderem über die Türkei, Dubai, Äthiopien und Jordanien ein.
Obwohl noch keine empirischen Daten vorliegen, besteht aufgrund der umfangreichen Mutationen von Omicron ein hohes Risiko, dass sich diese Variante der Impfstoffimmunität entzieht, was uns wieder an den Anfang der Pandemie bringen würde, allerdings mit einem sich viel schneller ausbreitenden Virus.
Was ist zu tun, um die Ausbreitung von Omicron zu verhindern?
Angesichts der Tatsache, dass die Omicron-Variante den Impfschutz zumindest teilweise umgehen kann, ist es wichtig, dass alle Länder die Maßnahmen im Bereich der öffentlichen Gesundheit und im sozialen Bereich ausweiten, um die Übertragung von COVID-19 zu begrenzen. Die Öffentlichkeit muss darauf hingewiesen werden, wie wichtig neben der Impfung Maßnahmen des öffentlichen Gesundheitswesens sind, um die eigene Gesundheit und die der Familienmitglieder zu schützen. Zu diesen, bekannten, Maßnahmen gehören das Tragen von Masken, Belüftung und Filterung und andere Vorsichtsmaßnahmen gegen die Übertragung über die Luft sowie Abstand halten zur Verringerung der Übertragung (kurz die AHA+L Regeln), Tests und Rückverfolgung von Kontakten zur Begrenzung der Größe von Clustern.
Es ist wichtig, dass alle Länder risikobasierte Grenzkontrollen einführen. Maßnahmen dazu umfassen:
— Einführung von Reisebeschränkungen für alle Länder mit bekannten oder vermuteten Fällen.
— Einführung einer allgemeinen Quarantäne und von mindestens zwei Tests (bei der Ein- und Ausreise) bei grenzüberschreitenden Reisen, z. B. durch eine mindestens 10-tägige Quarantäne in einer staatlichen Einrichtung, PCR-Tests vor der Reise und Tests bei der Ankunft und während der Quarantäne
— Ausweitung der Rückverfolgung von Kontakten zur Identifizierung aller Personen, die seit der Einreise mit dem Reisenden in Kontakt gekommen sein könnten, durch Einrichtung einer Omicron-spezifischen Überwachung
— Sensibilisierung und verstärkte freiwillige Offenlegung von Reisen in die betroffenen Länder, insbesondere in den letzten zwei Wochen, durch Einbeziehung der Medien,
Die Frühwarnung Südafrikas sollte gewürdigt werden, und das Land sollte bei der Bewältigung des Omicron-Ausbruchs unterstützt werden.
INFORMATIONEN, KONTAKTE, INTERVIEWS
USA: Yaneer Bar-Yam, Founder, World Health Network
USA: Eric Feigl-Ding, New England Complex Systems Institute
USA: Nassim Nicholas Taleb, New York University
France: Cécile Philippe, President, Institut économique Molinari
Germany: Matthias F. Schneider, WHN, Department of Physics, Technical University of Dortmund, Germany, matthias-f.schneider@tu-dortmund.de
+ 49 231 744 4139
Iberoamerica: Carlos Gershenson, Universidad Nacional Autónoma de México, info@worldhealthnetwork.global
India: Sunil Raina, Head of the Department of Community Medicine at the Dr. Rajendra Prasad Government Medical College in Himachal Pradesh, India
New Zealand: Michael Baker, Professor of Public Health and Epidemiology, University of Otago, Wellington New Zealand,
Israel: Meir Rubin, Executive Director, Kohelet Policy Forum
Canada: Stephane Bilodeau, WHN Indoor Air Quality Task Force
Taiwan : Shu-Ti Chiou, Founder & President, Health & Sustainable Development Foundation, Taiwan College of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan, Shu-Ti Chiou
Norway: Gunhild Alvik Nyborg, Covid Action Group, WHN
ÜBER DAS WORLD HEALTH NETWORK (WHN)
Das Weltgesundheitsnetzwerk (World Health Network, WHN) ist eine globale Gemeinschaft, die sich für den Schutz der Gesundheit und die Minimierung von Schäden für den Einzelnen und die Gesellschaft einsetzt. Es wurde als Reaktion auf die COVID-19-Pandemie als Arbeitsgruppe der Bevölkerung gegründet und umfasst unabhängige wissenschaftliche Beratungs- und Interessenvertretungsteams sowie Bürgerinitiativen. Das WHN lässt sich von Mitgefühl, wissenschaftlicher Strenge, Transparenz, sozialer Verantwortung und dem Wert des Lebens leiten. Das WHN setzt sich für wirksame Reaktion ein, die zu einer schrittweisen Elimination dieser Erkrankung führen und dies weltweit.
World Health Network
Die WHN-Deklaration wurde in The Lancet veröffentlicht.
whn Alerts
August 29, 2022: Monkeypox Self-Inoculation
Individuals infected with monkeypox can self-inoculate themselves (spread the infection to other areas of skin) by touching lesions and then other parts of their body, or through the repeated use of towels, bed sheets etc. This is especially risky for the eyes and may even cause permanent blindness. Touching lesions may also lead to a secondary infection that may cause scars and other damages.
Cover lesions at all times with disposable bandaids
Clean hands regularly
Use disposable gloves when touching lesions.
Never scratch a lesion (with hands or other objects/materials).
Change sheets and towels after each use.
Avoid touching your face.
NEVER touch your eyes with your hands, dirty towels, etc.
Avoid touching other sensitive areas, nose, mouth, genitals and rectum.
Do not wear contact lenses while you have active lesions.
If a child is infected, do your best to protect their eyes and prevent them from touching lesions.
Taking a bath carries some risk, adding vinegar to the bath has been mentioned as a potential mitigation, though evidence is not direct. Showers may have lower risk
June 25, 2022: Monkeypox and Children
The main risk groups for severe illness and death following monkeypox infection are children up to the age of 10, and pregnant or immuno-compromised people. The overall death rate in Africa of the spreading variant has been estimated to be 3.6%, with a significantly larger proportion of deaths occurring in children. Another significant fraction of children become permanently blind. In the developed world, percentages may be lower, but if kids become infected, many of them will suffer badly. Monkeypox virus remains infectious for an extended time on surfaces and is believed to infect through the skin as well as through airborne transmission. With an incubation period of 4-21 days, kindergartens and schools are likely to have super-spreader events that may be very hard to contain. In addition, about half the lesions in people infected in Africa turned into scars lasting for years. Such scars may stress kids, damage their mental well-being, and harm them socially. Isolation of up to 21 days may be hard for young children, and because a parent may readily get infected by simple touch as well as through shared air, many parents will get infected, which can extend the disruption for children for another few weeks. Kids may be infectious with very few symptoms, so it’s critical to ramp up testing capabilities in advance.
Initial symptoms include swollen lymph nodes, fever, headache, cough, muscle and back pain, fatigue, and chills. Within a few days, a rash of blisters develops, often beginning on the face, with some recent cases starting on the genitals or anus, then spreading to other parts of the body including the chest, palms of the hands and soles of the feet, and even inside the mouth. The rash, which can be extremely painful, and often causes scarring, goes through spots, pimples, blisters, abscesses, and scabs, before finally falling off.
action
Senior and Disability Action SF Public Health Commission
Title: Written statement for the San Francisco Health Commission on Broad Mask Requirements, Long COVID, and Monkeypox
Date: July 6, 2022
Authors: Yaneer Bar-Yam, Kaitlin E. Sundling, Geraldine A. Hamilton of the World Health Network
Summary:
We write to the Commission in strong support of the need for broad masking requirements, and strong public health messaging on the risk and harms of long COVID. Cases are going up in San Francisco with over 15% positivity rates, and BA.5, the growing variant, has higher transmissibility and severity than previous variants. Vaccine efficacy has further significantly decreased compared to recent variants. Therefore, the vaccine only approach can’t sufficiently protect the public. Long COVID is now known to be present in at least 1/3 of infected individuals and involves long term, serious impact on brain function, vascular function, immune system damage, and damage to multiple other organs including liver, lungs, and kidney. Also, the monkeypox outbreak should be taken seriously. Transmission through physical contact and with clothing, bedding and surfaces is considered dominant, but there is strong evidence it is airborne. We strongly recommend mask requirements. https://www.worldhealthnetwork.global/resources
Full Statement:
We hereby submit to the Commission the following points in strong support of the need for broad masking requirements, and strong public health messaging on the risk and harms of long COVID.
COVID cases are going up in San Francisco with over 15% positivity rates now, with BA.5 the growing variant that has higher severity than previous variants, significantly increased transmissibility, and more severe disease increasing likely hospitalization rates and deaths.
Vaccine efficacy has further decreased compared to recent variants due to changes in BA.5 that make it more immune evasive, therefore continuing with a vaccine only approach will be insufficient to protect the public
Variant is following variant with the next even more rapidly transmitting variant BA.2.75 expanding globally
Because rapid tests are often being taken without reporting to authorities, the undercounting of case rates makes it very difficult for policy makers to assess risk for everyone and for individuals to assess their own risk.
We are gaining more information about long covid. Symptoms are present in around 1 in 3 overall, and around 50% of those hospitalized (1,2,3), with 10-20% suffering more severe symptoms. Organ damage, irrespective of symptoms, is reported in studies as being over 50% (4). For example, impacts on cognitive function (IQ) happen even for those who have mild disease and do not report that they have long COVID symptoms. Children have about a 10-20% rate of long covid symptoms (5,6), depending on what is measured, and can experience the wide range of debilitating symptoms that are found in adults. Recent studies show that long covid is only reduced by 15% for those vaccinated and there is significant mortality in the post acute phase with 1.3% for those vaccinated and 2.0% for those unvaccinated (7). The expectation that immunity obtained from an infection reduces the severity of subsequent infections has been shown to be false (8). Reinfection adds substantial all-cause mortality, hospitalization, and adverse health outcomes in the acute and post-acute phase of the reinfection. Reducing overall burden of death, disease, disability and economic impacts due to SARS-CoV-2 will require strategies for reinfection prevention.
Masks are one of the five essential pillars of prevention of transmission for COVID-19. The others are air quality improvement through ventilation and HEPA air purification, surveillance testing for early case identification and isolation, and social distancing. There are multiple levels of adoption for each of these pillars and they can be combined to effectively reduce transmission in multiple ways (see Figure). We consider the prevention of transmission to be a technology adoption challenge which should be possible for San Francisco and its innovative technology driven ecosystem.
Mask requirements are needed to make it safer for high risk individuals (including immunocompromised people, people with disabilities, and seniors) and all people to access public spaces and essential services. Everyone is vulnerable to long covid effects including healthy young adults and children.
Universal masking lowers the risk of infection and it is significantly more effective than one way masking to protect individuals and specially more vulnerable populations. This is similar to an individual’s risk when drinking and driving, and being in the car with a driver who is drinking and driving. An example of two-way masking is pictured below. Even high-filtration N95 or KN95 masks do not always fit perfectly, and many have not had the opportunity to get fit-tested. Source control of potentially infectious people (who may be asymptomatic or presymptomatic) is important to reduce the risk of spreading the virus through the air.
Preventing transmission and reducing reinfections will also help prevent potential for Long COVID: now known to be in at least 1 in 3 people and involves long term, serious impact on brain function, vascular function, immune system damage, and damage to multiple other organs including liver, lungs, and kidney.
Given the Long COVID health impacts this could have debilitating effects on the public and the workforce. Preventing infections not only addresses the health aspects, future health costs, it also addresses the economic impact on the city and its workers.
Long COVID will bring severe strain to already struggling health care systems that are trying to cope with the increase in COVID infections.
Masks also help protect individuals and the public against other respiratory/airborne infections, air pollution, allergens, and smoke particles from wildfires.
The World Health Network has created guidelines to educate the public on key aspects of monkeypox including measures to prevent infection given the multiple possible routes of transmission that include the air. Infographics are also available for public distribution and education.
Transmission
Airborne transmission: transmission through aerosols is the dominant mode of spread for COVID-19
Airborne transmission is transmission through the inhalation of aerosols in the air. Aerosols can best be thought of as very fine mist or spray, and, in the context of COVID-19, these fine particles contain SARS-CoV-2 and are expelled in the air by coughing, sneezing, singing, speaking, and simply exhaling. Aerosols can also be created through mechanical means. Due to their miniscule size, aerosols can remain suspended in air for long periods of time–even hours after they have been released into the air (Van Doremalen et al., 2020). This creates ample opportunity to inhale virus-containing aerosols long after the source is no longer present (for example, long after an infected person breathing, speaking, or coughing in a room has left the room).
Historically, there have been barriers to observing and measuring aerosols directly, among which are their variable size and dynamics, obstacles associated with instruments of measurement, and limitations of sampling methods (Hogan et al., 2005; Cao et al., 2011; Pan et al.,2019). This makes detection and quantification of aerosols challenging, and incorrectly encourages the false conclusion that aerosolized virus is not a primary mechanism for SARS-CoV-2 transmission. Indeed, convergence of emerging evidence demonstrates otherwise.
Evidence for Airborne Transmission
Transmission over great distances
Cases of transmission between people who never come into contact is well documented (Eichler et al., 2021), including infection by inhaling contaminated air in adjacent rooms enabled by shared ventilation systems, as well as moving through and inhaling air a great distance away from the transmitting person (Lewis et al., 2021). Superspreader events, i.e. large gatherings which contribute to mass infection among people in sizeable indoor setting such as auditoriums and churches, as well as infection in closed-ventilation places such as cruise ships, strongly indicate that inhalation of moving air is the main mode of SARS-CoV-2 transmission (Greenhalgh et al., 2021; see also Nissen et al., 2020).
Indoor transmission is more common than outdoor transmission
It is well-established that infection with COVID-19 is more likely indoors than it is if one is in open air. Enclosed spaces determine that people inhale each other’s air (share a breathing space, see Lednicky et al., 2021) and that movement of air is limited (Bulfone et al., 2021). This strongly supports aerosol transmission as a primary mode of spreading the disease. The efficacy of appropriate ventilation and air purification in reducing infection rates indoors also demonstrates that breathing shared air with an infected person is conducive to becoming infected with SARS-CoV-2.
Asymptomatic and pre-symptomatic transmission
Transmission of the virus by people who are not experiencing symptoms or never develop symptoms but who have been infected also favors airborne transmission as a main mechanism of spreading COVID-19. Studies demonstrate that over half of COVID-19 infections occur through asymptomatic transmission and cannot be attributed to contact with a coughing, sneezing, or other droplet-producing behaviors (Johansson et al., 2021). The efficacy of high-quality masks and respirators in controlling the spread of COVID-19 even when symptoms are absent clearly shows that asymptomatic transmission of airborne virus is a key contributor.
Respiratory Droplets
Respiratory droplets are emitted during coughing, sneezing, and other activities, and are a vehicle for close-contact transmission. Due to their size and weight, droplets descend to the ground or other surfaces quickly after expulsion, and transfer infectious virus to a host by coming into contact with the upper respiratory tract upon inhalation, or via transfer of virus after touching contaminated surfaces (Gralton et al., 2010). While respiratory droplets play some part in proximal transmission of SARS-CoV-2 (Morawaska et al., 2020), this is unlikely to constitute a major source of disease spread and can be mitigated by masking when in the presence of crowds or nearby people. Importantly, the conventionally accepted size of respiratory droplets relative to the much smaller aerosols has been mistakenly regarded as affording greater viral loads to be expelled and therefore become highly infectious (Tang et al., 2021; for examples of the use of the term “droplet” to refer to particles within the size range of about 5μm vs 100μm, see Chen et al., 2020 and Morawaska et al., 2020). However, this argument ignores the relative paucity of data about the capacity of aerosols to contain significant quantities of virus. In the few examples when aerosol and droplet viral loads have been examined, aerosols have in fact proved to contain higher pathogen quantities than droplets (Fennely et al., 2020). Finally, droplets cannot function as the main vehicle of viral transfer since transmission, as mentioned previously, frequently occurs over distances far exceeding the area where droplets by an infected individual can land, lending further support to the consideration of airborne transmission as the main culprit in the spread of COVID-19.
school guidelines
\School guidelines must explicitly recognize that Covid-19 is an AIRBORNE virus and communicate proper precautions to the different stakeholders (including teachers, staff, parents and children). It is spread by inhaling AEROSOLS containing viral particles, which are exhaled by others. Keeping hands and high-touch surfaces clean is basic hygiene for all situations, but excessive use of disinfectants may be harmful, and do little to contain the spread of COVID-19 without airborne precautions in place as well.
Policy guidelines must also be adjusted as new variants occur. Preventing infection became significantly more difficult with the Delta variant due to high transmission (2-2.5X original variant and 1000X higher viral load) and further difficult with the Omicron variants (BA.1 and BA.2), the reduction in vaccine efficacy for transmission and severe disease, and the consequences of infection are worse due to higher severity, especially for children (including Multisystem Inflammatory Syndrome, MIS-C/PIMS-TS). The Omicron variant proved to be even more rapidly transmissible likely due to a change in the mechanism of infection that results in smaller viral loads that can infect, as well as bypassing much of the immunity due to vaccination and prior infection. Multiple infections are possible both of different variants and, especially for Omicron, by a single variant.
The role of children and youths in the spread of the coronavirus has been hotly debated since the first infections were registered. One thing is clear, children and youths can infect others. It is also clear that infected children and youths often show few or no signs of being ill. And it is just as clear that children and youths can also suffer lasting organ damage as the result of a COVID-19 infection. This doesn’t automatically mean that all children and youths are potential «superspreaders,» driving infection rates around them. Still, children and youths — through school, friends and sports — often have far more social interaction than adults. Like adults, young people often ignore social distancing and hygiene rules if they do not have clear guidelines in place to do otherwise. These guidelines are recommended to minimize risks in school settings.
Community transmission
The best way to ensure safety of children, teachers and families is to reduce transmission in the community.
Remote options
Remote options provide a means for families to make decisions about the risk they wish to take for their children, and themselves.
Families whose children are clinically vulnerable, or have family members who are clinically vulnerable should consider the risk and consequences of infection in deciding about remote options.
Where remote options are chosen, children may be organized to engage in outdoor activities with other children so as to provide social contact. Look for special games and other activities that allow for social distancing (due to Delta and Omicron, significantly larger distances are necessary).
Ventilation (general guidelines [1])
Outdoor spaces should be used for teaching and learning, and especially for activities where masks are not possible such as for lunch, and for sports and choir where high viral loads are generated. Use canopies where needed but avoid closed-sided tents as these are no different from being indoors. Where this is not possible, actions for indoor activities should be accompanied by significant effort to reduce the risk of transmission.
Mechanical ventilation (HVAC) systems should not allow recirculation without proper air filtration.
CO2 Monitors can serve as indicators of sufficient ventilation levels or indoor air quality risk: Use C02 meters, mounted on a wall approximately 5’ (1.5 m) up, not near a window, to measure the level of exhaled breath. Below 600 ppm is ideal; above 700-800 ppm the risk of transmitting Covid increases rapidly. With good air filtration (by central ventilation systems and HEPA air purifiers), the C02 target is less than 1000. Use C02 measurement to guide the following measures to improve indoor air quality.
Require the use of MERV 13 filters or equivalent (or higher efficiency filters) in all HVAC systems. If the system cannot function with MERV 13 filters, use the highest MERV filter grade that the system will tolerate and/or use a combination of filters and air cleaners (see next section) that achieve desired levels of air filtering.
Windows and doors should be open to allow fresh air in, both while the room is in use and afterwards for long enough for sufficient air exchange. Please note that, while opening windows may help reduce indoor risks by dilution of airborne particles, effectiveness varies greatly with wind speed and direction, temperature, building orientation, etc. While it reduces viral concentration in the air, opening windows alone may not be enough to keep C02 levels in the safe range because the intermittent amount of air exchanged with the outdoors. Avoid opening windows at desk level. Window fans should pull air out of the room. Ceiling fans should be on “winter” setting to draw air upwards.
Open windows should be considered as a temporary mitigation measure and shouldn’t be used as a robust or permanent solution to air filtering precautions for indoor space.
Students and staff should wear outdoor clothing in colder weather to allow windows to be kept open to the maximum extent possible.
Do not use rooms that lack external windows, suitable ventilation or air cleaning systems.
Filtration and air cleaners (High efficiency filters)
Use of HEPA filters is encouraged in all shared indoor spaces, it cleans the air reducing the density of virus carrying particles in the air, preventing infection of those who are not infected.[2]
When properly installed, ultraviolet germicidal light (UVGI) can be used as supplementary treatment to ventilation and air filters.
Devices that spray chemicals into the air and electronic air cleaners (ions, plasmas, hydroxyls, photocatalysis) can be harmful and should be avoided.
To maximize filtration while simplifying installation, choose a portable air cleaner that has a clean air delivery rate (CADR) that is large enough for the size of the room or area in which you will use it. The higher the CADR, the more particles the air cleaner can filter and the larger the area it can serve. Most air cleaner packaging will tell you the largest size area or room it should be used in. Portable air cleaners often achieve a high CADR by using a high-efficiency particulate air (HEPA) filter.
The reduction in virus carrying airborne particles improves with increased level of filtering. EPA HEPA filtering guidelines for environmental pollution are 5 ACH [3] (roughly one standard HEPA filter per classroom equivalent to 300-500 CADR). Unlike Covid infection, environmental pollution harm occurs by mass action, while even very small amounts of viral particles can cause infections [4], thus greater reductions should be the objective. Covid specific guidelines should be at least 10 to 12 ACH [5] (roughly 2 standard HEPA filters or 600 to 800 CADR per typical 25’ x 32’ classroom). The optimal air filtering system would ensure that exhaled air is filtered before another person breathes it in. Understanding the flow of air in the room is necessary to optimize filtering.
Reduction by 65% of airborne particles was obtained in a simulated environment in which 2 HEPA filters were located near an infected individual at 5 ACH total [6]. This shows the benefit of air filtering but also indicates higher levels of filtering should be used.
The placement of filters near the source is significantly better than other placements that resulted in 50-55% reduction of particles.
This optimized placement of filters cannot be achieved in a classroom since any child or the teacher might be infected. Without knowing which child is infected, the filters cannot be placed around that child or teacher. Movement around the classroom also results in exposure variation.
This points to the need for higher ACH levels than EPA guidelines.
Even higher ACH is necessary for Delta and Omicron variant due to higher viral load of exhaled air particles and ease of infection by small amounts of viral particles.
Properly designed DIY Air Cleaners have proven to be highly effective and less costly and can be considered as effective measures. The units should be placed near the center of the room, where the air will not flow directly over anyone, elevated to avoid tripping hazards, and run on the highest setting. High performance filters (MERV-13 or better) should be changed when needed to maintain performance and capacity.
Schools should use air filters not just in classrooms but also in other shared spaces including lunchrooms, hallways, bathrooms, locker rooms, gyms, lounges, and offices (see below), with a maximum sound level of 40-50 decibels, especially in classrooms.
Masks
Everyone should wear masks in indoor spaces. Outdoors masks should be worn where sufficient distance between individuals is not possible.
Indoors closer than 3 ft should be considered VERY CLOSE CONTACT.
The space of an entire connected air enclosure, during and several hours after occupancy by an infected individual, should be considered CLOSE CONTACT as airborne respiratory particles expand to fill the room and persist in the space until ventilation removes them.
Outdoors, the important measure is rate and the direction of air flow—being downwind of a person who is infected can lead to infection.
There is no single measure of adequate outdoor distance, 2 meters should be considered minimal but is not sufficient with Delta and Omicron due to the much larger viral load and small amount of viral particles that can infect.
The quality of a mask should be that of a N95 or similar (FFP2, KF94, KN95) Double masking with a surgical and a cloth mask is an alternative. Cloth masks alone are not sufficient with Delta and Omicron.
Masks should be evaluated for goodness of fit checking that airflow goes through the mask and doesn’t go around the mask when breathing in and out.
Children’s masks are not as readily available as adult masks but can be obtained, especially in FFP2, KF94, KN95 versions. Masks in special sizes for children are available.
Elastomeric half masks provide better fits and are reusable.
High quality masks should be provided to those who cannot afford them.
Where a student has difficulties e.g. anxiety or breathing difficulties, it would be safer for them to sit further away near an open window with air flowing outwards.
Lists of children’s masks:
Aaron J Prussin and Lindsey C Marr, Virginia Tech, https://tinyurl.com/etwcs4ae
Special spaces
Indoor lunches should be avoided as they lead to much higher opportunities for viral transmission including superspreader events. Where indoor lunches are necessary
Lunch should be distributed among different spaces including classrooms, gyms, auditoriums, as well as lunchrooms for minimal density of individuals in those spaces.
Groups in the same space should be consistent from day to day and constitute bubbles of class sizes or smaller than class sizes.
Those who eat lunch together should be considered to be close contacts.
Minimal time should be allocated for lunch.
Very high ventilation standards should be used where cafeterias must be used, with ideally no recirculation (100% fresh air intake) augmented by high efficiency filtration (see sections 3 and 4).
Bathrooms represent a high level of risk of transmission due to (a) short time high traffic use and persistent viral particles in the air leading to exposure from one individual to multiple others (from different bubbles), (b) flushing causing particles to become airborne that contain virus, (c) often poor standard ventilation.
Dramatically improve ventilation and air filtering for bathrooms and the ventilation system should be exhausting air (negative pressure of more than 50 Pa) to avoid any cross-contamination with adjacent spaces.
Avoid opening bathroom windows where those windows might lead to airborne particles entering other rooms through adjacent windows.
Ensure seat covers are present and post notices to close them before flushing.
Restrict the number of individuals in the bathroom at any time, e.g. one per every two stalls, where possible.
Deploy multiple HEPA filters in bathrooms. Since the walls of stalls restrict air flow, it is best to have one HEPA filter per stall, even if the filter chosen has reduced air flow capacity per unit.
Where possible position HEPA filters so that the outward airflow is toward the location of faces when seated or standing.
Hallways: Place HEPA filters at regular intervals along hallways according to the ACH needs.
Locker rooms and locker areas of hallways: Restrict distances between individuals to avoid interactions among different bubbles.
Teacher lounge: Repurpose teachers lounges so that teacher to teacher transmission does not link different bubbles.
Stairways: As much as possible, use the stair pressurization system approach using a supply fan to blow outside air into stairway or stairwell, creating a positive pressure differential across the enclosure boundary and avoiding any accumulation of contaminant or cross-contamination between adjacent spaces. The design of these ventilation systems can depend greatly on the local codes and standards, and if positive pressure is not possible, high level of ventilation (6+ ACH) or high efficiency filtration should be maintained.
Elevators: Elevators should not be used unless absolutely necessary (e.g. for wheelchair access), and where necessary solutions for air filtration in the elevator should be installed.
Sports: Sports should be conducted outdoors due to rapid breathing causing large amounts of respiratory particle generation.
Gyms: Should be repurposed to permit lower density activities in other spaces, including for lunch.
Choir: Choir should be conducted outdoors due to large amounts of respiratory particle generation.
Offices: Offices should follow ventilation and air purification guidelines. Remote work should be done as much as possible, virtual meetings should be standardized. In person meetings should take place outdoors, in larger spac
Schoolbuses: Masks must be worn on schoolbuses, the ventilation system should be set at 100% fresh air (no recirculation) and windows should be opened enough to let air in without compromising safety.es, and only as a last resort in offices.
General notes for all special spaces: When necessary to flush stale air from spaces between occupied periods, operate systems for a time required to achieve at least 6 air changes of equivalent clean air supply before and after occupation.
Bubbles / Cohorts and Lower Density Schools
In order to limit the number of close contacts and prevent wider outbreaks, bubbles should be formed that restrict within-room contact to as few individuals as possible.
Subdivide classes by using partially remote options.
Reduce density by expanding the space available to a class.
Identify and utilize opportunities to expand a school’s space to additional buildings to enable lower density classrooms and smaller bubbles.
The need for maintaining separation between bubbles should inform scheduling of bubbles for non-classroom activities, including entry to the school through the corridors, lunches, sports, and other activities.
When an individual who is a member of a bubble becomes infected, all members of their bubble should be quarantined.
Screening Testing
Screening testing provides for early detection and reduces transmission.
Using PCR tests reduces the number of cases by an estimated 70-85%. Rapid antigen tests reduce the number of cases by an estimated 50% (70% sensitivity relative to PCR).[1][2][3][4]
The rate of testing has been about 2 per week, but should be increased to every other day or even daily for the Delta variants, especially if rapid antigen tests are being used, but also where PCR or LAMP tests are being used, due to their false negative rates.
Test and Isolate
Individuals reporting a wide range of symptoms should be tested and isolated while they wait for results.
Isolation at home is a high risk and should be avoided if at all possible, separate quarters should be identified where individual or community resources enable out of home quarantine, as the likelihood of transmission to housemates is high.
Where isolation at home is necessary follow guidelines for isolation at home, including separate rooms, ventilation, hepa filtration, mask wearing, avoiding shared spaces, special precautions for bathrooms, cleaning and disinfecting.
Trace and Quarantine
Close contacts of an individual who is infected include anyone who has been in an indoor space at the same time, or within a few hours of an infected individual being present. This includes siblings and other family members and housemates. Duration of contact with an individual can be any time due to the high viral load of Delta variant [Previous guidelines of 15 min contact become less than 1 second for 1000X viral loads of Delta].
Close contacts should be quarantined. The same protocols for isolation should be followed for someone in quarantine with the exception that multiple individuals who are being quarantined must be separated from each other (note where an individual requires special care such as a child, elderly or for other reasons, special considerations must be made for care during quarantine while limiting exposure to the extent possible).
Testing of quarantined individuals is important for determining the need for contact tracing of their contacts. Testing negative does not remove the need for quarantine due to the incubation period lasting as long as 14 days or beyond.
Guidelines that have been suggested to allow reduction to 10 or 7 days when accompanied by negative tests [7] assumed 100% reliable PCR tests, but their false negative rates, estimated to be 15-30%, imply 14 day quarantines are necessary.
Vaccination
Vaccines reduce the likelihood of infection and of severe disease (by 2X and, for those infected by 2.5-3X, respectively). This protection is reduced for higher exposure due to changes in behavior or changes in policy. While vaccinated individuals are 2X less likely to be infected, they transmit at about the same rate due to similar viral load and therefore contribute to infections of others. Therefore, vaccinated individuals should follow the same rules as those of unvaccinated individuals. [Note, those who wear seatbelts or use airbags are not allowed higher speed limits or the right to drink and drive.]
Notes on Delta variant
The Delta variant changed the properties of the pandemic, here is a summary:
1000X viral load [8] and equivalent density of viral particles in the air means that a person produces a large amount of airborne particles as they breathe, speak, shout and sing.
Short time to symptoms reduced on average from 6 to 4 days, and short time to infectiousness reduced on average from 3 to 2 days.[8] Note that the incubation period continues to mean that the onset of infectiousness is not necessarily the typical or average onset but can be 14 days later.
The Delta variant also reduces vaccine efficacy against transmission and severe disease, with the transmission protection being about 2X, and the protection against severe disease being approximately 2-3X [9]. This means that for a particular exposure over a certain period of time the likelihood of severe disease is reduced by 4-6X. However, increased exposure or continued exposure increases the probability of infection so taking risks that leads to infection means that one gains only the reduction of severe disease which is 2-3X.
Combining the reduction in severity due to vaccination with the increase in severity due to Delta variant means that there is almost no change in severity for someone who is vaccinated compared to someone who was not vaccinated against the original variant.
For children, Delta is even more severe, with an increase of death rate estimated at 6-8X compared to previous variants.[4] Current estimates are 1 in 10,000 case deaths, 1 in 100 hospitalizations, and 1 in 10 long covid (with organ damage and loss of IQ expected to be higher as it occurs even for those who do not report long covid symptoms).
Notes on Omicron variant
The Omicron variant is much faster transmitting. The current understanding of the reasons for the rapid transmission include an underlying physiological change in the mechanism of transmission due to a different binding mechanism that makes infection possible higher in the lungs and therefore possible with smaller amounts of viral particles, and the ability of Omicron to bypass prior immunity due to either vaccination or previous infection.
Notes on current CDC guidelines
CDC guidelines continue to emphasize droplet transmission even though it has been demonstrated that COVID is primarily transmitted by airborne particles.
CDC guidelines continue to assume vaccination prevents transmission even though it only reduces it by a factor of about 2 for Delta, with rapid waning over several months.
CDC is making public health a personal issue, where individual risk is being emphasized rather than public health. It also emphasizes single event risk and not the accumulation of risk over time. This is a failed public health messaging strategy that leads to harm for everyone,
Example: Drinking while driving is not allowed due to public health implications.
Example: Risk for vaccination of being infected and transmitting leads to others becoming infected.
World health network
DECLARATION OF MONKEYPOX A GLOBAL PANDEMIC
JUNE 22, 2022
WORLD HEALTH NETWORK
The growth of Monkeypox in 58 countries through local community transmission around the world, with 3,417 confirmed Monkeypox cases reported across 58 countries, and the rate of growth of cases increasing week by week across multiple continents
The severe pain, scarring, blindness, and death, which has been observed in cases of Monkeypox historically.
The greater severity of Monkeypox in children, who have thus far been spared during the current outbreak but are likely to be infected increasingly as community transmission expands.
The danger of transmission to wildlife, including rodents such as mice, rats, squirrels, and domesticated pets, which would become a reservoir that will expand across the world leading to ongoing risk of human infection and the need to modify daily life due to this ongoing risk to avoid exposure in many contexts.
The World Health Network (WHN) declares the monkeypox outbreak a Public Health Emergency of Global Concern, by which it indicates that this outbreak is not limited to a single country or region and should be addressed by immediate actions taken wherever community transmission is taking place in order to ensure that the least effort is needed and the smallest impact is suffered due to this outbreak.
In particular the actions that are needed to achieve these objectives include:
Widespread public communication about the symptoms that identify monkeypox:
Initial symptoms include swollen lymph nodes, fever, headache, cough, muscle and back pain, fatigue, and chills. Within a few days, a rash of blisters develops, often beginning on the face, with some recent cases starting on the genitals or anus, then spreading to other parts of the body including the chest, palms of the hands and soles of the feet, and even inside the mouth. The rash, which can be extremely painful, and often causes scarring, goes through spots, pimples, blisters, abscesses, and scabs, before the scabs finally fall off.
Clear information about where testing for monkeypox is available, and the importance of testing in order to prevent the infection of family members and others.
Clear information about the need to isolate from others where symptoms may indicate infection even before the confirmation of monkeypox diagnosis.
Clear information about the possibility of infection outside of the gay community—in which most transmission occurred during the initial expansion of monkeypox across the world—to avoid promoting any misunderstanding or perceived stigma that would lead individuals not to report their symptoms or be tested.
Provision of accommodations in which isolation and quarantine is possible with necessary medical support.
Provision of financial and other support for individuals who should isolate or be quarantined.
Development of plans for targeted use of vaccination to contain the outbreak where necessary.
It is important to emphasize that early action requires the least intervention. Delayed action not only results in wider harm and suffering for those who become infected, but also much greater societal impact of interventions that are needed to contain its further effects. The current conditions are such that stopping the outbreak is likely possible with widespread case identification and contact tracing. Allowing further transmission may very well lead to conditions in which significantly more difficult and harsher interventions are needed to achieve the same objectives. Furthermore, monkeypox can affect anyone, so any perception and associated stigma that it only affects a specific group has the potential both to cause injustice and to hinder timely identification and isolation of all cases.
World health network
The World Health Network publishes a declaration urging immediate and effective action from country and global health authorities to prevent monkeypox from becoming a disaster.
CAMBRIDGE, Mass. – June 22, 2022 – The World Health Network (WHN) today announced that they are declaring the current monkeypox outbreak a pandemic given that there are now 3,417 confirmed Monkeypox cases reported across 58 countries and the outbreak is rapidly expanding across multiple continents. The outbreak will not stop without concerted global action. Even with death rates much lower than smallpox, unless actions are taken to stop the ongoing spread—actions that can be practically implemented—millions of people will die and many more will become blind and disabled.
The essential purpose of declaring a pandemic is to achieve a concerted effort across multiple countries or over the world to prevent widespread harm. The definition of a pandemic is an infectious disease growing over a wide area, crossing international boundaries, and usually affecting a large number of people. The accelerating growth across multiple continents, and the need for a concerted action to stop it, meets both the criteria, and the essential purpose, for declaration of a pandemic. Concerted global action is needed.
“There is no justification to wait for the monkeypox pandemic to grow further. The best time to act is now. By taking immediate action, we can control the outbreak with the least effort, and prevent consequences from becoming worse. The actions needed now only require clear public communication about symptoms, widely available testing, and contact tracing with very few quarantines. Any delay only makes the effort harder and the consequences more severe”, said Yaneer Bar-Yam, PhD, President of New England Complex System Institute and co-founder of WHN.
Until now most cases have been in adults, but any spread among children will lead to much more severe cases and more deaths. Infections of animals, especially rats and other rodents, but also pets, will make it much more difficult to stop. Passively waiting will lead to these harms without any compensating benefit.
The WHN announcement comes ahead of the The World Health Organization’s (WHO) meeting on June 23, 2022 to decide on their monkeypox outbreak designation. The WHN urges all local public health authorities to apply the precautionary principle and use the available, necessary, and proven interventions to contain and stop the spread.
“The WHO needs to urgently declare its own Public Health Emergency of International Concern (PHEIC)—the lessons of not declaring a PHEIC immediately in early January 2020 should be remembered as a history lesson of what acting late on an epidemic can mean for the world,” said Eric Feigl-Ding, PhD, Epidemiologist and Health Economist, and co-founder of WHN.
Monkeypox is a virus with the potential to cause significant harm to the public including acute painful illness that may require hospitalization, and may result in death, skin scarring, blindness, and other long-term disability. The most vulnerable to severe disease include children, pregnant people, and people who are immunocompromised.
“The first 18 months of the Covid pandemic showed us that stopping the virus is a cost effective strategy that aligns health and economic outcomes. Monkeypox is much easier to stop. This will provide a level of visibility, enabling businesses to project their societies and economies into the future”, said Cecile Phillips, Economist and President of, l’Institut économique Molinari.
Evidence supports many different routes of monkeypox transmission, including physical contact (touching an infected individual, especially the rash / postules), contact with contaminated clothing, bedding and objects, breathing airborne particles, and intimate contact/sex.
The WHN is urging immediate action by the WHO and national CDC organizations. Early action will have a greater impact with smaller interventions. If effective action is taken now, larger, more disruptive interventions will not be necessary. Health authorities and governments should learn from past mistakes in delaying response. Getting ahead of an outbreak is key to stopping it. Declaring it a pandemic now will help initiate a multi-stakeholder, multi-disciplinary approach to tackle it. The more we delay, the more we increase the chances of it getting out of hand.
Governments and public health authorities around the world, and particularly in countries with identified cases, should implement the following:
Implement case identification widely, with comprehensive contact tracing.
Provide free and readily available public testing services not limited by criteria of travel, contact with identified cases, or membership in current high risk groups.
Isolate and provide medical care to infected individuals, with implementation of precautionary infection and prevention control measures including for contact, droplet, and airborne transmission.
Provide up-to-date guidance for public health workers and clinicians.
Provide publicly available resources for isolation and case identification.
Raise awareness among the public of the need and opportunity for testing, and the possibility of being infected regardless of membership in currently higher risk groups.
Implement Public Health Service Announcements and education for symptom recognition.
Allocate funds to support above described interventions.
Plan for use of vaccines in locations and communities where ring vaccination of close contacts is advisable to prevent wider transmission.
Fast track emergency approval of updated monkeypox specific vaccines for children.
Provide funding and resources to community organizations and leaders for effective communication and services to reach underserved and under resourced communities.
The WHN declaration further describes the nature of this pandemic, the risk of inaction, and the recommended actions at http://worldheathnetwork.global/monkeypox
About the World Health Network
The World Health Network is a collaboration of scientific and citizen teams empowering action to promote health and prevent harm. It is independent from any political body or government, and guided by compassion and scientific rigor. For more information, visit worldhealthnetwork.global.
Media Contact:
Katie Marsh
New England Complex Systems Institute
programs@necsi.edu
Additional Quotes by WHN members and Global Experts:
USA Members Quotes:
Tiffany James, community activist, Columbia, South Carolina, Covid Action Group and World Health Network
«We have the opportunity to get ahead of another potential public health catastrophe. We need to act now in order to inform and prepare our most vulnerable communities worldwide to ensure they do not have the same fate as we have seen with the COVID-19 pandemic. Eliminating stigma and biases pertaining to monkeypox must be a priority in order to get public buy-in to participate in safe practices to eliminate the virus. Compounded pandemics will only further harm our already fragile communities”
Kaitlin Sundling, M.D. PhD physician-scientist, Madison, Wisconsin, Covid Action Group and World Health Network
“Monkeypox has the potential to cause significant harm and suffering if the outbreak is allowed to grow. Swift action from our leadership is needed. Complacency or hesitation may carry a high price. Proven methods will stop the spread of this deadly and damaging virus”
“Monkeypox can affect anyone. Stigmatization has the potential to hinder timely identification and isolation of all cases”
European Members Quotes:
Matthias Schneider, Technische Universität Dortmund, Germany, Covid Action Group and World Health Network
«We (humans) do not have a good intuition for probability. So don’t get fooled by «unlikely» / «likely» scenarios. We must act with precaution and no mercy for the virus. This is the natural and logical response to an uncertain threat. This would have stopped Covid-19 then, and can prevent the spread of Monkeybox now.»
Meir Rubin, Executive Director, Kohelet Policy Forum, Israel
«Monkeypox easily infects all mammals, between them and back to humans. To assume that the virus will limit itself to a certain population will lead us to global endemism that will require huge efforts to control.»
Latin American Members Quotes
Carlos Gershenson, Universidad Nacional Autónoma de México, Mexico, Covid Action Group and World Health Network
“COVID-19 has shown us that we should better be overcautious in the face of uncertainty. We cannot simply hope for the best when dealing with global risks. We should not make the same mistake with monkeypox. Hoping is not enough. We will achieve the best only when we expect the worst.»
World health network
Vaccination against covid-19 of children between 5 and 11 years of age began in Denmark at the end of November.
The association Covid-19 school and children and the action group Lärarupproret (Teachers Voice): Sweden should follow Denmark and Finland.
French Economist Cécile Philippe interviews Norway Researcher, M.D., Phd, BSc Econ. Gunhild Alvik Nyborg about the challenges Norway faces with Omicron.
French Economist Cécile Philippe interviews Meir Rubin about the challenges Israel faces with Omicron. Meir Rubin serves as Executive Director of the Kohelet Policy Forum, a non-profit organization that strives “to secure Israel’s future as the nation-state of the Jewish people, to strengthen representative democracy, and to broaden individual liberty and free-market principles in Israel.” Meir graduated from the Hebrew University in Law and Economics.
Make it stand out. «, «spaceBelowSectionTitle»: < "value": 40, "unit": "px" >, «sectionTitleAlignment»: «left», «isSectionButtonEnabled»: false, «sectionButton»: < "buttonText": "Make It", "buttonLink": "#", "buttonNewWindow": false >, «sectionButtonSize»: «large», «sectionButtonAlignment»: «left», «spaceAboveSectionButton»: < "value": 40, "unit": "px" >>» data-media-alignment=»left» data-title-alignment=»left» data-body-alignment=»left» data-button-alignment=»left» data-title-placement=»left» data-body-placement=»left» data-button-placement=»left» data-layout-width=»full» data-title-font-unit=»rem» data-description-font-unit=»rem» data-button-font-unit=»rem» data-space-between-rows=»20px» data-space-between-columns=»20px» data-vertical-padding-top-value=»3.3″ data-vertical-padding-bottom-value=»3.3″ data-vertical-padding-top-unit=»vmax» data-vertical-padding-bottom-unit=»vmax» >
An OPED in Sweden’s National Paper «Dagens Nyheter»
Vaccination against covid-19 of children between 5 and 11 years of age began in Denmark at the end of November.
The association Covid-19 school and children and the action group Lärarupproret (Teachers Voice): Sweden should follow Denmark and Finland.
Now that there are approved covid vaccines for children from the age of 5, Sweden should follow our Nordic neighbors and offer vaccines to the youngest school children as well. At the same time, the Swedish Public Health Agency should recommend testing of all children with symptoms, no matter what their age is.
French Economist Cécile Philippe interviews Norway Researcher, M.D., Phd, BSc Econ. Gunhild Alvik Nyborg about the challenges Norway faces with Omicron.
Original article published December 23, 2021 in L’Express magazine and on the Institut Économique Molinari online journal.
French Economist Cécile Philippe interviews Meir Rubin about the challenges Israel faces with Omicron. Meir Rubin serves as Executive Director of the Kohelet Policy Forum, a non-profit organization that strives “to secure Israel’s future as the nation-state of the Jewish people, to strengthen representative democracy, and to broaden individual liberty and free-market principles in Israel.” Meir graduated from the Hebrew University in Law and Economics.
Original article published December 23, 2021 in L’Express magazine and on the Institut Économique Molinari online journal.
The Global Health Network enables easier, faster, and better research in the world’s most challenging settings.
Better Research for Better Health
Research is critical to gaining the data we need to solve the world’s biggest health challenges.
The Global Health Network drives faster progress by sharing methods and processes to raise standards, remove duplication and enable faster transfer of evidence into practice.
The Global Health Network enables sharing of research methods, knowledge, and experience, online and on the ground.
Delivering training, skills, and career development to frontline healthcare workers and research staff to encourage locally-led research and to implement research findings into policy and practice.
The Global Health Network raises standards and improves the quality of research by sharing cross-cutting processes, tools, and guidance. Resulting in easier, faster, better research addressing the world’s biggest health challenges.
World Health Network
1 World Health Network
2 дистанционное техническое обслуживание
дистанционное техническое обслуживание
Техническое обслуживание объекта, проводимое под управлением персонала без его непосредственного присутствия.
[ОСТ 45.152-99 ]
Параллельные тексты EN-RU из ABB Review. Перевод компании Интент
MyRobot: 24-hour remote access
Тематики
Обобщающие термины
См. также в других словарях:
World Health Organization — WHO redirects here. For other uses, see Who (disambiguation). World Health Organization منظمة الصحة العالمية 世界卫生组织 Organisation mondiale de la Santé Всемирная организация здравоохранения Organización Mundial de la Salud … Wikipedia
Canadian Health Network — The Canadian Health Network (CHN) is a national, bilingual health promotion service operated by the Public Health Agency of Canada and major health organizations across Canada. It is an on line collaborative service and includes health… … Wikipedia
University Health Network — The University Health Network (UHN) is an umbrella organization encompassing three major hospitals in Toronto, Canada and a group of medical laboratories and foundations. It is closely affiliated with the University of Toronto in conducting… … Wikipedia
Men’s Health Network — Logo Men s Health Network (MHN) is a non profit educational organization of physicians, researchers, public health workers, other health professionals and individuals. MHN is committed to improving the health and wellness of men, boys, and their… … Wikipedia
Health insurance — is insurance against the risk of incurring medical expenses among individuals. By estimating the overall risk of health care expenses among a targeted group, an insurer can develop a routine finance structure, such as a monthly premium or payroll … Wikipedia
Health promoting hospitals — (HPH) is a network of the World Health Organization Regional Office for Europe. It is based on the health promotion philosophy of the World Health Organization (WHO) as outlined in the WHO Ottawa Charter for Health Promotion (WHO 1986) which was… … Wikipedia
Health informatics in China — (Chinese: 医学信息学) is about the Health informatics or Medical informatics or Healthcare information system/technology in China. The main review and assessment of health informatics in China[1] for the WHO Health Metrics Network was conducted in… … Wikipedia
Health Protection Agency — Agency overview Formed 2003 Preceding agency Health Protection Agency (special health authority) and National Radiological Protection Board Superseding agency none Jurisdiction United Kingdom Headquarters … Wikipedia
Health promotion — Health promotion, as defined by the World Health Organization, is the process of enabling people to increase control over, and to improve, their health. [ [http://www.euro.who.int/AboutWHO/Policy/20010827 2 WHO/Europe Ottawa Charter for Health… … Wikipedia
World Lymphoma Awareness Day — (WLAD) is held on September 15 every year and is a day dedicated to raising awareness of lymphoma, an increasingly common form of cancer. It is a global initiative hosted by the Lymphoma Coalition (LC), a non profit network organisation of 36… … Wikipedia
World Health Network
1 network
to break a network smuggling hi-tech equipment into a country — ликвидировать сеть контрабандистов, ввозивших в какую-л. страну высокотехническое оборудование
to set up network — устанавливать / создавать / организовывать систему
2 WHN
3 marketing
marketing director — маркетинговый директор, директор по маркетингу
marketing expert — маркетинговый эксперт, эксперт в области маркетинга
marketing expertise — маркетинговая экспертиза, экспертная оценка в области маркетинга
Do we need to improve marketing or simply drop a particular product? — Нужно ли нам улучшить маркетинг или лучше отказаться от какого-л. продукта?
Internet marketing is not as difficult as it sounds. — Маркетинг в интернет не так сложен, как может показаться.
I could prove that any male could do the weekly marketing at our local Ding Dong faster than any Mom. — Могу сказать с уверенностью, что любой мужчина может закупать провизию в нашем местном «Динг-Донге» быстрее домохозяйки.
4 WHIN
5 whin
6 WS
7 ws
8 remote maintenance
дистанционное техническое обслуживание
Техническое обслуживание объекта, проводимое под управлением персонала без его непосредственного присутствия.
[ОСТ 45.152-99 ]
Параллельные тексты EN-RU из ABB Review. Перевод компании Интент
MyRobot: 24-hour remote access
Тематики
Обобщающие термины
9 remote sevice
дистанционное техническое обслуживание
Техническое обслуживание объекта, проводимое под управлением персонала без его непосредственного присутствия.
[ОСТ 45.152-99 ]
Параллельные тексты EN-RU из ABB Review. Перевод компании Интент
MyRobot: 24-hour remote access
Тематики
Обобщающие термины
10 WNH
См. также в других словарях:
World Health Organization — WHO redirects here. For other uses, see Who (disambiguation). World Health Organization منظمة الصحة العالمية 世界卫生组织 Organisation mondiale de la Santé Всемирная организация здравоохранения Organización Mundial de la Salud … Wikipedia
Canadian Health Network — The Canadian Health Network (CHN) is a national, bilingual health promotion service operated by the Public Health Agency of Canada and major health organizations across Canada. It is an on line collaborative service and includes health… … Wikipedia
University Health Network — The University Health Network (UHN) is an umbrella organization encompassing three major hospitals in Toronto, Canada and a group of medical laboratories and foundations. It is closely affiliated with the University of Toronto in conducting… … Wikipedia
Men’s Health Network — Logo Men s Health Network (MHN) is a non profit educational organization of physicians, researchers, public health workers, other health professionals and individuals. MHN is committed to improving the health and wellness of men, boys, and their… … Wikipedia
Health insurance — is insurance against the risk of incurring medical expenses among individuals. By estimating the overall risk of health care expenses among a targeted group, an insurer can develop a routine finance structure, such as a monthly premium or payroll … Wikipedia
Health promoting hospitals — (HPH) is a network of the World Health Organization Regional Office for Europe. It is based on the health promotion philosophy of the World Health Organization (WHO) as outlined in the WHO Ottawa Charter for Health Promotion (WHO 1986) which was… … Wikipedia
Health informatics in China — (Chinese: 医学信息学) is about the Health informatics or Medical informatics or Healthcare information system/technology in China. The main review and assessment of health informatics in China[1] for the WHO Health Metrics Network was conducted in… … Wikipedia
Health Protection Agency — Agency overview Formed 2003 Preceding agency Health Protection Agency (special health authority) and National Radiological Protection Board Superseding agency none Jurisdiction United Kingdom Headquarters … Wikipedia
Health promotion — Health promotion, as defined by the World Health Organization, is the process of enabling people to increase control over, and to improve, their health. [ [http://www.euro.who.int/AboutWHO/Policy/20010827 2 WHO/Europe Ottawa Charter for Health… … Wikipedia
World Lymphoma Awareness Day — (WLAD) is held on September 15 every year and is a day dedicated to raising awareness of lymphoma, an increasingly common form of cancer. It is a global initiative hosted by the Lymphoma Coalition (LC), a non profit network organisation of 36… … Wikipedia
World health network
Airborne Precautions (DIY and more)
4-5pm EST Nov 3
The panel will discuss and showcase Airborne precautions for schools and workplaces, notably various DIY solutions, and the onset of an international coalition to generalize what was done in some states in US with already specific countries’ projects. During the panel, we will livestream the production of a box in real-time as a livestream during the second session.
Stephane Bilodeau
Sam Causton
Amanda Hu
Live Demonstration of DIY Cleaner making
Stephane Bilodeau
Airborne Risk Mitigation for All + Chair of the session
Big Pharma and «Vaccine Apartheid»
11am-12pm ET Nov 4
Anthony Staines, Professor of Health Systems, Dublin City University, and Tim Bierley with Global Justice Now, will outline how big pharma and rich countries have created a devastating “vaccine apartheid.» High income countries like the UK have ordered more than 3 times the amount of doses they’ve needed, whilst only 1.9% of people in low and middle income countries have received a single dose.
Fred Leplat
Anthony Staines, Professor of Health Systems, Dublin City University
Tim Bierley, Global Justice Now
Collaboration Not Siloed Session
9-10am ET Nov 4
The panel will discuss will introduce the Canadian interdisciplinary coalition approach. The Airborne Transmission Coalition, ZeroCovid or PPE Advocates, Occupational health and safety, Parents groups, Unions and Civil society groups collaborating to generate more traction. Notably, last year they successfully pushed for messaging to the Canadian Government for the message that covid is airborne. This panel will address how interdisciplinary groups work better than acting in our own silos. Different groups, backgrounds, specialities, but agree on the main goals/message. Interdisciplinary outreach.
Stephane Bilodeau
Alec Farquar
Alec Farquar
Canadian Coalition on Airborne Transmission/Occupational Health & Safety
Dr Joe Vipond
CAPE, Mask4Canada, POP Alberta
Sam Causton
Coalition from Civil Society for DIY solutions
Stephane Bilodeau
Airborne Risk Mitigation for All + Chair of the session
Gosia Gasperowicz (with PoP Alberta Group and ZeroCovidCanada)
Measures to Suppress & Eliminate
COVID Responses in South American Countries
9-10am ET Nov 4
South America, the most unequal region globally, has been hit hard by the Covid-19 pandemic, with a high number of cases and deaths and severe consequences on social and economic conditions. The responses, however, have been different in different countries. This session aims to discuss Covid responses in three key countries that have developed different approaches to preventive and healthcare measures and social protection interventions, trying to identify lessons to be learned, especially concerning equity.
Luis Eugenio de Souza
Mauricio Barreto
Rosana Campos
Avriel Diaz
COVID Responses in Ecuador
Cristian Rebolledo
COVID Responses in Chile
Ligia Kerr
Essential Data
4pm EST / 1pm PT Nov 3
This session will examine challenges and opportunities for expanding public access to COVID-19 case data. Increasingly, community members, parents and workers consult data dashboards, joining health experts in seeking to understand areas of high risk and transmission. Looking at information collected through contact tracing, and by tracking school cases, closures, and workplace outbreaks, speakers will reflect on key considerations for sharing meaningful data in the public interest.
Laura Streitfeld, Policy and Communications Strategist, Founder and Executive Director, Preserve Rural Orange
Shefali Oza, Ph.D., Epidemiologist, Senior Advisor, Partners in Health
Liz Rosenberg, Co-Founder and Steering Committee Member, Parents for Responsive Equitable Safe Schools (PRESS NYC)
Kaliris Salas-Ramirez, Ph.D., Neuroscientist, Distinguished Medical Lecturer, CUNY School of Medicine
Local Volunteering in China
8-9pm EST Nov 3
Xu Wenwen is a Wuhan-based English teacher who founded the Zebra Volunteer Group during the height of the outbreak in Wuhan. Group efforts were aimed at providing medical supplies to the hospitals, and daily necessities to local residences.
Zebra Volunteer Group
Initiated by Wuhan local volunteers during the start of the Covid pandemic. The aim is to provide PPE for medical staff and community workers. For more than 20 days, this group received generous PPE donations from overseas, individuals and organizations, and connected them to Chinese official philanthropy groups and rescue teams. In the later stage, they also received monetary and food donations, and transported them to the under-privileged communities in Wuhan.
Harm Reduction
8-9pm EST Nov 3
This session will discuss how harm reduction tools, including vaccines, tests, masks, and ventilation are being implemented globally in different ways. We will discuss how not accepting the science is preventing the optimal implementation of harm reduction tools that reduce the spread of COVID-19.
Theo Allen
Sara Citrenbaum
Julia Raifman
David Eldridge
Nicholas Smit
Gosia Gasperowicz
10-11am EST Nov 4
This session will discuss how families can avoid COVID-19 infections and keep resilience levels high to survive the COVID-19 Pandemic healthy in body and soul.
Berta Schodlok
Simone Draber
Roshan Mamarvar
Why to protect the children and family even after vaccination
Berta Schodlok
Simone Draber
7-8am ET Nov 4
At the Second Global Summit to End Pandemics, we want to share snapshots, experiences and open questions of what we have learned together. We want to summarize and look back as a local collective. Therefore we ask: What did we reach? How does it feel? Was it worth it? What did we learn? Now, we at least reached a safer and healthier together, so everybody could relax and feel welcome. Our well-being depends on our own actions. And strong actions can only work together!
Cornelius Fischer
Hanna Koch
Dr. Cornelius Fischer
Empowerment and strong actions. Everyone can reach safe spaces if WE just DO it!
Hanna Koch B.A.
The only good system is a healthy social systems. Towards ONE common vision to keep our spaces safe!
Josef S. Dipl. Ing.
Self-PCR collectives to create minimal risk spaces.
Dr. Elisa S.
Development of concepts to strengthen active communities that care.
Florian F.
Social interaction and cultural participation is key. How we supported it.
4-5:00pm EST Nov 3
This joint session will examine how to spark a grassroots movement, run completely by volunteers, using the internet. Our presentation addresses how to leverage community support to train the general public to become powerful advocates, by identifying issues that arise when employing social media. Our goal is to empower those unfamiliar with social media to use it to get their message out and reach the maximum number of people.
Julie Lam
Lindsay Schwarz
Arin Parsa
Ayaan Moledina
Julie Lam and Lindsay Schwarz
How to use social media to raise awareness and start a grassroots movement. What is grassroots empowerment? What are the obstacles? Why we need to build a community and bring people together on social media.
Arin Parsa and Ayaan Moledina
How to train teens to promote preventive measures and support public health? How to reach teens and get them to support awareness?
Listening to Children on «Back to School» in the Current Pandemic
9-10am EST Nov 4
The World Health Network (WHN) was set up in 2020 to bring people from very diverse disciplines, expertise and backgrounds, to work together for a ZERO COVID environment. In the current pandemic it is a very difficult period for children to cope with going ‘back to school’ under a new school environment and misinformation on COVID-19. Therefore, WHN is reaching out to learn from the perspective of children from diverse backgrounds in this virtual WHN Global Summit.
Meena Nathan Cherian
TBD
LongCovid: How pathogen persistence must be evaluated and addressed
5pm EST Nov 3
This session will cover the pandemic of chronic illness caused by COVID, the NIH’s decades-long failure to fund research about the enormous role of stealth, persistent infections in those with autoimmune, chronic and psychiatric illness, and explain the science behind it.
Dana Parish
Steven Phillips, MD
Possible mechanisms for LongCovid, how to prevent and manage it
Amy Proal, PhD
How Covid evades immune system and persists, causing ongoing symptoms
Natalie Lambert, PhD
Identifying LongCovid symptoms and barriers to care
Западная часть Тихого океана (Азия)
Америка (Южная и центральная)
Западная часть Тихого океана (Океания)
All regions
| 51.2% |
| 32.06% |
| 2.4% |
| 2.21% |
| 3.45% |
| 3.63% |
| 1.07% |
| 3.95% |
All regions
Schizophrenia and Related Disorders
Substance-Related Disorders and Behav Addictions
Dementia, Delirium, and Related Disorders
Attention Deficit and Conduct Disorders
Autism Spectrum Disorders
Obsessive-Compulsive and Related Disorders
Forensic Psychiatry / Psychology
Emerging Experience with New Categories in the ICD-11: Compulsive Sexual Behaviour Disorder
Научные выводы
Зарегистрироваться
Присоединяйтесь к нам!
Если Вы практикующий специалист в области охраны психического здоровья или первичного звена здравоохранения, Вы можете зарегистрироваться в нашей сети.
The New Era of Web 3.0 Medical Data Economy
Welcome to DeHealth — AI & Medical Data Based decentralized app to securely and anonymously store, manage and monetize depersonalized medical data.
DeHealth connects individuals, medical institutions, and data consumers in a secure and mutually beneficial system enabling a win-win data exchange of high-quality, structured data sets.
Learn how DeHealth works
Check this video to understand how the DeHealth system works and the features of the application, and the opportunities it opens for global healthcare development.
DeHealth in numbers
Individuals entrusted their health records
Hospitals partnered up with DeHealth
Members in our community
Token holders over the world
DeHealth redefines the healthcare landscape by making medical data the driving force of change. Individuals get a unified and secured source of truth for medical data, monetization opportunities, and access to their medical records 24/7 across the globe.
Healthcare providers are rewarded for sharing data and contributing to medical advances. Data consumers receive verified data for better treatment, prevention, and research.
Individuals store their medical data securely and anonymously, access it worldwide, manage data distribution and monetize it with the help of the DHLT token. All of this contributes to a new normal for a healthy lifestyle.
We always welcome opinion leaders to join our community of raving fans who want to spread the word about the DeHealth solution and its impact.
This is an infrastructure where healthcare providers share the medical data of clients upon their prior consent, while both getting DHLT tokens and opportunities from the DeHealth network.
The platform provides structured, high-quality, and relevant medical data to pharma companies and other data consumers for further research, drug manufacturing, and disease prevention.
The problems we solve
The company uses the power of Medtech, Blockchain, Big Data, AI, and ML to address the challenges of the industry.
The lack of thought-through infrastructure for data storage & management
Long data verification process & high entry threshold
Lack of proper Big data analysis impeding better disease treatment & prevention
Cybersecurity vulnerability in the industry & growing health data security risks
Medical data comes raw, unverified & unstructured, adding to further misuse of such
Barriers to a healthy lifestyle due to patients` little or zero access to medical data
Find out how we engage you into the whole DeHealth system, data exchange with healthcare providers, and monetization mechanisms.
World health network
This is a global project focused on communicating information about how to make schools safe based on the latest science, in easy to understand language and in multiple formats. This includes a series of animations with voice overs and a set of illustrated documents and posters. These are currently in English, but will be translated into other languages. The animations and documents will be shared / sent out via social media and national / local press and be available as a resource for schools.
«>
Schools Community Action Project
Communities across Europe and the US are engaged in this project focused on empowering parents and teachers to help make schools safer. We work with parents and teachers advocating and engaging in improving school safety and remote options. The effort involves writing and share petitions, write to school and government officials, organize local communities, and engaging with the press.
US: We won’t sacrifice our children. Together, we keep us safe:
«>
The group is looking at applying practical solutions, notably, ventilation, filtration, CO2 monitoring or DIY Air-Cleaners. We’re working on simple and low-cost solutions for higher risk settings (confined, closed spaces, poorly ventilated) that would benefit from such quick, yet safe fixes to Improve Indoor Air Quality and to further minimize risks on top of the other Covid precautions. The task force also investigates procurement, decision making and multiple Do-It-Yourself designs.
This WHN IAQ group is a work-in-progress, an ongoing effort to help parents, teachers, schools or workplaces to materialize DIY airborne precautions to better protect children, staff, families and communities.
«>
«>
About Us
The Global Indoor Health Network is a 501(c)(3) organization dedicated to providing education and awareness of the health effects of mold and other indoor contaminants.
Our worldwide network of scientists, physicians, researchers, indoor air quality experts, attorneys, teachers, injured workers, advocates and others are working together to promote healthy indoor environments in homes, schools and businesses.
We have united to share our collective knowledge, expertise and life experiences to advance the understanding and awareness of this very important public health issue.
Naysayers and Deniers (Explains why the truth is being hidden about toxic mold)
Vision
Our vision is a global community of individuals and organizations working together to ensure that comprehensive information and guidance concerning medical treatment, investigative techniques and solutions are available to address the effects of contaminants in the indoor environment of homes, schools and businesses.
Welcome to the Global Health Training Centre
Free eLearning courses in global health research for staff of all roles, in all regions and covering all disease areas, developed by The Global Health Network in collaboration with respected partners such as the World Health Organization
Online workshops and seminars in global health research, s panning research disciplines, regions, and therapeutic areas, aiming to foster collaboration, facilitate discussion, and celebrate advances and achievements towards faster and better research for health
Build your professional profile, create your CV and track your career in global health research as it develops. This flexible framework covers all the competencies that should be demonstrated by a research team to carry out a successful study
Begin your journey into health research here!
ESSENTIAL RESEARCH SKILLS TRAINING CURRICULUM
The Essential Research Skills Training Curriculum study identifies the minimum set of skills, knowledge and key principles that would enable those with limited or no previous experience to undertake high-quality research for health.
More than 536,000 people have taken over 2.5 million eLearning modules
in global health research and received certificates
NEW COURSE
POPULAR
MORE TRAINING RESOURCES
MORE TRAINING RESOURCES
NEW COURSE
MORE TRAINING RESOURCES
Sign up for the Global Health Training Newsletter here
Keeping you up to date on all the training and careers resources from around The Global Health Network
Social
World Health Network declares Monkeypox a pandemic
The World Health Network (WHN) announcement comes ahead of WHO meeting to be held on 23 June to decide on their monkeypox outbreak designation, APA reports citing Livemint.
Even with death rates much lower than smallpox, unless actions are taken to stop the ongoing spread—actions that can be practically implemented—millions of people will die and many more will become blind and disabled, it said.
With 3,417 confirmed Monkeypox cases reported across 58 countries, World Health Network (WHN) has announced that they are declaring the current monkeypox outbreak a pandemic.
The outbreak is rapidly expanding across multiple continents and will not stop without concerted global action, it said in a statement.
The WHN announcement comes ahead of WHO meeting to be held on 23 June to decide on their monkeypox outbreak designation.
The outbreak will not stop without concerted global action, it said.
World health network
You have covid, now what?
Contracting COVID can be disturbing as well as confusing. Here are the most essential steps to take when you test positive for COVID (or have been exposed to someone who has) with links to more detailed guidelines.
Don’t panic. Most people recover from Covid-19 and are able to return to their activities. Following these recommendations will give you the best chance to get there and to help prevent others you care about getting sick as well.
Begin isolation as quickly as possible and limit social contact to contain transmission. [1]
If possible, isolate away from other people. If you have to isolate at home with family or housemates, isolate yourself from them in separate rooms designated as the Red zone, rooms connected to the Red zone are the Yellow zone, which you should avoid as much as possible, and other rooms are the Green Zone for housemates. If possible, use a separate bathroom. [2]
Avoid sharing air using open windows, ventilation and HEPA air purifiers, keeping doors closed, blocking air flow under doors, and everyone should wear high quality masks when going into the Yellow zone (also if anyone uninfected has to go into the Red zone or you have to go into the Green zone).
While you are in a room by yourself (in the Red Zone), don’t wear a mask—it is best to breathe fresh air, open windows and use a HEPA filter.
Consume plenty of fluids, a healthy balanced diet, and rest.
To protect others it is important to contact (via email, text, phone call, or other means of remote contact) everyone you have encountered in the past week (even two weeks) and inform them that you have tested positive so that they too can get tested, inform their contacts, and isolate.
Check for mutual aid groups in your community and hotlines that can help you with necessities or specific help. Write down contact information for COVID hotlines. Check with your healthcare provider or state or local government website for information about medical assistance call centers, on-call medical personnel, and patient resources. Have these numbers handy if you experience a change in symptoms or need to consult with a healthcare provider.
Monitor your symptoms. Those include temperature, heart rate, oxygen (if you can, order an oximeter online), energy levels, GI symptoms, and other signs of malaise. Record any changes in symptoms. Follow best practices for optimizing respiratory health ([3]).
Seek medical attention if symptoms worsen (fever consistently >101F or 38C, difficulty breathing, chest pain, swelling or bruising of extremities, new or worsening cough, blue lips, extreme fatigue, worsening confusion).
Order groceries via delivery or contactless pick up ([4]).
It is best to remain in isolation for 14 days, longer if you continue to have symptoms or continue to test positive. There is some scientific precedent for a minimum 10 or 12 day isolation. However, shorter isolation periods make it harder for you to take care of yourself sufficiently and put everyone around you at a much greater risk of getting infected. It may seem to some that this is hard to do, but just like any condition, making yourself and others sicker is not a good solution. If your workplace doesn’t allow a 14-day isolation period, try negotiating remote work for the duration of testing positive and experiencing symptoms. Explain that this will reduce the likelihood others would have to take time away from work due to contracting the illness.
After you have recovered, remember that there’s still an increased risk for adverse outcomes like heart attacks and strokes, and that reinfections are possible. Recognize Long covid symptoms and seek care.
Before exiting isolation, take an at-home PCR or antigen test, avoid contact with others if you are still testing positive for the virus. A positive antigen test indicates you are likely to be still infectious, a PCR test may also find residual viral particles that are not infectious, but it is best to be careful and avoid contact with others until you test negative two days in a row.
Infodemic
An infodemic is too much information including false or misleading information in digital and physical environments during a disease outbreak. It causes confusion and risk-taking behaviours that can harm health. It also leads to mistrust in health authorities and undermines the public health response. An infodemic can intensify or lengthen outbreaks when people are unsure about what they need to do to protect their health and the health of people around them. With growing digitization – an expansion of social media and internet use – information can spread more rapidly. This can help to more quickly fill information voids but can also amplify harmful messages.
Infodemic management is the systematic use of risk- and evidence-based analysis and approaches to manage the infodemic and reduce its impact on health behaviours during health emergencies.
Infodemic management aims to enable good health practices through 4 types of activities:
Subscribe to the Infodemic Management News Flash to receive latest biweekly updates from the team.
Member States have recognized the importance and need of an infodemic response through recent resolutions, coming together in solidarity and responding to calls for actions. Therefore, WHO is building partnerships across all societies to respond to the COVID-19 infodemic and is developing country tools for infodemic management that can be used now and for future infodemics.
During the COVID-19 pandemic, WHO has worked with the UN family, tech sector, media, civil society and other amplifying communities to understand concerns, co-develop messages, extend the reach of health information, and to respond to the information needs of communities. WHO has also worked with academia to develop a public health research agenda for infodemic management, and with a diverse group of experts to develop a competency framework and trainings in infodemic management.
WHO is championing universal access to credible health information, and building resilience to misinformation for people worldwide. At the same time, more efforts are needed to better understand the scale of the infodemic, and impact of strategies used to manage it, in order to develop new toolkits for countries.
Through regional networks, such as the Africa Infodemic Response Alliance, WHO is fostering new approaches to meet changing needs for an evolving health emergency infodemic response. This is providing a foundation for further collaborations to also improve preparedness and early detection of emerging and resurgent health threats.
WHO is working with partners across society to strengthen the scientific discipline of infodemiology. The purpose is to build and deliver sustainable tools that health authorities and communities can use to prevent and overcome the harmful impacts caused by infodemics.
Through partnerships, WHO works to bolster digital capabilities and leverage social inoculation principles to foster higher digital and health literacy, build resilience to misinformation, and deliver innovative ways to reach communities with reliable health information. Here are a few of those innovations:
To advance progress on infodemiology, WHO regularly convenes the global community for conferences to discuss and chart ways forward on infodemic management topics.
World Health Network
Смотреть что такое «World Health Network» в других словарях:
World Health Organization — WHO redirects here. For other uses, see Who (disambiguation). World Health Organization منظمة الصحة العالمية 世界卫生组织 Organisation mondiale de la Santé Всемирная организация здравоохранения Organización Mundial de la Salud … Wikipedia
Canadian Health Network — The Canadian Health Network (CHN) is a national, bilingual health promotion service operated by the Public Health Agency of Canada and major health organizations across Canada. It is an on line collaborative service and includes health… … Wikipedia
University Health Network — The University Health Network (UHN) is an umbrella organization encompassing three major hospitals in Toronto, Canada and a group of medical laboratories and foundations. It is closely affiliated with the University of Toronto in conducting… … Wikipedia
Men’s Health Network — Logo Men s Health Network (MHN) is a non profit educational organization of physicians, researchers, public health workers, other health professionals and individuals. MHN is committed to improving the health and wellness of men, boys, and their… … Wikipedia
Health insurance — is insurance against the risk of incurring medical expenses among individuals. By estimating the overall risk of health care expenses among a targeted group, an insurer can develop a routine finance structure, such as a monthly premium or payroll … Wikipedia
Health promoting hospitals — (HPH) is a network of the World Health Organization Regional Office for Europe. It is based on the health promotion philosophy of the World Health Organization (WHO) as outlined in the WHO Ottawa Charter for Health Promotion (WHO 1986) which was… … Wikipedia
Health informatics in China — (Chinese: 医学信息学) is about the Health informatics or Medical informatics or Healthcare information system/technology in China. The main review and assessment of health informatics in China[1] for the WHO Health Metrics Network was conducted in… … Wikipedia
Health Protection Agency — Agency overview Formed 2003 Preceding agency Health Protection Agency (special health authority) and National Radiological Protection Board Superseding agency none Jurisdiction United Kingdom Headquarters … Wikipedia
Health promotion — Health promotion, as defined by the World Health Organization, is the process of enabling people to increase control over, and to improve, their health. [ [http://www.euro.who.int/AboutWHO/Policy/20010827 2 WHO/Europe Ottawa Charter for Health… … Wikipedia
World Lymphoma Awareness Day — (WLAD) is held on September 15 every year and is a day dedicated to raising awareness of lymphoma, an increasingly common form of cancer. It is a global initiative hosted by the Lymphoma Coalition (LC), a non profit network organisation of 36… … Wikipedia
World health network
French Economist Cécile Philippe interviews Norway Researcher, M.D.,Phd, BSc Econ. Gunhild Alvik Nyborg about Omicron.
December 23, 2021
CP: Norway has recently been in the news because of a Christmas party in Oslo. What can you tell us about it?
GN: This outbreak was made possible through the current Norwegian strategy. Indeed, until Omicron appeared, and since early summer, Norway was experimenting with a new strategy summarised by the overly well-known sentence “live with the virus”. You need to know that Norway was succeeding in keeping control over the virus in the first part of the pandemic. Anyway, what happened in Oslo on November 26th was the first Omicron super-spreader event known in Europe. As of December 8th, it has been confirmed that 80 people attending the Christmas party are Sars-Cov 2-positive. Among them, 17 are confirmed as being infected with the Omicron variant, and it is assumed that a majority of cases for which the sequencing results still unavailable will be found to be infected with the same variant. Sixty more people who visited the restaurant have been infected as well.
CP: What does it tell us about this new variant?
GN: It tells us many things. First, it shows the dynamics of variants that I have been warning against since the beginning of these pandemics. You want to keep the number of contaminations very low because, otherwise, new variants of concern are engineered. Second, it shows that new variants are not necessarily less harmful for society. First with Delta and now with Omicron, we discover that describing a virus as “mild” does not mean it ends up being less lethal: since it is more contagious, we get many more cases. And this aspect is what makes Omicron really worrying, because Norway may lose control of this new virus. It happens that some people attending the party went to a ski resort. It is believed that 21 Norwegian regions then got the virus from this ski resort. According to a recent report, the Norwegian Institute of Public Health estimates 90,000 to 300,000 new daily cases and 50 to 300 new hospitalizations per day over a three-week period, in a population of five million. This is along the lines of my own calculations, published on my Facebook page. If strong measures are not taken to stop the contaminations, it will not take more than four weeks for the entire population to be potentially contaminated, according to these models. The replication rate of this virus is between two and three days. We need to act quickly.
CP: Is the government taking new measures to deal with this new risk?
GN: it is, but not quickly enough. I can sense a change of attitude within the political arena since they have seen the epidemiological forecast, but there has been little decisive action up to now. Mask mandates have been imposed again when you cannot be at least one metre from other people, and booster shots are heavily recommended as is working from home. Restrictions have been imposed on the numbers of people allowed to gather and, as of yesterday, alcohol may not be served in restaurants. This will still not be enough at the present stage.
CP: How do you explain the slowness to react?
GN: There are many issues at stake. There is fatigue, of course as in many countries. There is also the very strong belief that vaccination would end the pandemic, that it would make it possible for the virus, if not to go extinct, at least to become harmless. This could have been true if vaccines had been able to stop transmission and if it had been possible to vaccinate the entire population quickly. Kids over 12 have been late to get vaccinated in Norway, and kids under 12 are not vaccinated at all. Vaccines are great tools and a crucial part of the strategy to fight this pandemic, but we have made the mistake of believing they could suffice. Vaccines are very effective when combined with non-pharmaceutical measures with the clear goal of avoiding contamination. And a final point I want to insist upon: the belief that natural immunity for kids can be a good thing is our loss. First, kids can get long Covid, but again you do not want to waste your vaccine investment on new variants.
CP: The fact remains that, from the outset, Norway has managed the crisis better than other countries. Deaths per million inhabitants remain low, and the economy did not take as big a hit as in France. How do you explain this?
GN: You are right. There is something positive we can say about Norway. Even though it is difficult to think out of the box, as consensus is sacred, the fact is the population is pragmatic. When facing facts and reality, people understand and comply. And this is happening. While at the start of the crisis, Norway was going to handle the crisis in the same was as other European countries, it decided on March 12th, 2020, that it was not possible to live with the virus, and it went into a strict lockdown for the time necessary to get rid of the virus, with border controls and quarantines maintained for a long time. Only when almost the entire eligible population had been vaccinated was it believed that these measures were not necessary anymore. We are about to learn again that they may be needed for longer periods of time along with the capacities to test, trace and isolate.
CP: Consensus is almost a matter of life and death in the Nordic countries. However, you have become a celebrity of sorts after telling people a story different from what the authorities wanted to tell at first. What happened?
GN: You could say that I have become a kind of whistle-blower, with the expected outcome that people listen closely to what I say, but many experts try to make me invisible. It happens that, at the beginning of the crisis, I was doing research at Oslo University Hospital. As resources were redirected towards the pandemic, I took the time to read everything I could about Covid-19. I would send notes and briefs to health experts, public authorities, to anyone I thought could benefit from this expertise. Then, witnessing complacency among decision-makers and health experts, I accepted an invitation to debate the situation with Fredrik Solvang, a prominent journalist known for the quality of his show on NRK (Norwegian Broadcasting Corporation, the country’s largest media organisation). This broke the news, as it was seen by 15% of the population. People believed me, and this helped empower decision-makers who shared my view that we needed to act quickly and that we should not let the virus get out of hand. Since then, I have been working incessantly to try to spread knowledge and new scientific results to the general population and to decision-makers. Recently, I have been at it again with an op-ed published by NRK. I was told it was read by around 5% of the population. The text explains that living with the virus means investing in all the measures that will put us ahead of it, not letting it roam free. I hope these contributions can add to the efforts of all those working to make a difference again.
CP: What are the lessons we should learn from Norway?
GN: Against my own personal preferences, I believe we won’t be able to avoid a new lockdown. A lesson we all need to bring home is, the sooner the better if we want to spare lives, the economy and our freedoms. Another lesson is that you need to choose your strategy carefully. People outside Norway do not realise that, for many months, Norwegians have been freer than people in most European countries because we had picked the right strategy. Norway was strong on border controls and quarantines, making life easier for the locals. You need to make sure to invest in measures that will keep you ahead of any future wave. Practically speaking, you need to see any outbreak as a fire. As soon as it is declared, put all your energy into extinguishing it. Fighting Covid is expensive. Better to prevent it than to try repairing the damage once it has completely overcome your society.
Since the publication of the interview, there has been a change of attitude in Norway and it managed to get cases down over the holidays.
on Dec. 15., the government issued new measures.
No lockdown was enacted, as very little has been actually closed but lots of advices on keeping distance, wearing masks etc. Some schools closed early for Christmas and some parents took their children out of school early to avoid illness during Christmas.
Most important is that the whole country seemed to take the issue seriously again and the results have been impressive. Over Christmas, Norway has actually seen cases drop, although from a high level of delta transmission to a yet high but still lower lever of mixed omicron+delta. At the moment, omicron is the dominant variant in the Oslo area but not in the country as a whole. We have managed to give almost 30% of the population a third dose now which is good.
However, 12-15 year olds have only been given a single dose, and 5-11 have unfortunately not yet been offered any vaccines as the NIPH have not yet decided to offer these the protection of the vaccines, aside those children with serious underlying conditions. So it is expected that cases will rise now when school starts tomorrow, no masking. I hope these vaccines will be allowed very shortly as they of course have been approved by EMA and the Norwegian equivalent, Norw. Medicines Agency, and are now proven safe and efficacious, and there are reports of increasing number of child admissions to hospitals due to Covid.
But the Norway example of Dec. 2021 serves to illustrate that measures do work: See the attached figure for comparison of how number of cases in Norway and Denmark have diverged after both countries saw early, large omicron super spreader events.
World health network
This is a global project focused on communicating information about how to make schools safe based on the latest science, in easy to understand language and in multiple formats. This includes a series of animations with voice overs and a set of illustrated documents and posters. These are currently in English, but will be translated into other languages. The animations and documents will be shared / sent out via social media and national / local press and be available as a resource for schools.
«>
Schools Community Action Project
Communities across Europe and the US are engaged in this project focused on empowering parents and teachers to help make schools safer. We work with parents and teachers advocating and engaging in improving school safety and remote options. The effort involves writing and share petitions, write to school and government officials, organize local communities, and engaging with the press.
US: We won’t sacrifice our children. Together, we keep us safe:
«>
The group is looking at applying practical solutions, notably, ventilation, filtration, CO2 monitoring or DIY Air-Cleaners. We’re working on simple and low-cost solutions for higher risk settings (confined, closed spaces, poorly ventilated) that would benefit from such quick, yet safe fixes to Improve Indoor Air Quality and to further minimize risks on top of the other Covid precautions. The task force also investigates procurement, decision making and multiple Do-It-Yourself designs.
This WHN IAQ group is a work-in-progress, an ongoing effort to help parents, teachers, schools or workplaces to materialize DIY airborne precautions to better protect children, staff, families and communities.
«>
«>
World health network
We have watched with increasing concern as cases have surged in England while mitigations have been progressively removed. Only 52% of the UK population is fully vaccinated. Ministers have been advised that this plan will likely result in 1-2 million cases over the coming weeks and potentially 7-10 million before the end of the year, and a peak of over 100,000 cases daily over the summer. The government’s own scientific advisors warned on the 7th July that high numbers of infections would lead to an increase in hospitalisations and deaths, more people suffering from ‘Long-COVID’”, and “the increased risk of new variants emerging”. They cautioned that “the combination of high prevalence and high levels of vaccination creates the conditions in which an immune escape variant is most likely to emerge. The likelihood of this happening is unknown, but such a variant would present a significant risk both in the UK and internationally.”
The UK government has both a national and global responsibility, even more so in its current role as chair of the G7. The current strategy of mass infection risks undermining efforts to control the pandemic not just within the UK but in other countries as well.
The UK government must urgently reconsider its proposed actions.
Co-signatories:
Prof. Gagandeep Kang, Christian Medical College, Vellore, India
Prof. Walter Ricciardi, Università Cattolica del Sacro Cuore, Italy
Prof. Martin McKee, London School of Hygiene & Tropical Medicine
Dr Stephen Duckett, Grattan Institute, Melbourne, Australia
Adv. Meir Rubin, Kohelet Policy Forum, Israel
Prof. Yaneer Bar-Yam, New England Complex Systems Institute, Cambridge, MA, USA
Prof Michael Baker, University of Otago, Wellington, New Zealand
Prof Shu-Ti Chiou, Health & Sustainable Development Foundation, Taiwan
Prof Jose M Martin-Moreno, ASPHER Honours’ Committee & University of Valencia, Spain
Dr. Deepti Gurdasani, Queen Mary University of London, UK
Dr. Hisham Ziauddeen, University of Cambridge, UK
Prof Christina Pagel, University College London, UK
Dr. William A. Haseltine, ACCESS Health International
Radiation: 5G mobile networks and health
5G, or fifth generation, is the latest wireless mobile phone technology, first widely deployed in 2019. 5G is expected to increase performance and a wide range of new applications, including strengthening e-Health (telemedicine, remote surveillance, telesurgery).
5G, or fifth Generation, is the latest wireless mobile phone technology, first widely deployed in 2019.
5G is expected to increase performance and a wide range of new applications, including strengthening e-Health (telemedicine, remote surveillance, telesurgery).
5G represents an evolution in telecommunication standards. To enable increased performance, 5G will extend into higher frequencies around 3.5 GHz and up to a few tens of GHz. The higher frequencies are new to mobile phone networks, but are commonly used in other applications, such as point-to-point radio links and body-scanners for security checks.
At these higher frequencies, 5G networks will use a greater number of base stations and of connected objects. 5G will further employ beam-forming antennas to focus signals more efficiently towards the device in use, rather than having the signal spread in broad directions as in current base station antennas.
Currently, exposure from 5G infrastructures at around 3.5 GHz is similar to that from existing mobile phone base stations. With the use of multiple beams from 5G antennas, exposure could be more variable as a function of location of the users and their usage. Given that the 5G technology is currently at an early stage of deployment, the extent of any change in exposure to radiofrequency fields is still under investigation.
To date, and after much research performed, no adverse health effect has been causally linked with exposure to wireless technologies. Health-related conclusions are drawn from studies performed across the entire radio spectrum but, so far, only a few studies have been carried out at the frequencies to be used by 5G.
Tissue heating is the main mechanism of interaction between radiofrequency fields and the human body. Radiofrequency exposure levels from current technologies result in negligible temperature rise in the human body.
As the frequency increases, there is less penetration into the body tissues and absorption of the energy becomes more confined to the surface of the body (skin and eye). Provided that the overall exposure remains below international guidelines, no consequences for public health are anticipated.
Two international bodies produce exposure guidelines on electromagnetic fields. Many countries currently adhere to the guidelines recommended by:
These guidelines are not technology-specific. They cover radiofrequencies up to 300 GHz, including the frequencies under discussion for 5G.
WHO is conducting a health risk assessment from exposure to radiofrequencies, covering the entire radiofrequency range, including 5G, to be published by 2022.
WHO will review scientific evidence related to potential health risks from 5G exposure as the new technology is deployed, and as more public health-related data become available.
WHO established the International Electromagnetic Fields (EMF) Project in 1996. The project investigates the health impact of exposure to electric and magnetic fields in the frequency range 0-300 GHz and advises national authorities on EMF radiation protection.
WHO advocates for further research into the possible long-term health impacts of all aspects of mobile-telecommunications. The Organization identifies and promotes related research priorities. It also develops public information materials and promotes dialogue among scientists, governments, and the public to increase understanding around health and mobile communications.
Global Health
Health is fundamental for a good quality of life. Being free from illness or injury directly affects our capacity to enjoy life.
In this entry we provide an overview of the available empirical evidence on aggregate health outcomes, focusing on long-run cross-country data from mortality and morbidity tables; and then provide an analysis of available evidence on health determinants, focusing specifically on the returns to macro healthcare investments.
Life expectancy is the most commonly used measure used to describe a population’s health. Historical data shows that global life expectancy has increased drastically over the last couple of centuries, with substantial long-run improvements in all countries around the world. In fact, recent life expectancy gains in developing countries have been particularly important. However, despite recent progress towards long-run cross-country convergence, there are still huge differences that have to be addressed: in several countries in Sub-Saharan Africa the average life expectancy is still less than 60 years, compared to more than 80 years in countries in Europe or in Japan.
Historical reductions in child mortality and maternal mortality have been crucial to improving life expectancy around the world. But also for these two measures of health we observe large remaining inequalities: low-income countries still have, on average, child mortality rates that are more than ten times higher than those in high-income countries. We show that similarly large gaps remain for other measures of health, including recent burden-of-disease estimates.
A growing body of empirical research suggests that, at a macro level, health outcomes are highly responsive to healthcare investments. Moreover, as one would expect, the evidence suggests large health returns to healthcare expenditure at low levels of baseline expenditure. This implies that international resources channeled through development assistance for health, if suitably targeted and managed, have the potential of drastically reducing global inequalities in living standards.
This is a ‘meta-entry’. All visualizations and data discussed here are also discussed in more detail in other, more specific data entries on the topic of health. In what follows we provide links to these other entries, as we cover the corresponding topics. These include Life Expectancy, Child Mortality, Healthcare Provision, Health Inequality, among other.
Health Outcomes
Life expectancy
Further in-depth information on life expectancy, including definitions, data sources, historical trends and much more, can be found in our dedicated entry on Life Expectancy.
How has cross-country life expectancy changed in the long-run?
The visualization summarises available life expectancy data over the last few centuries. The estimates from the UK – the country for which we have the longest time-series – show that life expectancy before 1800 was very low, but since then it has increased drastically. We can see that in less than 200 years the UK doubled life expectancy at birth. And the data shows that similarly remarkable improvements also took place in other European countries during the same period.
The chart also shows large historical changes in life expectancy estimates for other countries. Notice, for example, that a century ago life expectancy in India and South Korea was as low as 23 years – and a century later, life expectancy in India almost tripled, and in South Korea almost quadrupled.
You can switch to the map view in this visualization by clicking on the corresponding tab, in order to compare life expectancy across countries. The map shows that, despite long-run cross-country convergence, there are still huge differences between countries: people in some sub-Saharan African countries have a life expectancy of less than 50 years, compared to 80 years in countries such as Japan.
The increase in life expectancy happened to a significant extent because of changing mortality patterns at a young age, but this was not the only reason: life expectancy increased for people at all ages.
Click to open interactive version
Have all countries in the world experienced increasing life expectancy?
The visualization here shows the cumulative share of the world population (horizontal axis) against the corresponding life expectancy (vertical axis) at different points in time (colored lines). You can think of this as a bar-chart of life expectancy by country, but where countries have been ordered by life expectancy, and the width of each bar has been drawn proportional to each country’s share of the world population.
For 1800 (red line) we see that the countries on the left – including India and also South Korea – have a life expectancy of around 25 years. And on the very right we see that in 1800 no country had a life expectancy above 40 (Belgium had the highest life expectancy with just 40 years).
In 1950 life expectancy in all countries was higher than in 1800, but we can see that inequality grew substantially. This happened because very large improvements in health outcomes took place in some countries (mainly the richer countries in Europe and North America), while others (notably India and China) made only little progress.
In 2012 (green line), we can see again an improvement in life expectancy across all countries; yet interestingly, improvements in this last period implied a reduction in inequality. This happened through very large recent improvements in life expectancy across developing countries.
The conclusion is that the world developed from equally poor health in 1800, to great inequality in 1950, and back to more equality today – but equality at a much higher level.
Life expectancy of the world population, 1800, 1950 and 2012 1
In the long run the inequality in life expectancy within countries decreased hugely
The inequality in years of life between people within the same country can be measured in the same way that we measure, for example, the inequality in the distribution of incomes. The idea is to estimate the extent to which a small share of a country’s population concentrates a large ‘stock of health’, hence living much longer than most of the population in the same country.
As can be seen in the chart, inequality in health outcomes has fallen strongly within many countries.
Click to open interactive version
Child mortality
In the preceding section we studied life expectancy at birth as a key measure of aggregate health in a population. This measure provides an overview of health outcomes for the average person in a country. In this section we focus on health outcomes specifically for children.
An analysis of mortality for children provides important information regarding aggregate health in a country, because the first years of life are characterised by important health-related challenges. Consequently, life expectancy increases substantially conditional on surviving the first years of life. Indeed, as we shall show, an important part of the gains in life expectancy at birth are precisely due to large reductions in child mortality.
Child mortality is usually measured as the probability per 1,000 live births that a newborn baby will die before reaching age five under current age-specific mortality patterns.
Further in-depth information on child mortality, including definitions, data sources, historical trends and much more, can be found in our dedicated entry on Child Mortality.
How has cross-country child mortality changed in the long-run?
The interactive time-series plot shows how child mortality has changed over the long run. As we can see, child mortality in industrialised countries today is below 5 per 1,000 live births – but these low mortality rates are a very recent development. In pre-modern countries child mortality rates were between 300 and 500 per 1,000 live births. In developing countries the health of children is quickly improving – but child mortality is still much higher than in developed countries.
A second interesting feature of the trends depicted in this chart is that there are many sharp ‘spikes’ in the 19th century. This is partly because the data quality is improving over time, but also because health crises were more frequent in pre-modern times. The decline of crises is an important aspect of improving ‘living standards’. In our entry on food price volatility you find empirical evidence of how frequent food crises were. In the following plot you can see what these and other crises – epidemics or wars, for example – meant for the health of the population.
You can switch to the map view in this visualization by clicking on the corresponding tab, in order to compare child mortality estimates across countries and time. The map reinforces what we already noted: all countries have reduced child mortality in the long run, but there are still large differences between developed and developing countries.
Click to open interactive version
Are developing countries catching up with low child mortality rates in developed countries?
The fact that developing countries have made particularly fast improvements to reduce child mortality in the last fifty years, has meant that cross-country gaps have been closing.
The following visualization shows child mortality estimates by income level of countries. We can see a clear downward trend across all groups. And since high-income countries have seen the slowest progress (due to their already high health outcomes) we can see that the gap between these countries and the rest of the world has been narrowing. Upper middle income countries are in fact close to catching up.
Nevertheless, the latest figures show the important challenges that remain: low-income countries have, on average, child mortality rates that are still more than ten times higher than in high-income countries. The remaining gap is still large.
Click to open interactive version
The five most lethal infectious diseases over time
The chart focuses on the five most lethal infectious diseases. It shows the number of child deaths caused by these diseases from 1990 onwards.
Deaths caused by malaria and HIV/AIDS were rising over the 1990s. From 2005 onwards the deaths caused by each of these diseases is declining.
The most important disease referred to as ‘lower respiratory infections‘ in the visualization is pneumonia.
Click to open interactive version
Maternal mortality
Similarly to child mortality, maternal mortality provides important information regarding the level of health in a country.
Maternal mortality is usually defined as the number of women dying from pregnancy-related causes while pregnant, or within 42 days of pregnancy termination (typically expressed as a ratio per 100,000 live births).
Further in-depth information on maternal mortality, including definitions, data sources, historical trends and much more, can be found in our dedicated entry on Maternal Mortality.
Maternal mortality reduced in the long run
The visualizations above highlight the drastic long-term improvements that countries have made to reduce child mortality. But have these health improvements also materialized for mothers?
The chart shows long-run maternal mortality estimates for a selection of mainly high income countries. We can see that a hundred years ago, out of 100,000 child birth, between 500 and 1,000 ended with the death of the mother. This means every 100th to 200th birth led to the mother’s death. Since women gave birth much more often than today, the death of the mother was a common tragedy. Today, these countries have maternal mortality rates close to 10 per 100,000 live births.
The decline of maternal mortality to around 10 per 100,000 births can be attributed to our modern scientific understanding of the causes leading to maternal mortality. In fact, a common reason for mothers to die was puerperal fever (or childbed fever), which was caused by unhygienic conditions leading to infections in the mothers’ genital tract during childbirth. It was the physician Ignaz Semmelweis who first noticed the link between hygiene and the survival of mothers in the middle of the 19th century, but it was only until the germ theory of disease became known that appropriate practices became widely adopted.
The same chart also shows that different countries have achieved progress in maternal mortality at different points in time. The decline of maternal mortality in Finland, for example, began in the middle of the 19th century and didn’t reach today’s low level until more than a century later. Malaysia in contrast achieved this progress in only a few decades.
Click to open interactive version
How do countries around the world currently compare in terms of maternal mortality?
Recent data on maternal mortality shows improvements around the world. The following interactive visualization presents a world map of maternal mortality rates for the period 1990-2013. You can switch to the chart view to explore country-specific trends.
As before, the conclusion here is that despite recent widespread improvements in the developing world, there are huge challenges ahead: in sub-Saharan Africa more than 500 mothers die per 100,000 live births. This is more than 60 times higher than the figure for countries in the European Union.
Click to open interactive version
Burden of disease
Context
In the preceding sections we discussed health outcomes, as measured only from data on mortality. This does not take the morbidity from disease and disability into account.
The burden of disease is a related, but different measure of health outcomes that accounts for both the mortality and the morbidity of disease.
The most common way to measure the burden of disease is to estimate the number of ‘lost’ years due to poor health – the so-called loss in Disability Adjusted Life Years, or DALYs.
This variable is calculated as the sum of years of potential life lost due to premature mortality, and the years of healthy life lost due to disease and disability. As such, the measure of a country’s DALYs extends the notion of life expectancy, in the sense that it incorporates both the prevalence of different diseases or risk factors, and the relative harm they cause. One DALY lost can be thought of as one lost year of ‘healthy’ life. You can read more about the definition and calculation of DALYs in the technical report WHO methods and data sources for global burden of disease estimates.
Further in-depth information on burden of disease can be found in our dedicated entry on Burden of Disease.
The global distribution of the disease burden
This map shows DALYs per 100,000 people of the population. It is thereby measuring the distribution of the burden of both mortality and morbidity around the world.
We see that rates across the regions with the best health are below 20,000 DALYs per 100,000 individuals. In 2017 this is achieved in many European countries, but also in Canada, Israel, South Korea, Taiwan, Japan, Kuwait, the Maldives, and Australia.
In the worst-off regions, particularly in Sub-Saharan Africa, the rate is higher than 80,000 DALYs per 100,000.
Click to open interactive version
Infectious diseases
The data from the Global Burden of Disease Project, discussed above, shows that there are still important challenges regarding certain diseases, notably HIV/AIDS and malaria. Here we discuss trends showing how the fight against these diseases is evolving.
The most common way of measuring the evolution of diseases is to estimate the number (and frequency) of deaths caused by the diseases; as well as the number of new people suffering from them.
Further in-depth information can be found in our entries dedicated to HIV/AIDS and Malaria.
Is the world making progress in its fight against HIV/AIDS?
The 1990s saw a substantial increase in the number of people infected with HIV and dying of AIDS.
Between 1996 and 2001 more than 3 million people were infected with HIV every year. Since then the number of new infections began to decline and in 2019 it was reduced to below 2 million. The lowest number of new infections since 1990.
The number of AIDS-related deaths increased throughout the 1990s and reached a peak in 2004, 2005 when in both years close to 2 million people died. Since then the annual number of deaths from AIDS declined as well and was since halved. 2016 was the first year since the peak in which fewer than 1 million people died from AIDS.
The chart also shows the continuing increase in the number of people living with HIV. The rate of increase has slowed down compared to the 1990s, but the absolute number is at the highest ever with more than 36 million people globally living with HIV.
Click to open interactive version
What explains changes and differences in health outcomes?
The ‘production’ of health outcomes
Economists often think of health as a ‘stock’ variable relating to the absence of illness or injury. As such, health is often thought of as an individual characteristic beginning with inherited conditions (e.g. genetics) and evolving over time as a function of other inputs, such as environmental conditions and medical care. 3 In general, the inputs for ‘producing health’ fall under the following broad categories:
Health returns to healthcare investment
More information about the provision of healthcare can be found in our entry on Financing Healthcare.
How strong is the link between healthcare expenditure and life expectancy?
One of the most important inputs to health is healthcare. Here we study cross-country evidence of the link between aggregate healthcare consumption and production, and health outcomes.
One common way of measuring national healthcare consumption and production is to estimate aggregate expenditure on healthcare (typically expressed as a share of national income).
This visualization shows the cross-country relationship between life expectancy at birth and healthcare expenditure per capita.
The chart shows the level of both measures at two points in time, about a generation apart (1995 and 2014 respectively). The arrows connect these two observations, thereby showing the change over time of both measures for all countries in the world. As it can be seen, countries with higher expenditure on healthcare per person tend to have a higher life expectancy. And looking at the change over time, we see that as countries spend more on health, life expectancy of the population increases.
Notice that the relationship in this chart seems to follow a pattern of ‘diminishing returns’: the increase in life expectancy associated with an increase in healthcare expenditure decreases as expenditure increases. This means the proportional highest gains are achieved in poor countries with low baseline levels of spending. This pattern is similar to that observed between life expectancy and per capita income.
The countries are color-coded by world region, as per the inserted legends. Many of the green countries (Sub-Saharan Africa) achieved remarkable progress over the last 2 decades: health spending often increased substantially and life expectancy in many African countries increased by more than 10 years. The most extreme case is Rwanda, where life expectancy has increased from 32 to 64 years since 1995 — which was one year after the Rwandan genocide. The graph also shows that the African countries that suffered the most under the HIV/AIDS epidemic — Lesotho, Eswatini, and South Africa — experienced a decline of life expectancy from which they have not yet recovered.
The two most populous countries of the world – India and China – are emphasized by larger arrows. It is interesting to see that in 1995 China achieved already relatively good health outcomes at comparatively low levels of health spending.
The association between health spending and increasing life expectancy also holds for rich countries in Europe, Asia, and North America in the upper right corner of the chart. The US is an outlier that achieves only a comparatively short life expectancy considering the fact that the country has by far the highest health expenditure of any country in the world.
Global Coalition of Public Health Experts and Citizens Announces Formation of World Health Network with Goal of COVID-19 Elimination
Key members of the World Health Network include:
The task force’s COVID-19 elimination strategy calls for governments to bring cases down to sufficiently low numbers so that no community transmission occurs for extended periods of time. It calls on governments of the world to adopt the goal of progressive elimination of COVID and to reject the idea that the global community must learn to «live with the virus.»
«An effective global strategy is required with solidarity and collective action at the individual, local, national, and international levels,» the group writes in the paper. «Many governments’ responses have been shaped by false dichotomies, pitting public health against the economy and collective well-being against individual liberty.»
To help governments achieve elimination, WHN will produce rigorous scientific evidence and guidelines; coordinate international strategies; empower citizens to engage with the public health process; address issues of inequality and inequity; and combat misinformation, nationalism, and exceptionalism.
As part of its launch, WHN will host its Second «Summit to End Global Pandemics,» which will feature lectures and collaborative engagement among members toward best practices to achieve COVID-19 elimination. The Summit will open with a State of the World address by Dr. Bar-Yam, other scientists, concerned parents and community members from around the world, and will feature dozens of breakout sessions on topics in science, communication and technology. RSVP and learn more here: https://www.worldhealthnetwork.global/summit-info.
Throughout the course of the pandemic, WHN members have guided successful elimination efforts in multiple countries. They have advised governments and institutions on best practices, built accessible data analytical platforms, advocated for airborne precautions and school safety, and engaged in public communication and community-based efforts to promote individual and public health.
The COVID-19 pandemic has resulted in nearly 5 million lives lost, left millions of people with persistent symptoms (Long COVID), and has devastated societies, with already disadvantaged communities being hit the hardest. WHN’s efforts will be rooted in short- and long-term prevention, recognizing the importance of preparation and coordination in this increasingly globalized world.
ABOUT THE WORLD HEALTH NETWORK
The World Health Network (WHN) is a global community devoted to protecting health and minimizing harm to individuals and society. It was formed as a people’s task force in response to the COVID-19 pandemic and includes independent scientific advisory and advocacy teams and citizens’ action initiatives. The WHN is guided by compassion, scientific rigor, transparency, social responsibility, and value for life. The WHN advocates for an effective response to achieve progressive elimination of the disease globally.
World health network
Interview with Yaneer Bar-Yam
Cécile Philippe, Institut économique Molinari
Yaneer Bar-Yam is a physicist specializing in complex systems. He received his PhD from MIT and was an Associate Professor of engineering at Boston University until 1997 where he explained how current synthetic diamonds could be grown. In 1997 he founded the New England Complex Systems Institute in order to work on real world complex issues. With the pandemic, he co-founded the World Health Network (see declaration in the Lancet) that pursues the work on complex challenges along with the need for mechanisms for galvanizing and empowering communities.
He is a long time collaborator of Nassim Nicholas Taleb working together to explain risk and opportunity and how to understand them in the real world.
CP: You are an expert on complexity science. By its name, people get the idea that it is complicated but they usually have no idea what we are talking about. Could you take us through what is complexity science, situating it in within science?
YBY: I believe that most people have heard about networks, traffic jams and maybe even more about big data. These have become hot topics and they are all part of complexity science. As recently as 25 years ago, in the 90s, complexity was not recognized as being needed. It was believed that the two traditional methods of science, calculus and statistics, were enough in order to understand the world. There was even talk about the end of science, as it was believed that reality could be grasped fully with calculus and statistics and that everything important had been discovered.
However, increasingly it became apparent that these were not enough. Indeed, underlying those tools are assumptions about the world that are not true. Not only are a set of new mathematical methods needed, they are essential to applying science in the context of many critical real world situations, physical, biological, and social.
Along with these methods comes a strategy for describing the properties of elements that make up a system, their individual behavior. What is missing is the ability to describe the dependencies of elements and how they form collective behaviors. To give you examples, these methods miss the behavior of a flock of birds, market crashes, and clothing fads. The collective behaviors of birds and people are of a different nature that need new tools to be understood.
The emblematic example of such a need has been shown in the case of the transition of liquid water to vapor. While there is a smooth relationship between the density of water and temperature before it boils, it then reaches a point where it jumps suddenly, the boiling point. This is the phase transition. Physicists studied the properties near the transition, and they found that the molecules do not behave in the way the calculus and statistics tools predict they should. It is only when physicist Ken Wilson developed a new tool known as renormalization group that it was possible to have concepts describing the reality. The idea of renormalization group is to look at things as a function of scale. The reason is that at that phase transition point, there are fluctuations on all scales—this means that the molecule motions are coupled to each other across the material in a way that violates the assumptions of calculus and statistics. The material is not smooth, as calculus assumes, and the motion of molecules is not independent, as statistics assumes.
What this and related tools enable us to describe is the fact that in many real-world situations, phenomenon emerge and cannot be described by the behaviors of the individual components only. It makes sense that many systems that we care about work this way, from neurons interacting in the brain, to people interacting in societies. The pattern of their interactions is essential to describe. But recognizing that this requires a different kind of mathematics has been less clear. It has been thought that we could just tweak or improve the calculus and statistics way. But it turns out that this is fundamentally not the case. The same thing is true for many macro phenomena emerging from the interdependence of particles, cells, individuals, companies, etc.
CP: Why does it matter?
YBY: It matters immensely because we can get a better understanding of systems, and our whole civilization is based on the well-functioning of the many systems it is composed of. It helps, on the one hand, to grasp how it works but even more important than that, I believe it makes possible to find ways to improve it. Anyone interested in policy issues knows how much time is spent on thinking and working on improving the system. When one does not know what makes it tick, this work is in the dark. Even worse one can miss important fragilities in the system and/or implement solutions that are going to make the problem worse. These are known as “unintended consequences”. It also helps predicting what might happen in a system. This is what we actually did with the Arab spring in predicting that there would be riots, not because of dictators, but because of the food price increases caused by ethanol policies (turning corn into fuel) along with money flows into the commodity markets as a result of the financial crisis. We have done a lot of work in many areas, and one I have been working on for the last 15 years is the field of pandemics. Because I identified a long time ago, a transition to fragility in a highly connected world.
CP: How did you get interested in pandemics?
YBY: We did an analysis of pathogen evolution in the context of increasing global transportation that was published in 2006. Just as with the boiling of water, there is a transition point at which the system goes from local outbreaks to global extinction. That there is a transition means that people would be unprepared for this happening. A sharp transition means that trends would not show that it will happen and all of a sudden, we would be in a regime where we were vulnerable and it would only be a matter of short time that diseases would appear or evolve to exploit that vulnerability with catastrophic consequences. Since then I have been talking about and engaging in outbreak and infectious diseases control, because our ability to prevent extinction depends on taking effective action that addresses that vulnerability. This means that society has to learn to respond, rather than depending on what the disease itself does.
CP: Why do you think that society can do this?
YBY: I marvel at the level of complexity our societies have reached. It gives me hope for the future because if we have reached such a level of complexity, it means that there are some built-in process that make it possible in principle to survive at that level. Still, it does not mean that our current system will necessarily survive. I have even identified reasons that it might not, i.e. if we were not going to be able to fix problems such as pandemics and other challenges inherently constitutive of increasing complexity. One of those is the incapacity of hierarchies or top/down systems of authority to deal with the increased level of information. Networks with their distributed control structure are needed to replace them.
CP: What do you mean exactly by networks? Is it what you are trying to build within this new organization you’ve co-founded called the World Health Network? Why would it work better than other organization similar to it?
YBY: The essential way an effective network works is to have each individual’s capabilities, both talents and knowledge, to be recognized in the role they play. Individuals vary tremendously in the kinds of tasks they do well. Everything a network does can be a distributed property replacing the kind of central authority model that has been used for thousands of years. In recent centuries the debate/conflict of government forms is mostly about how a leader gets into power, e.g. dictatorship, socialism, communism or democracy. A democracy uses a distributed voting process. However, the purpose of that vote is choosing a few individuals to take power. Compare with how the brain works, there isn’t a “master neuron,” there are over a million billion neurons that are all contributing to the way the brain functions. We are working on developing a network based upon enabling individuals to take the role they are best suited to, fulfilling their unique “superpower.” This is consistent with the general tendency of society in recent decades to build on teamwork, and less on leaders.
CP: Why are pandemics such a danger for our civilization?
YBY: Pandemics are a danger for our societies because there is a risk of ruin or extinction. We need to build robust strategies in order to prevent them. After two years of Covid this should be obvious to everyone in the long-term consequences of this disease, the next variant, or another disease that might follow soon afterwards. As long as the world is sufficiently separated into local regions, the danger of rapid spread of a deadly disease is minimal. It might happen but happens only rarely, like once in a hundred years. But now with global transportation at the rate it is, there is very little barrier to a deadly disease spreading—unless people react fast to stop it. We are still reacting slowly and not doing what it takes to prevent a disease with a rapid spread and a slow but deadly consequence. We are watching this happen with Covid, and people are aware that it has a certain level of lethality over the short term, but in survivors, infection raises the risk of massive deaths from heart attacks and strokes over multiple years. We haven’t prevented that longer-term consequence from happening and it may very well happen. But even if it doesn’t happen for this disease, there is nothing that prevents it from being true about the next outbreak that happens. If we don’t stop such outbreaks, we will certainly go extinct and it won’t take very long for it to happen. This is also happening in other ways with antibiotic resistant diseases that are becoming more severe over time in recent decades. The same analysis holds. Even currently mild endemic diseases can mutate to become more severe and cause extinction. When a system is inherently vulnerable something will surely happen to exploit that vulnerability.
CP: You advocate for elimination. Why? Is it still a possibility when even the few Western countries doing it have given up in the face of a much more contagious variant like Omicron? Any chance of reaching herd immunity at some point?
YBY: Elimination is possible and has become easier even in the face of the Omicron variant because of technological advances and because of the fact that getting ahead of Omicron causes it to decrease faster than previous variants. The rapid transmission is partly due to the shortening of the time from infection to transmission. If we reduce R to be less than one, the shorter interval means cases go down more rapidly.
In contrast, elimination by herd immunity through vaccination has not been possible because of the high rate of transmission and the inability of vaccination to achieve a sufficiently high prevention of transmission in the face of rapidly mutating virus. Herd immunity by infection has been a terrible strategy from the beginning because it accepts the consequence of infecting many people in diseases, hospitalizations, deaths and chronic illness and disability often called long covid, injuring the brain, heart and other organs as well as the immune system.
CP: Elimination is seen as the strategy of those who want to lockdown people. Are there other ways? What do you tell people who are exhausted by a two-year fight?
YBY: The objective of elimination is an exit from the pandemic. The only question is whether we will act together to do this. People also think it is very hard to do so, but the issue is putting our minds and determination to this task. Technology and social action work together to make it possible.
For much of the pandemic the main way to achieve elimination has been through strong lockdowns. Even then, the objective of the lockdown is to open up soon, not stay locked down. But today we also have other methods that are easier. With new technology mass testing to stop transmission is now much more practical with the development of low cost and easy to implement RT-LAMP testing.
You are right to mention New Zealand and Australia – the two Western countries that have openly pursued elimination – because for the first two years thanks to their investment in the first lockdown, they have been better on all fronts: mortality, economics, mobility and even liberties. They have had to implement local and short lockdowns when there were local outbreaks, like putting out a fire when it happens, but all in all they have been better off. Much of the western world failed them. Had others done as they did, there would not have been such a risk of importing cases, or new variants. Everyone would have been at elimination and travel would have been possible. It is, of course, immensely difficult to do elimination by yourself, enduring the challenge of new imported cases, the increasing challenge of new variants, and the desire to travel, and the pressure of well-organized groups willing to pursue “normal” lives with no consideration for others and the society at large.
CP: It has become increasingly difficult to follow the flux of information regarding the pandemics. Which variables do you think are the most important ones to focus on at the society level? at the individual level?
YBY: The most essential variables are the number of cases over time—the value of the transmission rate R (or the rate of change in cases per day), and the rate of transmission from community to community (travel). Hidden in the first variable is the discreteness of cases, because the important thing to know is whether we are at zero or not. Zero leads to ability to open up without restrictions. When there are a lot of cases, we feel we are far away, but exponential decline gets us there very quickly if we don’t stop going before we get to the finish line.
CP: Why is it worth saving the system? We get the impression in the Western world that the system is too rotten to be saved and that it might actually be better to let it collapse. What is your take on that?
YBY: The most important thing is not just the system, but also the values that the system represents. Today we see clearly that the value of life and health has been diminished dramatically. People have started to say, ‘well, it doesn’t matter if a few hundred thousand people die.’ That’s a real problem. And it’s not just a problem because of the fact that we’re losing the value of life, which is very bad, but because it is totally counter to the possibility that civilization will be sustained as a complex entity with complex technologies and all the complex supply chains and all the complex collaborations, scientific and literary and other ones we have around the world.
We should surely restore the value of life and go further in recognizing the value of each individual’s life and wellbeing. This goes hand in hand with recognizing the unique capabilities of individuals, quite different from an industrial model where people are seen as commodities like widgets, the same as parts of the machines they make. Statistics and calculus are not well suited to understanding this distinction, but we can see how badly they treat the importance of individuals, and the value of human life and wellbeing.
CP: Final question: when you think about networks, what make you think that life within networks will be better than otherwise. Is it mostly a question of survival against extinction?
YBY: As I mentioned previously, the network as a complex collective should inherently recognize the value of each individual that is part of it. That is integral to how it works.
ventilation guidelines
Monitor CO2 levels
Measuring Carbon Dioxide (CO2) is the best way to judge the amount of exhaled air in an indoor space; higher levels of CO2 indicate a higher percentage of the air in a room has already been breathed by someone else. Publicly viewable CO2 monitoring devices should be installed in all government/business/public shared indoor spaces (“indoor spaces”). Indoor CO2 levels should not exceed 800 PPM (if no filtering is used) or 1000 ppm, if significant HVAC or portable HEPA filtering is in use.[3]
Enforce occupancy limits
All indoor spaces must specify occupancy limits based on the ability to ventilate the space to target CO2 levels.
Address inadequate ventilation
If an indoor space exceeds the target CO2 limit, the relevant entity must take at least one of the following actions to bring the space into compliance: 1) reduce the maximum occupancy level of the space; 2) improve natural or mechanical ventilation of the space; OR 3) install portable HEPA air cleaners. Number and size of cleaners to be determined based on size, layout, function, and occupancy of space.[4]
Institute an “open windows/doors” policy
Require that windows and doors always be kept open in naturally ventilated indoor spaces, unless there is a safety, security, privacy, health, weather or other significant reason for closing them.
Require high efficiency air filters
Require the use of MERV 13 filters or equivalent (or higher efficiency filters) in all HVAC systems.[5] If the system cannot function with MERV 13 filters, use the highest MERV filter grade that the system will tolerate.
Require respirators
Respirators are more effective than surgical or cloth masks at preventing SARS-CoV-2 transmission. Require the use of N95 or equivalent respirators, including N95, FFP2, KF94, KN95, and elastomeric half masks, in all indoor spaces. Educate building users on the importance of fit and closing gaps between the respirator and the face.
Only use proven air cleaner technologies
Filter-based technologies such as portable HEPA filters, as well as ultraviolet germicidal light (UVGI),[6] that could be used as supplementary treatment when filtration is limited, are proven to work against virus-containing aerosols.[7] Foggers that spray chemicals into the air and electronic air cleaners (ions, plasmas, hydroxyls, photocatalysis) can be harmful and should be avoided.
Establish accountability for protective measures
Fines or penalties should be imposed on organizations that fail to implement COVID-19 measures. Following significant outbreaks among individuals who shared the same indoor space, an audit of ventilation, air cleaning, occupancy, face covering policy implementation should be conducted.
Health professions networks
Health professionals play a central and critical role in improving access and quality health care for the population. They provide essential services that promote health, prevent diseases and deliver health care services to individuals, families and communities based on the primary health care approach. Mechanisms for optimizing the strengths and skills of health professionals will be essential to achieving the Millennium Development Goals.
The World Health Report 2006: Working Together for Health highlighted a worldwide shortage of almost 4.3 million doctors, midwives, nurses and support workers. Thirty-six of the 57 countries with severe shortages are in Africa. Responding to this urgent crisis, the 59th World Health Assembly adopted Resolution WHA59.23 which recognized the “centrality of human resources for health for the effective operation of country health systems” and called for the use of innovative strategies to maximize health professionals’ contributions.
Through networks and partnerships, WHO will:
Health workforce
Health systems can only function with health workers; improving health service coverage and realizing the right to the enjoyment of the highest attainable standard of health is dependent on their availability, accessibility, acceptability and quality.
WHO estimates a projected shortfall of 15 million health workers by 2030, mostly in low- and lower-middle income countries.
However, countries at all levels of socioeconomic development face, to varying degrees, difficulties in the education, employment, deployment, retention, and performance of their workforce.
The chronic under-investment in education and training of health workers in some countries and the mismatch between education and employment strategies in relation to health systems and population needs are contributing to continuous shortages. These are compounded by difficulties in deploying health workers to rural, remote and underserved areas. Moreover, the increasing international migration of health workers may exacerbate health workforce shortfalls, particularly in low- and lower-middle income countries. Human resources for health information systems are often weak to take stock of selected health workers from the public sector.
In some countries, challenges in universal access to health workers may also result from the lack of capacity by the public sector to absorb the supply of health workers due to budgetary constraints. As a result, some countries face the paradox of health worker unemployment co-existing with major unmet health needs.
The High-Level Commission on Health Employment and Economic Growth identified six pathways by which investments in the health and social workforce can spur inclusive economic growth. The health workforce has a vital role in building the resilience of communities and health systems to respond to disasters caused by natural or artificial hazards, as well as related environmental, technological and biological hazards and risks. Seventy per cent (70%) of the health and social workforce are women and investing in the health workforce is an opportunity to create decent employment opportunities, in particular for women and youth.
The Global Strategy on Human Resources for Health: Workforce 2030 is the key guiding document with principles and objectives presented below:
Working for Health Programme
The Working for Health Programme is a joint partnership between the World Health Organization (WHO), International Labour Organization (ILO) and the Organization for Economic Co-operation and Development (OECD) to expand and transform the health and social workforce to drive inclusive economic growth and achieve the Sustainable Development Goals (SDGs).
Working for Health contributes to universal health coverage and to SDG 3, 4, 5 and 8 (health, education, gender equality, decent work and economic growth) through the Five-Year Action Plan on Health Employment and Inclusive Economic Growth 2017-2021. In 2020, Working for Health supported thirty-two countries and two regional economic areas namely, the Southern African Development Community and the West African Economic and Monetary Union. The Working for Health Programme supports strengthening health workforce data globally through the International Platform on Health Worker Mobility Platform on Health Worker Mobility and Inter-Agency Data Exchange (IADEx).
The Global Health Workforce Network
The WHO led/coordinated network Global Health Workforce Network was established in 2016, following a request by Member States and building on a proposal by the Board of the Global Health Workforce Alliance. The Network operates within WHO as a global mechanism for stakeholder consultation, dialogue and coordination on comprehensive and coherent health workforce policies in support of the implementation of the Global Strategy on Human Resources for Health and the recommendations of the Commission.
Key national and local partners
Key international partners
International Labour Organization (ILO), The Organisation for Economic Co-operation and Development (OECD), The World Bank, The United Nations Children’s Fund (UNICEF), The European Union (EU), International NGOs.
Long COVID Research databank
Are you passionate about following the latest research on Long Covid? Are you inspired to help further public understanding of the risks of Long Covid on a global scale? The World Health Network and its partners are recruiting volunteers to join us in investing in a centralized research library on the long-term effects of SARS-CoV-2 infection. This Long Covid Research Databank will become an asset for WHN’s entire network of science and advocacy organizations, offering clearly summarized scientific findings in a format accessible to the general public.
It’s fantastic if you have scientific, medical, communications, or web design and development expertise to bring to the community, but all volunteers are welcome. We encourage all who are interested to join our effort regardless of background or how much time you have to contribute.
- Volunteers submit new research to the Long Covid Research Databank, with each study receiving its own dedicated forum for relevant links, media references, excerpts, and a space for discussion. «, «button»: < "buttonText": "Make It", "buttonLink": "#" >, «imageId»: «627450db8393271cc2e3116b», «image»: < "id": "627450db8393271cc2e3116b", "recordType": 2, "addedOn": 1618497398784, "updatedOn": 1618497398838, "starred": false, "passthrough": false, "workflowState": 1, "publishOn": 1618497398784, "authorId": "5fee44274fa6a530d78f873c", "systemDataId": "1618497259178-6XJGK9GR6YAVBQL5L519", "systemDataVariants": "2500x1518,100w,300w,500w,750w,1000w,1500w,2500w", "systemDataSourceType": "JPG", "filename": "20140301_Trade-151_012-2.jpg", "mediaFocalPoint": < "x": 0.5, "y": 0.5, "source": 3 >, «colorData»: < "topLeftAverage": "ebf1f3", "topRightAverage": "f7fbfc", "bottomLeftAverage": "807855", "bottomRightAverage": "1f261d", "centerAverage": "698aa5", "suggestedBgColor": "e4ecee" >, «urlId»: «fflfv7rqfrdrlxls2s4e7a3oawvosd-ef442-gjl6c», «title»: «», «body»: null, «likeCount»: 0, «commentCount»: 0, «publicCommentCount»: 0, «commentState»: 2, «unsaved»: false, «author»: < "id": "5fee44274fa6a530d78f873c", "displayName": "NECSI Programs", "firstName": "Kim", "lastName": "Severino", "avatarUrl": "https://static1.squarespace.com/static/images/5fee44271c60c7508813506d", "bio": "", "avatarAssetUrl": "https://static1.squarespace.com/static/images/5fee44271c60c7508813506d" >, «assetUrl»: «https://images.squarespace-cdn.com/content/v1/5ec321c2af33de48734cc929/1618497259178-6XJGK9GR6YAVBQL5L519/20140301_Trade-151_012-2.jpg», «contentType»: «image/jpeg», «items»: [ ], «pushedServices»: < >, «pendingPushedServices»: < >, «recordTypeLabel»: «image», «originalSize»: «2500×1518» > >, < "title": "Experts Review studies", "description": "
How it works «, «spaceBelowSectionTitle»: < "value": 70, "unit": "px" >, «sectionTitleAlignment»: «left», «isSectionButtonEnabled»: false, «sectionButton»: < "buttonText": "Make It", "buttonLink": "#", "buttonNewWindow": false >, «sectionButtonSize»: «large», «sectionButtonAlignment»: «left», «spaceAboveSectionButton»: < "value": 70, "unit": "px" >>» data-media-alignment=»left» data-title-alignment=»left» data-body-alignment=»left» data-button-alignment=»left» data-title-placement=»center» data-body-placement=»center» data-button-placement=»center» data-layout-width=»full» data-title-font-unit=»rem» data-description-font-unit=»rem» data-button-font-unit=»rem» data-space-between-rows=»60px» data-space-between-columns=»60px» data-vertical-padding-top-value=»3.3″ data-vertical-padding-bottom-value=»3.3″ data-vertical-padding-top-unit=»vmax» data-vertical-padding-bottom-unit=»vmax» >
Volunteers Submit Research
Volunteers submit new research to the Long Covid Research Databank, with each study receiving its own dedicated forum for relevant links, media references, excerpts, and a space for discussion.
Experts Review studies
Medical and science experts review studies to vet the credibility of the research, summarizing the takeaway in a one-bullet format approachable for «laypeople» without scientific training.
Research is shared
Research summaries are published to a new website under development by the World Health Network once «cleared» by our triage and expert review teams — ready to be put to work in our advocacy to change what «living with Covid» safely looks like in the years ahead.
Ready to help us build this resource together? Share your contact information with us and we’ll reach out via email to introduce you to the World Health Network and discuss how you’d like to contribute to the Long Covid Research Databank. You can also ask questions prior to joining by contacting the project coordinator Greg Howard on Twitter.
A Network Connecting Health Care Professionals
Connecting Millions Of MDs, Hospitals and Clinics
sign up
log in
Welcome to WebHealth Network
WebHealth Network is a leading provider of credible information about health subjects that matter to you. You can use WebHealth Network as your «one-stop-shop» for all information related to staying healthy. The site is an aggregation of content from the most trusted providers on the web. WebHealth Network is intended for educational purposes only. The site does not provide medical advise, diagnoses, or treatment.
Search, view and contact Pharmacies, hospitals, clinics, and labs by name and location.
Search and View Clinical Trials by topic, date or condition.
Designed for customer-centric providers, service providers, and others that want to learn, grow their business.
Continuing medical education training with videos.
Quick Links
About
Network Sites
Partner Offers
Additional
WebHealth Network
WebHealth Network is the leading aggregator of health, fitness, and wellness news and information from across the Web. We provide our readers with the deepest access to health information from the most trusted health publishers.
We aim to be a one stop for all the info you need to stay healthy.
Our sources include hundreds of blogs, health sites, government sites, pharmaceutical manufacturers and much more. All the information provided is publicly available and is updated daily.
Not a Substitute for Medical Advise
WebHealth Network is designed for educational purposes only. The information provided is not a substitute for professional medical advise, diagnoses, or treatment. If you are experiencing problems with your health, it is recommended that you consult a medical professional, doctor, or other health care professional. Do not delay or avoid seekeing medical advise from a professional because of any information listed on WebHealth Network. The use of the information provided on the site is at your own risk.
Ongoing medical research may change or impact the information listed on WebHealth Network. No assurances are provided that the information listed will include the most updated developments.
If you are you are experiencing a medical emergency, please call your health care professional immediately.
Isolation Guidelines
Gold Standard Recommendation for Isolation
Following a SARS-CoV-2 positive test (antigen or PCR) an individual completes a minimum of a 14-day [1] isolation
Isolation ends when both of the following conditions are met:
No symptoms for three days[2]
Two sequential negative PCR tests spaced 24-hours apart (each test should include samples taken from two sources).
Federal or state coverage of lost wages to support the absence.
After release from isolation, the individual continues to follow preventive guidelines including getting vaccinated, wearing a high quality mask, and avoiding meeting others indoors.
The above gold standard provides strong assurance that SARS-COV2 transmission will not take place from identified cases.
The World Health Network, guided by the scientific advice of the Covid Action Group, made these recommendations in response to the 12/27/21 revised CDC Update that reduced SARS-COV2 positive individuals’ isolation time to 5 days[3]. The recommendations are intended for local public health officials in the United States as well as globally who consider using the CDC’s recommendation without adapting it to their context and the latest scientific knowledge. The CDC’s changed recommendation for isolation of 5 days has not been justified based upon scientific analysis of the prevention of transmission, but rather on employer staffing needs due to substantial numbers of infected individuals. A recent study makes clear that even with only a few samples, a signature of infectiousness—the ability to culture viable virus—can be found in Omicron cases up to 9 days after infection [4], and evidence of infectiousness in an Omicron patient has been cited at up to 12 days [5]. Moreover, the idea that such an isolation would enable workers to support economic activity is undermined by outbreaks in the workplace, infection of service customers and housemates, and others encountering those who stop isolation prematurely. Rejection of the reduction to a 5 day isolation standard by individuals, institutions and corporations is essential to control infections.
↑ There is some but very limited scientific evidence for a reduction from 14 days to not less than 10 days of isolation (see next section). Our review of the studies often cited for a 10 day isolation, indicates very few relevant studies with poor statistics as well as evidence of longer periods of infectiousness. Thus, we recommend a 14 day gold standard isolation period. Where a reduction to 12 or 10 days is proposed, additional careful monitoring and guidelines for precaution should be adopted.
↑ Where individuals have symptoms that do not resolve for extended times, medical evaluation of their condition is necessary.
↑ Active epidemiological investigation on SARS-CoV-2 infection caused by Omicron variant (Pango lineage B.1.1.529) in Japan: preliminary report on infectious period, National Institute of Infectious Diseases Disease Control and Prevention Center, National Center for Global Health and Medicine, https://www.niid.go.jp/niid/en/2019-ncov-e/10884-covid19-66-en.html
↑ Taiwan rejects US CDC guidance on 5-day quarantine, identifies Omicron infected individual who is infectious at 12 days: https://www.taiwannews.com.tw/en/news/4393548
Scientific explanation
A recent controversial reduction in the recommended period of isolation by the CDC to 5 days and no-test exit criteria have resulted in many symptomatic individuals exiting isolation prematurely and returning to the workplace. This has raised concerns about both the absence of a scientific basis, and the lack of motivation to protect individuals and institutions. There is no scientific study that has justified a reduction to the 5 day CDC policy.
Here we review the literature about infectious periods and show that it provides sound justification for a 14 day isolation policy with a multiple test exit condition. There are several scientific studies supporting a reduction to no less than 10 days. We review this literature and conclude that the reduction to 10 days is weakly justified due to limited samples and poor statistics. Our conclusion is that the gold standard should be a 14 day isolation period. We note, however, that whether a 14 day, 12 day or 10 day minimum isolation period is adopted, it is essential to reject the 5 day isolation period.
Measures of infectivity include detection of the presence of virus as measured by PCR or antigen tests, with PCR or other nucleic acid tests being the best standard. Reviews of the literature primarily for the original variant indicate that the typical time from positive to negative tests is 14 days, with an extended tail of the distribution to longer times 1. More precisely, the estimated mean time from symptom onset to two negative RT-PCR tests was 13.4 days (95% CI 10.9 to 15.8). Estimated mean duration from symptom onset to hospital discharge or death (potential maximal infectious period) was 18.1 days (95% CI 15.1 to 21.0); time to discharge was on average 4 days shorter than time to death, which provides a consistent estimate for the expected mean of 14 days of infectiousness. The long tail of positive tests is manifest in many reports of individuals manifesting symptoms of disease and of serial positive tests extending to over 20 days of infectiousness [1,4]. Noting the 95% upper bound of confidence intervals of the expected mean time at roughly 16 and 21 days, and the extended tail of infectiousness for some individuals as well as continued positive tests, the 14 days is a conservative value for isolation periods.
Indeed, since this is only a typical value, individual infectiousness must be evaluated through testing before exit from isolation. The need for two negative tests and two different sampling sources separated by 24 hours results from stochastic viral densities, i.e., randomness in their presence at any particular time, so test results are stochastic as well. The false negative rates of RT-PCR are approximately 30%, and this is higher for lower viral densities, necessitating multiple tests with different samples [5,6].
It has been argued in the literature that infectiousness decreases toward the end of the period of time of positive PCR tests due to the existence of non-viable fragments of virus rather than viable virus [7,8]. This has been used to justify reducing the isolation period to a minimum of 10 days and that testing should not be used as a criterion for release from isolation. The degree to which this reduction from 14 days to 10 days occurs reliably across the population has not been empirically shown, with very few samples reported in the literature between 10 and 14 days (9 mild cases from which 9 samples were taken with a low probability of detecting viable virus in samples even during the known infectious period in Ref. [7], 6 or 7 samples of which only one was taken at 10 days without any study of the reliability of virus detection during infectiousness in Ref [9], and even manuscript errors in not reporting positive tests at 14 days [see Supplement of 10]). The linkage of reduction in viability fraction to infectiousness, as an additional factor to the detection of virus by PCR, has also not been shown empirically. Indeed, a variety of observations, including of young healthy individuals with mild symptoms, show individuals can continue to consistently have viable virus or be infectious for over 20 days [1,4,11], which undermines the arguments in favor of reduction of isolation times, and surely the justification of not using an exit test. Thus, it is important both to establish a longer period of isolation than the weakly justified minimum of 10 days and to continue to use testing as an exit condition from isolation.
A 14-day isolation period should be a minimum requirement to avoid releasing individuals from isolation prematurely, particularly for the rapidly spreading Omicron variant, which is highly prone to superspreader events, and for whom the parameters of infectious periods are not established empirically and therefore may be shorter or longer. In the presence of uncertainty, the adoption of more conservative guidelines is justified. New studies should be devoted to determining the range of infectious periods for this particular variant.
World health network
International Clinical Trials Registry Platform (ICTRP)
Important information about the COVID-19 outbreak
The Search Portal is currently down because of an emergency maintenance update which may take a few days. Please keep checking this page for updates.
Related links
The mission of the WHO International Clinical Trials Registry Platform is to ensure that a complete view of research is accessible to all those involved in health care decision making. This will improve research transparency and will ultimately strengthen the validity and value of the scientific evidence base.
The registration of all interventional trials is a scientific, ethical and moral responsibility.
What is a clinical trial?
For the purposes of registration, a clinical trial is any research study that prospectively assigns human participants or groups of humans to one or more health-related interventions to evaluate the effects on health outcomes. Clinical trials may also be referred to as interventional trials. Interventions include but are not restricted to drugs, cells and other biological products, surgical procedures, radiologic procedures, devices, behavioural treatments, process-of-care changes, preventive care, etc. This definition includes Phase I to Phase IV trials.
What is trial registration?
WHO regards trial registration as the publication of an internationally-agreed set of information about the design, conduct and administration of clinical trials. These details are published on a publicly-accessible website managed by a registry conforming to WHO standards.
World health network
From the 2016 UNICEF report:
The sheer numbers of children affected (by indoor and outdoor pollution) are staggering. Based on satellite imagery, in the first analysis of its kind, this report shows that around the world today, 300 million children live in areas with extremely toxic levels of air pollution. Approximately 2 billion children live in areas where pollution levels exceed the minimum air quality standards set by the World Health Organization. These data don’t account for the millions of children exposed to air pollution inside the home.
Together, outdoor and indoor air pollution are directly linked with pneumonia and other respiratory diseases that account for almost one in 10 under-five deaths, making air pollution one of the leading dangers to children’s health.
From a 2016 report on the economic costs of certain health issues caused by exposure to indoor dampness and mold in the U.S.:
This researcher estimated the costs of allergic rhinitis, acute bronchitis and asthma caused by exposure to indoor dampness and mold in the U.S. He used two methods—cost of illness (COI) and willingness to pay (WTP).
WTP measures the full cost to society, but WTP estimates are difficult to compute and rarely available. COI methods are more often used but less likely to reflect full costs.
Based on the data available, he estimates the total annual costs as follows:
From a 2016 World Health Organization report:
The report states that “92% of the world’s population lives in places where air quality levels exceed WHO limits.”
Some 3 million deaths a year are linked to exposure to outdoor air pollution. Indoor air pollution can be just as deadly. In 2012, an estimated 6.5 million deaths (11.6% of all global deaths) were associated with indoor and outdoor air pollution together. [ Note from GIHN : The 11.6% statistic relates to only five types of pollutants.]
From a November 12, 2016, article about the effects of indoor and outdoor pollution in India:
Studies across the world and also in India prove that outdoor and indoor air pollution is a serious environmental risk factor that causes or aggravates acute and chronic diseases and has been identified as the fifth highest cause of morbidity in India.
Four kids could be dying every hour in UP (Uttar Pradesh ) of pneumonia caused by respirable suspended particulate matter (PM) 1, 2.5 and 10, which form a large part of the air we breathe. Alarmingly, the number adds up to 104 deaths per day and 38,000 a year.
From a 2015 report from the Centre for Science and Environment (CSE) in India:
Air pollution is responsible for 10,000-30,000 deaths in Delhi annually and is the fifth largest cause of death in the country.
Outdoor air pollution kills 620,000 people, and indoor air pollution kills 1.5 million people in India annually.
From a 2015 World Health Organization report:
From a 2015 report by the United Kingdom: National Institute for Health and Welfare:
This report highlights the impact of indoor pollutants on disease and life expectancy. The study concludes that indoor air pollution is potentially responsible for the annual loss of over 200,000 healthy life years in the U.K.
In a recent Pan-European study, they estimate that exposure to indoor pollutants is linked to reduced life expectancy and burden of disease (57% of the total burden relates to cardiovascular diseases, 23% to lung cancer, 12% to asthma and the remaining 8% is in association with other respiratory conditions).
From a 2012 report from Finland:
The estimated cost of health problems associated with mould and damp is 450 million euros each year. If you add the cost of repairing the problem, the total reaches 1.4 billion euros.
The recent publication of the Audit Committee of the Finnish Parliament indicated that approximately 7–9% of terraced houses; 6–9% of apartment buildings; 12–18% of schools and kindergartens; 20–26% of nursing homes, hospitals, and outpatient departments; and 2.5–5% of offices have been significantly damaged with dampness and are infested with indoor molds.
It has been estimated that approximately 800,000 or every seventh Finnish citizen has been exposed to some extent and become sensitized to compounds present in poor quality indoor air. However, since there is no ICD-10 coding system for mold-related illness, its exact incidence is unknown. If one extrapolates from the above presented figures, one could argue that the incidence of mold-related illness may be much higher than the incidences for cardiovascular conditions, cancers, and accident-induced traumas.
From a March 25, 2014 press release by the World Health Organization (WHO):
In particular, the new data reveal a stronger link between both indoor and outdoor air pollution exposure and cardiovascular diseases, such as strokes and ischaemic heart disease, as well as between air pollution and cancer. This is in addition to air pollution’s role in the development of respiratory diseases, including acute respiratory infections and chronic obstructive pulmonary diseases.
About 12% of new childhood asthma in Europe can be attributed to indoor mould exposure, which represents approximately 55 842 potentially avoidable DALYs (Disability-Adjusted Life Years) and 83 potentially avoidable deaths per year.
About 15% of new childhood asthma in Europe can be attributed to indoor dampness, which represents approximately 69 462 potentially avoidable DALYs and 103 potentially avoidable deaths per year.
Some 4.8 million (22%) of England’s 22 million dwellings were identified as having a Category 1 HHSRS (Housing Health and Safety Rating System) hazard and thus by our definition deemed to be ‘unhealthy housing’.
The total cost of dealing with HHSRS Category 1 hazards in the English housing stock is some £17.6 billion.
From a 2017 report about the costs relating to asthma and chronic obstructive pulmonary disease (COPD) in Europe:
Today, one out of six Europeans – or the equivalent of Germany’s population – reports living in unhealthy buildings, i.e., buildings that have damp (leaking roof or damp floor, walls or foundation), a lack of daylight, inadequate heating during the winter or overheating problems. In some countries, that number is as high as one out of three.
The entire respiratory system becomes vulnerable when exposed to poor indoor air quality, which can provoke the onset of various respiratory illnesses and even raise the risk of developing non-respiratory diseases. In fact, people are 40% more likely to have asthma when living in a damp or mouldy home.
They estimated the annual cost of asthma and chronic obstructive pulmonary disease at €82 billion ($93 billion).
From a January 27, 2010 article posted on Wire Service Canada:
From a 2008 report from Canada about the environmental burden of disease:
Estimates of the environmental burden of disease focused on four major categories of disease (i.e., respiratory disease, cardiovascular illness, cancer and congenital affliction). They presented the following estimates:
From the Mold Resources page on the U.S. EPA website:
One third to one half of all structures have damp conditions that may encourage development of pollutants such as molds and bacteria, which can cause allergic reactions — including asthma — and spread infectious diseases.
From a 1994 report on PROPOSED rules by OSHA (standards addressing indoor air quality in indoor work environments). On December 17, 2001, OSHA withdrew this proposal.
Based on the information submitted to the docket, OSHA assumed that 30 percent of the buildings have indoor air quality problems.
Based on OSHA’s percentage of problem buildings (30 percent), OSHA assumed that 30 percent of employees working indoors are exposed to poor indoor air quality. Therefore, the number of employees potentially affected is 21 million.
From an August 17, 2016, article about the United Kingdom’s National Clean Air Day:
Emeritus Professor Derek Clements-Croome of Reading University shared the results of a BESA 2016 survey that showed 70% of office workers were concerned with the impact of poor IAQ. The results of the survey also showed:
From a 2016 report by United Kingdom’s Royal College of Physicians:
In this report, they discuss the impact of indoor air pollution and also mention new indoor air pollutants that need to be considered such as advanced materials and three-dimensional printing.
The multiplicity of contaminants can make it more problematic to determine the precise source of an exposure-triggered illness and more difficult for epidemiologists to quantify cases. However, the report estimates indoor air pollutants “cause, at a minimum, several thousands of deaths per year in the U.K., and associated with healthcare costs in the order of tens of millions of pounds.”
In the report, they estimate that 40,000 deaths per year are attributable to outdoor air pollution, with an annual cost of 20 billion pounds. And, they also include information about indoor air pollutants (including radon, tobacco smoke, carbon monoxide, lead, nitrogen dioxide, particulate matter, PCBs, VOCs, formaldehyde, asbestos, kitchen products, faulty boilers, open fires, fly sprays, air fresheners, biological materials, mould, etc.).
«When our patients are exposed to such a clear and avoidable cause of death, illness and disability, it is our duty as doctors to speak out.»
From a report by the Organisation for Economic Co-Operation and Development (OECD) in Africa:
The annual number of deaths from outdoor pollution rose 36% from 1990 to 2013. Deaths from indoor air pollution rose 18% during that same time period.
From a 2016 report by the World Health Organization (this is an update to their 2006 report on Preventing Disease Through Healthy Environments):
The report includes the following statistics for deaths attributable to the environment:
They point out in the paper that statistics are not available for deaths due to each of these specific causes, so the estimates are largely based on surveys of expert opinion.
Although these estimates reflect only a few select environmental causes (i.e., primarily climate change, fossil fuel consumption, safe water and sanitation) imagine how large the percentage might be if they include all environmental factors.
From a 2012 report on dampness and mold in European housing:
The percentage of homes in 31 European countries that are affected by damp, mold or water damage. This report concluded that 12.1% of homes had damp, 10.3% had mold and 10.0% had water damage, giving a result of 16.5% for a combination of these indicators.
Significant (up to 18%) differences were observed for dampness and mold prevalence estimates depending on survey factors, region, and climate. In conclusion, dampness and/or mold problems could be expected to occur in one of every six of the dwellings in Europe.
From a 2016 report on the financial impact of endocrine-disrupting chemicals:
Accounting for probability of causation, in the European Union, organophosphate pesticides were the largest contributor to costs associated with EDC exposure ($121 billion), whereas in the USA costs due to pesticides were much lower ($42 billion).
From a report by the CPSC (Consumer Product Safety Commission):
Most information about sources and health effects of biological pollutants is based on studies of large office buildings and two surveys of homes in northern U.S. and Canada. These surveys show that 30% to 50% of all structures have damp conditions which may encourage the growth and buildup of biological pollutants. This percentage is likely to be higher in warm, moist climates.
From the 2009 World Health Organization report:
Indoor air pollution – such as from dampness and mould, chemicals and other biological agents – is a major cause of morbidity and mortality worldwide. About 1.5 million deaths each year are associated with the indoor combustion of solid fuels, the majority of which occur among women and children in low-income countries.
The prevalence of indoor dampness varies widely within and among countries, continents and climate zones. It is estimated to affect 10–50% of indoor environments in Europe, North America, Australia, India and Japan. In certain settings, such as river valleys and coastal areas, the conditions of dampness are substantially more
severe than the national averages for such conditions.
From a 1989 report by the Special Legislative Commission on Indoor Air Pollution, The Commonwealth of Massachusetts:
Indoor air pollution is a growing problem in the United States and accounts for up to 50% of all illnesses.
Indoor air pollution seriously threatens public health. Scientific testimony and information provided to the Commission shows that many diseases and symptoms are attributable to indoor air pollution: irritation of the eyes, nose and throat, headaches, fatigue, nausea, asthma, emphysema, pneumonia, lung cancer, heart disease, chemical sensitivity, liver and central nervous system damage and many other ailments. As a result, billions of dollars are spent annually on pollution abatement and health care costs resulting from indoor air pollution.
From a 2010 report by Berkeley Lab:
From a 2007 joint study conducted by the EPA and Berkeley National Laboratory:
Building dampness and mold raised the risk of a variety of respiratory and asthma-related health outcomes by 30 to 50 percent.
Of the 21.8 million people reported to have asthma in the U.S., approximately 4.6 million cases are estimated to be attributable to dampness and mold exposure in the home.
NIOSH has estimated that 29% to 33% of new-onset adult asthma is attributable to work-related exposures and 23% of existing adult asthma is exacerbated by work. If occupants develop asthma or asthma exacerbation while working in damp buildings, medical treatment may not be effective if the occupant continues to be exposed. An occupant in damp buildings with allergic asthma may experience symptoms after exposure to very low levels of a sensitizing agent that may still be present after remediation; in such cases, an occupant may require relocation to another area.
From a 2010 report by the World Health Organization on second-hand smoke:
Worldwide, 40% of children, 33% of male non-smokers, and 35% of female non-smokers were exposed to second-hand smoke in 2004. This exposure was estimated to have caused 379,000 deaths from ischaemic heart disease, 165,000 from lower respiratory infections, 36,900 from asthma, and 21,400 from lung cancer.
603,000 deaths were attributable to second-hand smoke in 2004, which was about 1.0% of worldwide mortality.
47% of deaths from second-hand smoke occurred in women, 28% in children, and 26% in men.
From a June 18, 2017, article about leaky buildings and hidden mould in New Zealand:
New Zealand’s leaky buildings, which have been widely attributed to lax building regulations and sub-standard materials, include schools, prisons, and government buildings, as well as an estimated 100,000 New Zealand homes.
Experts agree that leaky homes are still being built in New Zealand, and the health costs from them could reach into the billions.
From the CDC and the Be Tobacco Free organization:
More than 480,000 people in the United States die from tobacco use each year.
Smoking cigarettes kills more Americans than alcohol, car accidents, HIV, guns, and illegal drugs combined.
More than 20 million Americans have died because of smoking since 1964, including approximately 2.5 million deaths due to exposure to secondhand smoke.
During 2016, about 258 billion cigarettes were sold in the United States.
From the American Cancer Society:
Approximately 2.5 million deaths due to exposure to secondhand smoke.
World health network
Wiki-центр TAdviser приглашает редактора блока NNM.
Компании могут зарегистрировать свои системы и проекты в каталоге TAdviser/NNM бесплатно. Раздел находится в оперативном режиме обновления.
Несмотря на снижение объемов, российский рынок продолжает развиваться. Растет объем данных, а значит, увеличивается нагрузка на сети. Так, рынок систем хранения данных за 2013 г. в России поднялся на 11% до 473,4 петабайт. Растет и протяженность сетей. Согласно данным Федеральной службы государственной статистики, в 2012 г. количество рабочих станций увеличилось в среднем на 7–8%, 80% из них находятся в составе локально-вычислительных сетей. Активно развивается и рынок WLAN, осуществляется переход на новые стандарты, в частности, на 802.11n. Централизация управления беспроводных локальных сетей становится также актуальной. Возрастают показатели спроса на облака и виртуализацию. Среднегодовой темп роста российского рынка облачных технологий составляет 50%. Популярностью пользуются гибридные облака, предполагающие применение собственной инфраструктуры наряду с технологиями провайдера.
В результате активного развития на предприятиях растет нагрузка на сеть, следовательно, на приложения и устройства. Параллельно с этим увеличиваются требования к скорости обработки данных, работе сети, серверов, приложений и хранилищ данных. Эта тенденция сохранится в ближайшем будущем. Удовлетворить возрастающую потребность в работоспособности сети можно в случае постоянного контроля и анализа работы компонентов инфраструктуры, поэтому решения мониторинга сети, работы приложений и серверов жизненно необходимы для современного бизнеса. Зачастую они бывают узконаправленными: только мониторинг сети или работы серверов и приложений, тогда как современные сетевые инфраструктуры достаточно сложны и продолжают усложняться с развитием технологий. Система должна учитывать разнообразие архитектуры сетей, мультивендорный набор устройств. При выборе продукта необходимо ориентироваться на приобретение комплексного решения, которое позволяет отслеживать работу различных устройств и компонентов инфраструктуры.
Introducing The Global Health Network: a knowledge-sharing digital platform
The Global Health Network is a digital platform that aims to advance research by providing a mechanism that facilitates collaboration and resource-sharing in global health research.
About the author: Astrid Erber is the coordinator of the NTDs section of The Global Health Network. She is also a doctoral candidate at the University of Oxford, with research interests in clinical trial methodology in an LMIC context, and the evaluation of diagnostics for parasitic diseases under field conditions.
Two weeks ago, I sat in the audience of a session on mapping neglected tropical diseases (NTD) at the Royal Society for Tropical Medicine and Hygiene (RSTMH) biennial meeting in Oxford, chaired by Prof. Simon Brooker from the London School of Hygiene & Tropical Medicine and head of GAHI, together with Prof. Bundy from the World Bank and Ms. Jacobson from the Bill & Melinda Gates Foundation. In this session, the progress towards control and elimination for many NTDs was mapped out: Dr. Seddoh of the International Finance Corporation was talking about the cost of controlling NTDs in sub-Saharan Africa, Mr. Deribe of the Brighton and Sussex Medical School presented data on modelling of podoconiosis risk in Ethiopia, and Dr. Walker from Sightsavers gave a presentation on the Global Trachoma Mapping Project.
I couldn’t help but feel impressed at all those collaborative efforts and the progress made so far. I am coordinating an area dedicated to NTD research on The Global Health Network, which complements my work towards a doctorate in tropical medicine with a focus on parasitic diseases very well.
The Global Health Network is a thriving system of connected, yet individual, web-based areas that are each led by research groups from all over the world. Each of The Global Health Network’s initiatives focuses on a specific therapeutic area (such as respiratory disease, maternal health, or oncology), type of research (for example, diagnostics or microbiology), or are cross-cutting research support communities (such as clinical trials or bioethics). The Global Health Network can transform research by enabling researchers to share methods across staff levels, communities, regions, diseases and disciplines of global health. A dedicated sub-site focusing on Neglected Tropical Diseases was established to specifically address the needs of that community.
Dissemination of knowledge and results is considered a core element of our work. Already a challenge in high income environments, we believe that it might take a bit more time for it to be adapted in LMIC settings due to various constraints. For that reason, TGHN has established regional faculties and is running workshops in LMICs in collaboration with them. These workshops are great – very lively and focusing on specific topics within a country context. At the same time, often these outcomes are shared online with others in similar settings.
We are specifically paying attention to openness and-low tech access, in order to avoid a top-down approach – because this is not what TGHN is about! The websites offer access to high-quality guidance, all free: protocols, very popular e-learning courses in a new training centre, they are often donated by institutions and adapted for TGHN), process maps, a so called site-finder application to link up research sites and projects, and much more. All material is peer-reviewed to ensure quality standards. TGHN aims to build global ‘communities of practice’ by providing a neutral, friendly space that allows everyone in research to connect. At the same time, we do rely on people contributing and sharing their knowledge, opinions, materials and tools.
TGHN is very much focused on sharing methods and we believe that open access is very important, specifically within the NTD context: There are much fewer large initiatives and funding opportunities specifically dedicated to these. Sharing of methods and data would ensure that efforts are coordinated instead of merely replicated. Unfortunately, sharing data on an open access basis has challenges – an argument that is often brought up is that, after all, it’s a world where specific research funding is tied to generating and publishing data, as fast as possible. This is why we put the primary focus of the Global Health Network on sharing methods, and more and more often data sharing does come along at a later stage and within a specific setting, if an atmosphere of trust and collaboration has been established between specific persons or groups.
Working within the Global Health Network is fascinating, and seeing a ‘sister initiative’ like GAHI makes me think that this is definitely the way to go forward for research!
World Health Organization
We’ve verified that the organization WorldHealthOrganization controls the domain:
who.int
Pinned
Communication channel for open source community
Data transformer for COVID-19 case counts from Worldometers
2 Updated Aug 30, 2022
Code and actions for generating a COVID-19 case counts dashboard.
0 Updated Aug 30, 2022
Data transformer for COVID-19 case counts from Johns Hopkins University
0 Updated Aug 30, 2022
30 Updated Aug 29, 2022
Data transformer for COVID-19 case counts from WHO
0 Updated Aug 27, 2022
DHIS2-based application to enable secure and flexible metadata exchange between DHIS2 and Go.Data.
2 Updated Aug 26, 2022
Data transformer for COVID-19 case counts from ECDC
0 Updated Aug 26, 2022
R package for retrieving collections from the Go.Data API.
0 Updated Aug 24, 2022
WHO Antenatal Care Guidelines IG
0 Updated Aug 22, 2022
Template used for HL7-defined WHO implementation guides (based on ig-template-base).
2 Updated Aug 22, 2022
People
Top languages
Most used topics
Footer
© 2022 GitHub, Inc.
You can’t perform that action at this time.
You signed in with another tab or window. Reload to refresh your session. You signed out in another tab or window. Reload to refresh your session.
Through dynamic research, collaboration and training, our global network of 16600 clinicians is transforming mental health care worldwide.
Western Pacific, Asia
Western Pacific, Oceania
All regions
| 51.9% |
| 31.3% |
| 3.8% |
| 4.1% |
| 3.1% |
| 2.3% |
| 2.3% |
| 1.1% |
All regions
Schizophrenia and Related Disorders
Disorder Due to Substance Use and Addictive Behaviours
Disruptive Behaviour Disorders
Obsessive-Compulsive and Related Disorders
Feeding and Eating Disorders
Bodily Distress Disorders
World Health Organization Mental Health Atlas 2020
October 28, 2021
Scholarly Output
REGISTER
Join Now!
If you are a practicing mental health or primary care professional, you can register for our network.
Copyright GCP.Network 2021
You will now view GCP.Network in [Language].
Content that is not yet available in [Language] will be displayed in English.
WHO Info 4+
World Health Organization
Screenshots
Description
Have the latest health information at your fingertips with the official World Health Organization Information App. This app displays the latest news, events, features and breaking updates on outbreaks.
WHO works worldwide to promote health, keep the world safe, and serve the vulnerable.
Our goal is to ensure that a billion more people have universal health coverage, to protect a billion more people from health emergencies, and provide a further billion people with better health and well-being.
What’s New
This release introduces filtering in «Publications» page.
Ratings and Reviews
Needs new version
Initially I was pleased with the app, however it has ceased to function in iOS14 on my iPhone. Still works on iOS13.7 on iPad.
Not working on my iPhone 11
This problem started soon after Trump said he was taking the US out of WHO. I try to open the app & it crashes.
I hope WHO is not responding to Trump’s grandiose pout (think of a 2-year-old) by denying Americans access to its app. Many Americans also see Trump as an abomination. His desertion of international cooperative efforts to improve the world is a betrayal of American values.
WHO fights on many fronts against a multitude of horrible diseases that beset our species—diseases that flourish thanks to poverty, poor education, environmental destruction, overpopulation, & governmental corruption. Readers’ need to learn about those diseases & follow their numbers might load the WHO’s servers to a crash point all by themselves. Then the coronavirus plops a ten-kilogram weight into an apparatus set for grams.
I hope it is server overload & not political meddling that has created the crash problem with the WHO app for iPhone 11, & I hope that the problem can soon be resolved.
It’s updated now
Lots of reviews on here saying the app doesn’t give covid19 news and updates. It is updated now and very handy and useful. Also go on their website, you can see some cool data viz. They also have a what’s chatbot. WHO has stepped up in their communication to the public.
App Privacy
Data Not Linked to You
The following data may be collected but it is not linked to your identity:
Privacy practices may vary, for example, based on the features you use or your age. Learn More
Information
English, Arabic, French, Russian, Simplified Chinese, Spanish
World Health Organization: Global Clinical Practice Network (GCPN)
The World Health Organization (WHO) is currently undergoing the 11th revision of the International Classification of Diseases and Related Health Problems (ICD), scheduled to be published in 2015. The ICD is the international standard for health information and enables the global assessment of monitoring and mortality, morbidity and other relevant health parameters. The ICD is also the basis for the official U.S. government classification of health conditions, required for all electronic health-related transactions such as billing and reimbursement.
The WHO Department of Mental Health and Substance Abuse is taking an international and multidisciplinary approach to revising the ICD-11 chapter on Mental and Behavioural Disorders. As part of developing the classification of mental disorders, WHO is undertaking a systematic program of global field studies to improve the chapter’s clinical utility. These field studies will evaluate proposals for ICD-11 in terms of clinician acceptability, clinical utility (e.g., ease of use and goodness of fit), reliability and validity of the draft definitions and diagnostic guidelines. WHO is using both internet-based and clinic-based approaches to field testing.
Psychologists are invited to participate in the internet-based approach by registering for the Global Clinical Practice Network (GCPN), a global network of individual mental health and primary care practitioners. By joining this network, participants will review materials, offer feedback about ideas or concepts that WHO is developing, and be guided through a selection of questionnaires, case-vignettes and/or other materials accessible from their computers. This information will inform WHO’s decisions about the content and structure of the new classification system, as well as how that information is presented to different users.
Once registered, GCPN members will receive requests for participation no more than once a month. Participation will be designed to take approximately 20 minutes on each occasion; it is completely voluntary, and responses will be kept confidential, secure and will not be released to anyone else. Information will be analyzed in aggregate form and used exclusively for the purpose of ICD revision.
Any mental health or primary care professional who has completed his or her training and is qualified to practice in his or her country is eligible to participate in the GCPN. As a part of registration, you will be asked to provide contact information and specific information about your work settings, activities and interests to help determine eligibility for specific studies. Registration is currently available in Arabic, Chinese, English, French, German, Japanese and Spanish, and additional languages will be added as capacity develops.
World health network
COVID- 19 MAP
COVID- 19 REPORT

COUNTRY HEALTH PROFILES
CAUSE OF DEATH MAPS
Alcohol
Click to Select
All Cancers
Click to Select
Alzheimers & Dementia
Click to Select
Anemia
Click to Select
Asthma
Click to Select
Birth Trauma
Click to Select
Bladder Cancer
Click to Select
Brain/CNS cancers
Click to Select
Breast Cancer
Click to Select
Cervical Cancer
Click to Select
Colon-Rectum Cancers
Click to Select
Congenital Anomalies
Click to Select
Coronary Heart Disease
Click to Select
Diabetes Mellitus
Click to Select
Diarrhoeal diseases
Click to Select
Drownings
Click to Select
Drug Use
Click to Select
Endocrine Disorders
Click to Select
Falls
Click to Select
Fires
Click to Select
Hepatitis C
Click to Select
HIV/AIDS
Click to Select
Hypertension
Click to Select
Inflammatory/Heart
Click to Select
Influenza and Pneumonia
Click to Select
Kidney Disease
Click to Select
Leukemia
Click to Select
Liver Cancer
Click to Select
Liver Disease
Click to Select
Low Birth Weight
Click to Select
Lung Cancers
Click to Select
Lung Disease
Click to Select
Malaria
Click to Select
Malnutrition
Click to Select
Multiple Sclerosis
Click to Select
Oesophagus Cancer
Click to Select
Oral Cancer
Click to Select
Other Injuries
Click to Select
Other Neoplasms
Click to Select
Ovary Cancer
Click to Select
Pancreas Cancer
Click to Select
Parkinson’s Disease
Click to Select
Peptic Ulcer Disease
Click to Select
Poisonings
Click to Select
Prostate Cancer
Click to Select
Rheumatic Heart Disease
Click to Select
Road Traffic Accidents
Click to Select
Skin Cancers
Click to Select
Skin Disease
Click to Select
Stomach Cancer
Click to Select
Stroke
Click to Select
Suicide
Click to Select
Tuberculosis
Click to Select
Uterin Cancer
Click to Select
Violence
Click to Select
CAUSES OF DEATH BY REGION
Africa
Click to Select
Click to Select
Europe
Click to Select
Middle East
Click to Select
North America
Click to Select
Oceania
Click to Select
South America
Click to Select
WORLD HEALTH REVIEW
SELECTED COUNTRY COMPARISONS
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
Compare the Top 10 causes of death and see which country comes out on top.
FOLLOW US
OUR DATA : We use the most recent data from these primary sources: WHO, World Bank, UNESCO, CIA and individual country databases for global health and causes of death.
We use the CDC, NIH and individual state and county databases for verification and supplementation for USA data.
Health professions networks
Health professionals play a central and critical role in improving access and quality health care for the population. They provide essential services that promote health, prevent diseases and deliver health care services to individuals, families and communities based on the primary health care approach. Mechanisms for optimizing the strengths and skills of health professionals will be essential to achieving the Millennium Development Goals.
The World Health Report 2006: Working Together for Health highlighted a worldwide shortage of almost 4.3 million doctors, midwives, nurses and support workers. Thirty-six of the 57 countries with severe shortages are in Africa. Responding to this urgent crisis, the 59th World Health Assembly adopted Resolution WHA59.23 which recognized the “centrality of human resources for health for the effective operation of country health systems” and called for the use of innovative strategies to maximize health professionals’ contributions.
Through networks and partnerships, WHO will:
What Is the World Health Organization?
James Lacy, MLS, is a fact-checker and researcher. James received a Master of Library Science degree from Dominican University.
The World Health Organization (WHO) was first proposed in 1945 as a public health agency to be formed as part of the United Nations. WHO’s constitution was ratified on April 7, 1948, marking its official establishment.
WHO categorizes its work into three broad areas of focus:
Main Responsibilities
To support its three main missions, WHO engages in a variety of technical and practical functions related to disease prevention, emergency response, and direct care delivery.
Research
Collection and analysis of public health data represents a cornerstone of WHO’s function in identifying and responding to disease. WHO uses these data to inform disease prevention guidelines, such as vaccination standards.
Based on its research, WHO creates reference information—such as the International Classification of Diseases—that standardize global reporting of illness and disease. WHO also uses its data to develop clinical guides for disease prevention, such as its WHO Model Lists of Essential Medicines, that countries can use to create a comprehensive healthcare system.
WHO’s research extends beyond personal health concerns to encompass issues that impact community health. For example, WHO’s research led to recommendations related to clean air and water standards in 2018.
Disease Prevention
WHO has always focused on disease prevention, beginning with efforts to eradicate vaccine-preventable diseases like smallpox and polio. The organization promotes disease prevention directly and indirectly through initiatives that include:
Emergency Response
Throughout its history, WHO has coordinated global health emergency responses to crises ranging from Ebola to COVID-19. WHO takes a multi-pronged approach to emergency preparedness that includes:
WHO’s emergency response activities extend to natural disasters, wars, and other issues beyond chronic diseases and general wellness.
Who is in Charge?
As an agency of the United Nations, WHO’s governing body – the World Health Assembly (WHA) – includes representatives of every United Nations Member State. WHO’s structure includes an executive board comprised of 34 technically qualified representatives from the various Member States. These members generally possess an extensive background in clinical or public health.
The WHA elects a Director-General every five years. Dr. Tedros Adhanom Ghebreyesus was elected in 2017 for a term that expires in 2022. An Ethiopian, Ghebreyesus is the first WHO Director-General elected from the group’s African region.
WHO also organizes numerous committees and working groups, often dedicated to single-interest initiatives like road safety.
Members
The WHA currently consists of 194 members, one designee from each Member State. Meetings of the WHA and Executive Board may be attended by “non-State actors” (non-governmental organizations, academic institutions, philanthropic organizations, and others) who may observe and make statements to the body, but cannot vote.
To carry out its global mission, WHO engages in “partnerships, networks, and alliances” with a wide variety of groups in various countries to facilitate its ability to coordinate transportation, lodging, and other services.
Funding
How WHO Works with the U.S. Government
WHO works with the United States through WHO’s Pan American Health Organization. This group brings WHO’s mission and resources to all of the Americas. WHO’s work in the U.S. includes providing public health surveillance data to inform decision-making during the COVID-19 pandemic.
On April 14, 2020, U.S. President Donald Trump announced the country would immediately halt funding to WHO, calling for a review of its alleged mishandling of the COVID-19 response. Whether this freeze is temporary, legal, or what will be done with the money instead remains to be seen.
COVID-19 Response
WHO issued its first situation report—a sort of daily status report—regarding COVID-19 on January 20, 2020. This report described a “pneumonia of unknown etiology … detected in Wuhan City, Hubei Province of China” on December 31, 2019. Upon being notified of these pneumonia cases on January 2, 2020, WHO activated its incident management system to provide support within China and the surrounding region to contain and manage the threat.
WHO has subsequently issued more than 90 additional situation reports, each containing surveillance information, statistics, clinical information, and guidelines for responding to the threat in every country around the globe.
Past Emergency Response
WHO specializes in rapid identification of emerging health threats, such as COVID-19, and activation of resources to mitigate the threat. It has successfully identified and responded to previous health emergencies.
On March 12, 2003, WHO issued a global alert about a specific health threat that later came to be known as Severe Acute Respiratory Syndrome (SARS). This early warning may have helped contain the threat, which, like COVID-19, is caused by a coronavirus but which never evolved into a pandemic.
Ebola
In 2014, the Ebola virus caused a large outbreak in western Africa. WHO responded to provide a range of support, including contact tracing, strategy, case management, and dignified burials.
Zika Virus
In 2016, WHO and its Pan American Health Organization jointly rolled out a strategic response to combat the Zika virus throughout the Americas. WHO provided research, prevention and care guidelines, and public health education materials to guide decision-making.
A Word From Verywell
WHO is one of many health-focused organizations you may be hearing about in light of COVID-19. On a national level, while WHO can make data-backed recommendations, the Centers for Disease Control and Prevention (CDC) is the U.S. agency that can actually implement public health decisions for the country.
The information in this article is current as of the date listed, which means newer information may be available when you read this. For the most recent updates on COVID-19, visit our coronavirus news page.
World health network
Cécile Philippe, Institut économique Molinari
Since the advent of Covid-19, I have never been so unfree. Since March 2020, I have lost many of my freedoms, not so much because the French state has imposed major restrictions over the past few months, but because I don’t want to catch Covid for a variety of reasons, nor to pass it on to others. This has forced me to completely reorganize my life and that of my family, and in the end, despite the precautions I have taken, I have recently been infected. The paradox of this situation is that I was ultimately freer when the virus was circulating at a low level, thanks to mitigation measures, than I was when it was allowed to circulate without them. I was more likely to achieve my goal as long as society was collectively choosing to try to contain the infection. But this choice has been abandoned in the name of freedom, and I never cease to wonder about the meaning of this freedom regained by some and lost by others. I might as well say that this collective choice reduces even more the space of freedom to which I aspire and does not constitute a victory.
What am I supposed to complain about, since my isolation is only due to my personal choices? I don’t want to get infected. That’s fine. It’s up to me to take the appropriate measures, i.e. not to see anyone outside of our household. Beyond the fact that this is obviously very costly on an individual and family level, and is not guaranteed to be completely effective, the story is not that simple.
This pace is all the greater as the number of infections grows higher, which gives the virus as many chances to mutate. How many times have we heard that this wave was the last one, only to discover almost at the same time that a new worrying variant with new characteristics was becoming dominant? Of course, there are vaccines, and that is wonderful. But this dynamic of the variants is problematic because one infection can be repeatedly followed by another, and the multiplication of episodes increases the probability of complications such as mutations which demonstrate some vaccine evasion and treatment resistance. The vaccine itself, while it reduces the risk of severe disease and death, does not fully protect against infection, transmission, or long Covid, and it must be renewed regularly with boosters to continue to provide adequate protection. And without near-universal global vaccination coupled with other mitigations to contain the spread of infections during the process, it is a race against time that promises to accelerate as more and more different variants with vaccine-evading potential appear over time.
When we decide to participate in this dynamic, it is reasonable to ask whether it can have a happy ending. Some think so, in the name of herd immunity, but as infection or vaccination against prior variants does not provide reliable, lasting immunity against emerging variants, it would only be a realistic promise if we could stop the emergence of variants. Can we really celebrate the reclaiming of individual freedoms until we are able to stop the virus, with the sword of Damocles hanging over our heads? This is an indecent freedom bought on on credit, poised to make its beneficiaries lose months or years of healthy life, and it is the freedom to compel others to lose it.
Finally, the exercise of freedom implies confronting, not evading, the questions of responsibility. Transmitting a virus which is likely to generate the long-lasting effects of Long Covid for hundreds of thousands of people, or even to be lethal for millions of people, is not trivial. To hide the moral imperative not to harm others in the name of a fight for freedom is problematic. Freedom and individual responsibility are intimately associated in liberal thought, as Friedrich Hayek’s writings attest. To dissociate them does not constitute a moral project for society that would bring together all those who love freedom. We classical liberals claim the effectiveness of voluntary measures, and fight, against imposed constraints, for responsibility. It is time to show responsibility in the area of Covid, by helping to reduce its spread while defending Freedom.
Европейская сеть ВОЗ «Здоровые города»
Основная цель действующего под эгидой ВОЗ глобального движения «Здоровые города» – всемерно содействовать тому, чтобы вопросы здоровья заняли приоритетное положение в социально-экономической и политической повестке дня органов городского самоуправления.
В течение 30 лет своего развития Европейская сеть ВОЗ «Здоровые города» объединила свыше 100 флагманских городов и около 30 национальных сетей.
Флагманские города взаимодействуют непосредственно с ЕРБ ВОЗ, а национальные сети объединяют города в пределах конкретного государства-члена. В обоих случаях ВОЗ предоставляет политическую, стратегическую и техническую поддержку, а также помогает в укреплении потенциала.
Флагманские города и национальные сети в совокупности охватывают около 1400 муниципалитетов.
Их общая цель – вовлечь местные органы власти в процессы укрепления политической приверженности, институциональных преобразований, наращивания потенциала, планирования на базе партнерств и внедрения инноваций.
Тридцатилетие сети «Здоровые города»
В 2018 г. Сеть в масштабе всего Европейского региона отмечает свое тридцатилетие: Саммит мэров ознаменовал старт юбилейных мероприятий, их кульминацией станет Международная конференция «Здоровые города», которая состоится в октябре в Белфасте.
В течение трех десятилетий движение «Здоровые города» служило инновационным стимулом преобразований в целях создания более здоровой городской среды, способствующей повышению уровня здоровья и благополучия жителей. Оно также стало вдохновляющим примером для сетей «Здоровые города» во всех остальных регионах ВОЗ, дав импульс для развития этого движения в глобальном масштабе.
Города играют важнейшую социальную, культурную и политическую роль, и поэтому Сеть будет праздновать свой 30-летний юбилей с прицелом на будущее.
В этом сложном мире, где существуют многочисленные уровни государственной власти, различные секторы, стремящиеся к достижению одних и тех же целей, а также множество сторон, заинтересованных в повышении показателей здоровья и благополучия, города располагают уникальными возможностями для выполнения функций лидерства.
Глобальные проблемы решаются на местном уровне. Это один из принципов концептуального видения «Здоровых городов».
Подход «Здоровые города»
Станьте членом Европейской сети ВОЗ «Здоровые города»
Принят на Саммите мэров городов-участников Европейской сети ВОЗ «Здоровые города», 12–13 февраля 2018 г., Копенгаген, Дания



Контакты ▼
Европейское региональное бюро ВОЗ
UN City
Marmorvej 51
DK-2100 Copenhagen Ø
Denmark
Тел.: +45 45 33 70 00
Факс: +45 45 33 70 01
Расположение и схема проезда
Направьте нам электронное сообщение
eLearning Courses
Our eLearning courses are designed to cover every step, process, and issue that needs to be understood in order to conduct high-quality research. Every course is written to be globally applicable, for all diseases and all regions. Each course is carefully researched to provide high-quality material that is peer reviewed and regularly updated. A certificate is issued once a minimum of 80% is achieved in the course quizzes.
NEW COURSES:
Tools for addressing public health emergencies in the context of civil society
Health Geography
RESEARCH PROCESSES & METHODS | SOCIAL SCIENCE, ETHICS & COMMUNITIES | INFECTION, IMMUNITY & RESISTANCE | WOMEN & CHILD HEALTH | LABORATORY, VECTORS & DIAGNOSITICS
Research Processes & Methods
Introduction to Clinical Research
1 module
An overview of the basic concepts of clinical research, focusing on the main areas of why and how clinical research is carried out, the importance of ethics in research, and an outline of the five main clinical study designs.
English | Español | Français | Português | Swahili | Việt | 中文
ICH Good Clinical Practice E6 (R2)
1 module
Good clinical practice provides a framework of principles which aim to ensure the safety of research participants and the integrity and validity of data. This course aims to provide the researcher with the basic principles of GCP and how these principles can be applied practically in the research setting. This ICH E6 GCP Investigator Site Training meets the Minimum Criteria for ICH GCP Investigator Site Personnel Training identified by TransCelerate BioPharma as necessary to enable mutual recognition of GCP training among trial sponsors.
English | Español | Français | Português | Русский | Việt
The Research Question
1 module
The research question forms the foundation of any study and is vital to the effectiveness and validity of the research to be carried out. This course explores the main factors that affect and influence the development of a valid research question.
English | Español | Français | Việt | 中文
The Study Protocol
2 modules
This course is designed to guide researchers through the basic stages and concepts surrounding the creation of a protocol, the document outlining the design of a study, describing the objectives, methodology and overall organisation of the research to be carried out forming a template and guide to the research process as a whole.
Part 1 | Première Partie
Part 2 | Deuxième Partie
Data Safety Monitoring Boards for Clinical Trials
1 module
This course examines the role of Data Safety and Monitoring Boards (DSMBs) in assessing the overall progress of a clinical trial and analysing the safety and efficacy data.
English | Français
Introduction to Informed Consent
1 module
The primary aims of informed consent are to protect the research participant from misinformation, exploitation and coercion. This course offers an introduction to the processes and wider factors which need to be taken into consideration when involving participants in clinical research.
Introduction to Data Management For Clinical Research Studies
1 module
Good data management is key to maintaining, processing. analysing and storing high-quality data. This overview is aimed at everyone involved in clinical research.
Introduction to Good Clinical Laboratory Practice
1 module
Good Clinical Laboratory Practice (GCLP) guidelines allow the reliability, quality, consistency and integrity of data generated by clinical trial laboratories to be assured. This course gives an overview of GCLP principles and their implementation ins a clinical trial laboratory.
English | Español | Français | Português
Good Clinical Laboratory Practice
7 modules
Good Clinical Laboratory Practice (GCLP) guidelines allow the reliability, quality, consistency and integrity of data generated by clinical trial laboratories to be assured. This course gives an overview of GCLP principles and their implementation ins a clinical trial laboratory.
English | Русский
How to Conduct GCP Inspections/Audits at the Clinical Investigator Site
1 module
Aimed at regulatory good clinical practice (GCP) inspectors and sponsor auditors who audit clinical trials, this course covers the procedures involved in planning, conducting and reporting inspections/audits, particularly at clinical investigator sites.
Data Sharing
9 modules
This course is aimed at early career researchers, postgraduate students and clinical research support staff who are collecting, managing and using health data.
Back to top
Social Science, Ethics & Communities
Introduction to Informed Consent
1 module
The primary aims of informed consent are to protect the research participant from misinformation, exploitation and coercion. This course offers an introduction to the processes and wider factors which need to be taken into consideration when involving participants in clinical research.
Essential Elements of Ethics
11 modules
Protocol authors should address certain ethical issues in the design of studies and document their rationale in a section of the protocol that will be easily understood by review boards and investigators. This eLearning resource will guide the development of a dedicated “Ethics section” of the protocol in which Essential Elements are addressed. This online resource will assist clinical researchers as they write their study protocol to recognize and address common ethical challenges in clinical trials, and ethics committee members as they review and analyse clinical trial protocols in an efficient and comprehensive manner.
Research in Global Health Emergencies: Ethical Issues
1 module
Emergencies are particularly challenging contexts in which to conduct health-related research – while research norms and standards remain important, applying these appropriately in exceptional circumstances needs careful and nuanced consideration. Based on a Nuffield Council on Bioethics report, this course explores core ethical issues that arise during research in global health emergencies, and highlights how they sometimes go beyond those covered in traditional research frameworks.
Ethics in Epidemics, Emergencies and Disasters: Research, Surveillance and Patient Care
7 modules
A comprehensive exploration of the wide range of ethical issues faced by health professionals and policy makers working in the context of epidemics/pandemics and disaster situations, focusing primarily on the key areas of research, surveillance and patient care.
Ethics Review of Social Research on Health-Related Topics
1 module
Increasingly biomedical ethics committees are being asked to review applications to conduct social research (SR) on health-related topics. As with medical research, SR can involve risks of harm as well as potential benefits that need to be assessed in an ethics review process. However, these risks and benefits can be different from those in medical research. Ethics review of SR should be sensitive to how ethical issues in social research depart from the so-called ‘medical model’ of review.
The Practice and Ethics of Participatory Visual Methods for Community Engagement in Public Health and Health Science
8 modules
This course provides guidelines on the practice and ethics of participatory visual methods (PVM) with emphasis on their use in low and middle-income countries for community and public engagement in health and health science. With a wealth of practical tips and case studies, this course has been developed for use by engagement practitioners who are relatively new to the field of PVM and want to learn more about what they are and how to work with them.
Children and Clinical Research
1 module
If children and young people are not given the opportunity of taking part in research, it is very difficult to obtain the evidence needed to improve the health services provided for them. This course aims to give researchers and members of ethics committees confidence in thinking through the challenges of carrying out research with children and young people.
English | Español
Ethics of Ancillary Care in Research
1 module
Ancillary care is healthcare that research participants need but that is not required by to answer the researchers’ scientific question or to avoid or mitigate harm resulting from participation in the research. This course covers the main ethical questions associated with providing or facilitating ancillary care, including the various philosophical approaches to establishing whether or not researchers have ancillary care obligations.
Ethics and Best Practices in Sharing Individual-level Research Data
1 module
Research funders, regulators and researchers are increasingly calling for the sharing of individual-level data from biomedical and public health research. This introductory course aims to describe the potential benefits and risks of sharing data, discusses the ethical challenges involved and proposed best practices insharing research data.
Introduction to Reviewing Genomic Research
1 module
This introductory course provides an overview of how genomic research differs from other research, and the specific ethical issues to consider when conducting an ethics review of this research.
English | Español | Français | Português
What is Open Science?
1 module
Open Science is a scientific activity practiced in an open, collaborative and transparent way in all knowledge domains, from fundamental science to social and human sciences. This course presents the concept of open science, as well as the reasons and advantages of practicing open science. This course is aimed at students, researchers and the general public.
English | Español | Português
Open Access
5 modules
Open Access refers to the practice of making research publications freely available to the public so that anyone can read and use them. It can also come in the form of reusing content shared by other researchers. This course aims to help you understand a little more about the main concepts, historic milestones, different forms of applications, and various initiatives both on the international scene and Brazilian experiences of Open Access. This course is aimed at students, researchers and the general public.
English | Español | Português
Tools for Scientific Dissemination
11 modules
This course is intended to help the reader plan and execute scientific advertising activities in different formats and by targeting different audiences. It is aimed at researchers and post-graduate students interested in scientific advertising.
English | Español | Português
Tools for addressing public health emergencies in the context of civil society
9 modules
This course aims to share technical and scientific knowledge about public health emergencies. It presents how global governance operates, ways of civil society action and tools to help social movements to act as mediators and producers of knowledge through the strengthening of popular surveillance and digital activism. It is intended for representatives of, and those involved with, social movements of vulnerable populations in Latin America. It may be extended to the public of other countries and people interested in the subject.
English | Español | Português
Health Geography
Health geography is a sub-discipline of human geography, which offers a holistic view on health by linking health and disease outcomes to the socio-cultural and physical environment, and the places that generate them. This course is aimed at health researchers needing to understand how to incorporate geographical thought into their work. In addition, geographers needing to apply their methods to health could find value in taking this introductory course.
Infection, Immunity & Resistance
Neurological Infectious Diseases
1 module for each disease
Neurological infectious diseases pose some of the greatest challenges to clinicians. The presenting clinical syndromes are often elusive, determining the causative organisms can be problematic, and there is often little evidence to guide treatment. Although many are rare, others are extremely common, particularly in tropical climates, and collectively the disease burden is considerable. These Neurological Infectious Diseases eLearning modules are aimed at medics of all grades, from undergraduate students to consultants and senior academics.
English | Español | Français | Português
Maternal Infections
6 modules
Appropriate prevention, diagnosis and treatment of infections during pregnancy can reduce maternal and neonatal morbidity and mortality, and mitigate the adverse effects on both mothers and newborns. For each major maternal infection, this course addresses the global burdens, the effects on mother and fetus, diagnosis and treatment based on current evidence.
Transmission, Surveillance, Control and Prevention of Yellow Fever
1 module
The course presents general concepts of yellow fever, aimed at health professionals who work in primary healthcare, including surveillence and treament measures.
English | Português
COVID-19: Management of Infection Caused by the Novel Coronavirus
2 modules
The course is one of the initiatives of the Oswaldo Cruz Foundation (Fiocruz, Brazil) which, in the face of the health emergency scenario, seeks to contribute to the strengthening of the health system in order to face this and other health challenges. The course is introductory in nature: it provides training for professionals working in health services for the clinical management of the disease.
English | Español | Português
Back to top
Women & Child Health
Children and Clinical Research
1 module
If children and young people are not given the opportunity of taking part in research, it is very difficult to obtain the evidence needed to improve the health services provided for them. This course aims to give researchers and members of ethics committees confidence in thinking through the challenges of carrying out research with children and young people.
English | Español
Maternal Infections
6 modules
Appropriate prevention, diagnosis and treatment of infections during pregnancy can reduce maternal and neonatal morbidity and mortality, and mitigate the adverse effects on both mothers and newborns. For each major maternal infection, this course addresses the global burdens, the effects on mother and fetus, diagnosis and treatment based on current evidence.
Obstetric Fistula
4 modules
Each year between 50,000 to 100,000 women worldwide are affected by obstetric fistula and it is estimated that more than 2 million young women live with untreated obstetric fistula in Asia and sub-Saharan Africa. This course addresses the epidemiology, etiology, pathogenesis, prevention, diagnosis, classification and management of obstetric fistula.
English | Français
INTERGROWTH-21st Course on Maternal, Fetal and Newborn Growth Monitoring
3 modules
This course communicates the methodology of maternal, fetal and newborn growth monitoring and the application of the INTERGROWTH-21st international growth standards to make judgement about appropriateness of growth.
English | Español | Italiano | Português
Preterm Infant Feeding and Growth Monitoring: Implementation of the INTERGROWTH-21st Protocol
3 modules
The INTERPRACTICE-21st Project promotes the optimal postnatal growth of preterm infants and standardises growth measurement in selected populations around the world. It is based on the implementation of the INTERGROWTH-21st international standards for preterm postnatal growth and evidence-based feeding recommendations based on human milk. This course provides a background on preterm birth, gastrointestinal development in preterm infants, and feeding recommendations for the routine care of preterm infants.
English | Español | Italiano | Português | Русский
COVID-19 in pregnancy, delivery and the neonatal period
1 module
COVID-19 is a global emergency. Its effects on pregnancy and the newborn include the direct spread of disease to pregnant women and their babies and indirectly, the reduction in access to essential maternal and newborn healthcare services resulting in maternal and newborn morbidity and mortality. The aim of the course is to provide healthcare providers with evidence-based recommendations for disease prevention and management of pregnant women and their babies during the COVID-19 pandemic and thereby lessen the adverse maternal and newborn outcomes from the disease.
English | Español
Speech therapy healthcare: oral sensory-motor disorders in the field of neonatology
8 modules
The physical, psychological, social, and financial burden of oral sensory-motor disorders in pre and full term infants strongly impacts the patients, their caregivers, and the healthcare system that supports them. In sharp contrast to these multifaceted and often long-term consequences, recognition of these disorders in the medical and political communities is strikingly poor and has not changed meaningfully over the past years. This course aims to heighten awareness and amend this collective neglect.
Back to top
Laboratory, Vectors & Diagnostics
Introduction to Good Clinical Laboratory Practice
1 module
Good Clinical Laboratory Practice (GCLP) guidelines allow the reliability, quality, consistency and integrity of data generated by clinical trial laboratories to be assured. This short course gives an overview of GCLP principles and their implementation ins a clinical trial laboratory.
English | Español | Français | Português
Good Clinical Laboratory Practice
7 modules
This course is for all those wanting to gain an in-depth understanding of Good Clinical Laboratory Practice and how each principle of GCLP can be applied in clinical trial laboratory.
Basic Malaria Microscopy
5 modules
The Basic Malaria Microscopy Learner’s Guide is a World Health Organisation (WHO) publication. The WHO have very kindly granted permission for the replication of the Guide in an e-learning format.
Back to top
These eLearning courses originate from resources that researchers have shared with us; many researchers teach face-to-face courses, and these can easily be converted into eLearning courses to disseminate the knowledge and skills taught on each course further. All source material, authors and reviewers are fully acknowledged. If you have any material which you feel would make a good eLearning course, or any resouces that you feel would benefit other researchers and which you are willing to share, please do not hesitate to contact us. We will continue to extend this list of courses so please tell us if you need to learn about something that you do not see listed here. Please also get in touch if you have any feedback on our courses: training@theglobalhealthnetwork.org
If you have any questions about our eLearning courses or how to use our site, then please see our FAQ section.
 Funding
Funding
The Global Health Training Centre is supported in part by a grant from the Bill & Melinda Gates Foundation.
Funding
The Global Health Training Centre is supported in part by a grant from the Bill & Melinda Gates Foundation.
Collaboration
We worked with the following organisations and institutions to produce these courses:
Digital health
Digital technologies are now integral to daily life, and the world’s population has never been more interconnected. Innovation, particularly in the digital sphere, is happening at unprecedented scale. Even so, its application to improve the health of populations remains largely untapped, and there is immense scope for use of digital health solutions.
WHO is harnessing the power of digital technologies and health innovation to accelerate global attainment of health and the well-being
WHO has three key objectives to promote the adoption and scale-up of digital health and innovation:
1. Translating latest data, research, and evidence into action: this means promoting standards for interoperability and data sharing and supporting implementation of digital solutions that contribute to informed decision making.
2. Enhancing knowledge through scientific communities of practice: enabled by new technologies and no longer limited by the need for physical meetings or hard copy peer review journals, WHO brings together top expert voices around topics of clinical and public health significance.
3. Systematically assessing and linking country needs with supply of innovations: all too often in global health, products are developed with the attitude of “if you build it, they will use it.” This approach has failed time and again. WHO takes a proactive, systematic approach to identify, promote, co-develop, and scale innovations that are based on country needs.
The WHO Global Strategy on Digital Health, adopted in 2020 by the World Health Assembly, presents a roadmap to link the latest developments in innovation and digital health, and put these tools to action in order to improve health outcomes.
Part of WHO’s strategic vision is for digital health to be supportive of equitable and universal access to quality health services. Digital health can help make health systems more efficient and sustainable, enabling them to deliver good quality, affordable and equitable care.
These high ideals are challenging to attain, especially for low- and middle-income countries. The purpose of WHO’s Global Strategy on Digital Health is to support countries in strengthening their health systems through the application of digital health technologies and achieve the vision of health for all. The strategy is designed to be fit for purpose and for use by all Member States, including those with limited access to digital technologies, goods and services.
Источники:
- http://www.worldhealthnetwork.global/
- http://www.worldhealthnetwork.global/omicron
- http://www.worldhealthnetwork.global/alerts
- http://www.worldhealthnetwork.global/action
- http://www.worldhealthnetwork.global/transmission
- http://www.worldhealthnetwork.global/school-guidelines
- http://www.worldhealthnetwork.global/monkeypoxdeclaration
- http://www.worldhealthnetwork.global/monkeypoxpressrelease
- http://www.worldhealthnetwork.global/members-publications
- http://tghn.org/
- http://translate.academic.ru/World%20Health%20Network/ru/en/
- http://translate.academic.ru/World%20Health%20Network/en/ru/
- http://www.worldhealthnetwork.global/summit-sessions
- http://gcp.network/ru/
- http://www.dehealth.world/
- http://www.worldhealthnetwork.global/visual-page
- http://www.globalindoorhealthnetwork.com/
- http://globalhealthtrainingcentre.tghn.org/
- http://apa.az/en/social/world-health-network-declares-monkeypox-a-pandemic-379255
- http://www.worldhealthnetwork.global/ihavecovid
- http://www.who.int/health-topics/infodemic
- http://universal_ru_en.academic.ru/282319/World_Health_Network
- http://www.worldhealthnetwork.global/norway
- http://www.worldhealthnetwork.global/projects-2
- http://www.worldhealthnetwork.global/emergency-summit
- http://www.who.int/news-room/questions-and-answers/item/radiation-5g-mobile-networks-and-health
- http://ourworldindata.org/health-meta
- http://markets.businessinsider.com/news/stocks/global-coalition-of-public-health-experts-and-citizens-announces-formation-of-world-health-network-with-goal-of-covid-19-elimination-1030915768
- http://www.worldhealthnetwork.global/yaneer-interview
- http://www.worldhealthnetwork.global/ventilation
- http://www.who.int/teams/health-workforce/health-professions-networks
- http://www.who.int/health-topics/health-workforce
- http://www.worldhealthnetwork.global/databank
- http://webhealthnetwork.com/
- http://www.worldhealthnetwork.global/isolationguidelines
- http://www.who.int/clinical-trials-registry-platform
- http://www.globalindoorhealthnetwork.com/statistics
- http://www.tadviser.ru/index.php/Network_Health_Monitoring_-_%D0%9C%D0%BE%D0%BD%D0%B8%D1%82%D0%BE%D1%80%D0%B8%D0%BD%D0%B3_%D1%81%D0%B5%D1%82%D0%B8_%D0%B8%D0%BB%D0%B8_%D1%83%D0%BF%D1%80%D0%B0%D0%B2%D0%BB%D0%B5%D0%BD%D0%B8%D0%B5_%D0%B7%D0%B4%D0%BE%D1%80%D0%BE%D0%B2%D1%8C%D0%B5%D0%BC-%D0%BF%D1%80%D0%BE%D0%B8%D0%B7%D0%B2%D0%BE%D0%B4%D0%B8%D1%82%D0%B5%D0%BB%D1%8C%D0%BD%D0%BE%D1%81%D1%82%D1%8C%D1%8E_%D0%98%D0%A2-%D0%98%D0%BD%D1%84%D1%80%D0%B0%D1%81%D1%82%D1%80%D1%83%D0%BA%D1%82%D1%83%D1%80%D1%8B
- http://www.thiswormyworld.org/news-blogs/blogs/introducing-the-global-health-network-a-knowledge-sharing-digital-platform
- http://github.com/WorldHealthOrganization
- http://gcp.network/
- http://apps.apple.com/us/app/who-info/id895463794
- http://www.apa.org/international/pi/2013/03/who
- http://www.worldlifeexpectancy.com/world-health-rankings
- http://www.who.int/teams/health-workforce/health-professions-networks/
- http://www.verywellhealth.com/world-health-organization-facts-4842833
- http://www.worldhealthnetwork.global/covidandfreedom
- http://www.euro.who.int/ru/health-topics/environment-and-health/urban-health/who-european-healthy-cities-network
- http://globalhealthtrainingcentre.tghn.org/elearning/
- http://www.who.int/health-topics/digital-health








































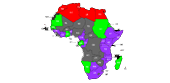
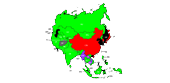
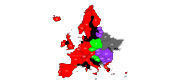
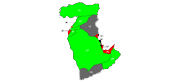

















:max_bytes(150000):strip_icc()/2020ElizabethHanesheadshot-ed9e11cd856543179f6b17238d7e66e6.jpg)
:max_bytes(150000):strip_icc()/James-Lacy-1000-7e812c960b8b463da418845e72b9b086.jpg)
:max_bytes(150000):strip_icc()/GettyImages-456610468-56b80a9d3df78c0b1364df8f.jpg)


 Funding
Funding