World health organization age classification
World health organization age classification
Everyone knows that the elderly – it is the young who are beginning to age. Then in the human body irreversible changes occur. However, graying hair, wrinkles and shortness of breath are not always talking about the onset of old age. But how to determine the age when a person can be attributed to the category of the elderly?
Different time-different opinions?
It was once thought that old age – when a person has exceeded 20. We remember a lot of vivid historical examples where young people were married after reaching the age of 12-13 years. By the standards of the middle ages woman in 20 years was considered old. Today, however, not the middle ages. A lot has changed.
Later, this figure had been changed several times and the young were considered to be twenty people. This age marks the beginning of independent life, so flourishing, youth.
Modern views on age
In modern society again, everything somehow changed. And today, most young people did not hesitate to rank as the elderly those who barely crossed the thirties. The proof is the fact that employers are quite wary of applicants older than 35. And what can we say about those who have crossed 40?
But, it would seem that by this age, a person acquires a certain confidence, life experience, including professional. At this age he has a solid stance, clear goals. This is the age when people are able to realistically assess their strengths and take responsibility for their own actions. And suddenly, the verdict is: “Older”. What age can be considered individual elderly, we will try to understand.
How relevant today, drugs against worms in humans? What kind of creatures these worms, what are modern methods of treatment? We will try to answer these questions, since ignorance in this area is undesirable. Imagine a mummy, which is misleading in k.
Male impotence is a pathological condition associated with abnormal physiological capacity of the penis to reginout and bring sexual partner pleasure in bed.sex impotenceimpotence may not men to pass unnoticed – it usually spoils his nervous sy.
Developmental milestones
Representatives of the Russian Academy of medical Sciences say that recently there have been significant changes in the determination of biological age of a person. To explore these and many other changes occurring with the person, there is world health organization-who. Thus, the classification of the age of the person who says the following:
All who were fortunate enough to cross this threshold are considered to be long-lived. Unfortunately, up to 90, and especially 100 to live a few. The reason for this are various diseases that afflict people, the environmental situation and living conditions.
So what is it? Older age according to the who classification is much younger?
What is shown in polls
According to opinion polls, held annually in different countries, the people themselves are not going to grow old. And ready to identify themselves to the elderly only when they reach the age of 60-65 years. Apparently here originate bills to increase the retirement age.
Older people, however, need to devote more time to their health. In addition, the reduced attention and speed of information perception is not always possible for people 60 years to adapt quickly to changing situations. Of particular relevance it assumes in the conditions of scientific-technical progress. People who have reached a certain age it is sometimes difficult to master innovative technologies. But few think about the fact that for many people this is the strongest psychological trauma. They suddenly begin to feel their worthlessness, uselessness. This exacerbates the already heightened situation of reassessment of the age.
My years-my wealth
Classification of age who is not an absolute criterion to assign the person to a specific age category. It is not only the number of years characterizes the human condition. It is appropriate to recall the famous saying that says that a man is as old as he feels. Perhaps this expression to a greater extent characterizes the age of the person than the age classification of the who. It is related to the emotional condition of the person and with the degree of deterioration of the organism.
Unfortunately, the disease plaguing and harassing people, do not ask age. They are affected equally and the elderly, and children. It depends on many factors, including the condition of the body, immunity and living conditions. And, of course, from the way the person relates to their health. When something is not fully cured of the disease, and lack of proper rest, poor nutrition-all this and more pretty much makes the body.
Old age – for many grunts, poor memory, a whole bunch of chronic diseases. However, all of these weaknesses can be characterized and relatively young man. Today, it is not a criterion in order to classify the person to a specific age category.
The Crisis of middle age. What it the threshold?
Everyone knows such a thing as a midlife crisis. And who can answer the question, at what age it occurs more frequently? Before to define this age, let’s deal with the concept.
Under the crisis here refers to a time when a person begins to rethink values, beliefs, evaluate your life and your actions. It’s probably a phase in life and occurs when the experience of human life, experience, mistakes and frustration. Therefore, this life stage is often accompanied by emotional instability, even a deep and prolonged depression.
The Onset of such a crisis inevitable, it can last from several months to several years. And its duration depends not only from individual to individual and from his past life and from the profession, family environments and other factors. A emerge victorious from this conflict of life. And then the middle age gives way to aging. But it can also happen that the contractions go older and lost interest in life people who haven’t reached 50.
That says world health organization
As we have considered above, older age according to the who classification falls within the range from 60 to 75 years. According to the results of sociological researches, the representatives of this age category are young at heart and not going to burn themselves in the elderly. By the way, according to the same research conducted ten years ago, to the old carried all under the age of 50 years or more. The current classification of age by the who shows that people middle age. And it is quite possible that this category will only younger.
Few people in her youth think about what is the age considered elderly. And, crossing one milestone after another, people understand that at any age «life begins”. Only after accumulating a huge experience, people begin to think about how to prolong youth. Sometimes it turns into a real fight with age.
Signs of aging
The Elderly in the who is characterized by the fact that people have a reduction in vitality. What does it mean? Older people become sedentary, gain weight chronic diseases, they suffer from a reduced attentiveness, memory worsens.
However, older age according to the who classification, it is not just the age range. Researchers long ago came to the conclusion that the aging process takes place in two areas: physiological and psychological.
Senescence
With regard to physiological aging, it is the most clear and visible to others. As with the human body there are certain irreversible changes which are noticeable to himself and others. In the body everything changes. The skin becomes dry and loose, it causes wrinkles. The bones become brittle and because of this, the probability of fracture increases. Hair are discolored, broken and often falls. Of course, for people who want to keep their youth, many of these problems are solvable. There are various cosmetic products and procedures which, if correct and regular use can disguise visible changes. But these changes sooner or later will become visible.
Psychological aging
Psychological aging might not be as noticeable to others, but it is not always so. The elderly often varies greatly in nature. They become inattentive, irritable, tired quickly. And it happens often precisely because they see the manifestation of physiological aging. They not in forces to affect irreversible processes in the body and because of this, often experience deep emotional drama.
So what is the age considered elderly?
Due To the fact that every human body has its own characteristics, such changes occur in all different ways. And comes physiological.
Article in other languages:
later this figure several times changed and young people were considered to be twenty years.It is this age symbolizes the beginning of an independent life, and thus blossoming youth.
Modern views on the age
In modern society, again somehow changed.Today, most of the young people did not hesitate to classify the elderly who barely stepped over thirty years abroad.Proof of this is the fact that employers are quite wary of job seekers older than 35. And what can we say about those who have crossed 40?
But, it would seem, at this age the person gets some confidence, experience, including professional.At this age, he has a solid stance, clear goals.This is the age when a person is able to realistically assess their strength and take responsibility for their own actions.And suddenly, the verdict is: «The elderly».At what age can count the individual seniors, and we try to understand.
age limit
all who were fortunate enough to cross this threshold are considered to be long-lived.Unfortunately, up to 90, and even more so few live to 100.The reason for this are the different diseases that affect people, the environmental situation and living conditions.
So what happens?With old age according to WHO classification is much younger?
What sociological studies show
According to opinion polls, held annually in different countries, the people themselves are not going to grow old.And willing to classify themselves to the elderly only when they reach the age of 60-65 years.Apparently here originate a bill to increase the retirement age.
Older people, however, need to devote more time to their health.In addition, decreased attention and speed of information perception is not always possible for people over 60 years to adapt quickly to the changing situation.Of particular relevance is assumed in the scientific and technical progress.People who have reached a certain age, it is sometimes difficult to develop innovative technologies.But few people think about the fact that for many people this is a strong psychological trauma.They suddenly begin to feel worthlessness, uselessness.This exacerbates the deterioration of the situation revaluation of age.
age WHO classification is not an absolute criterion for chargeability person to a certain age group.It is not only the number of years characterizes the human condition.It is appropriate to recall the famous proverb that says that a man as old as he feels himself.Perhaps this expression to a greater extent characterizes a person’s age rather than age WHO classification.This is due not only to the psycho-emotional state of the person and to the degree of deterioration of the body.
midlife crisis.What is it today, the threshold?
Everybody knows such a thing as a midlife crisis.And who can answer the question about the age at which it occurs most often?Before you define this age, let’s get with the concept.
Under the crisis is here meant such a moment, when a person begins to rethink the values, beliefs, estimates the lived life and his actions.Probably, such a period in my life and there comes a time when a man behind those years, experience, mistakes and disappointments.Therefore, the life span is often accompanied by emotional instability, even a deep and prolonged depression.
onset of such a crisis is inevitable, it can last from several months to several years.And its duration depends not only from individual to individual and from his past life, but also by profession, family situation and other factors.Many emerging victorious from the conflicts of this life.And while the average age of not giving way to aging.But it happens, and so that out of this battle aged and lost interest in the life of people who have not yet reached 50 years.
What does the World Health Organization
As we have already discussed above, the older age of the WHO classification falls in the range of 60 to 75 years.According to the results of sociological research, the representatives of this age group and the young at heart is not going to write itself in the elderly.By the way, according to the same study, conducted ten years ago, all attributed to the elderly and those with 50 years or more.The current classification of the age of the WHO shows that this middle-aged people.And it is not excluded that this category will only younger.
Few youth thinks about what age is considered elderly.It was only over the years, crossing one milestone after another, people realize that at any age, «life is just beginning.»Only accumulated great experience, people start to think about how to stay young.Sometimes it turns into a real fight with age.
signs of aging
Old age is characterized by the WHO, that people have a decrease in vitality.What does this mean?Older people become sedentary, gain a lot of chronic diseases have decreased attentiveness, memory deteriorates.
However, old age according to WHO classification, it is not just age limits.Researchers have long come to the conclusion that the aging process is happening as if in two directions: physiological and psychological.
senescence
Regarding the physiological aging, then it is most clear and noticeable to others.As with the human body there are certain irreversible changes that are noticeable to himself and others.The body is changing everything.The skin becomes dry and loose, it leads to the fact that there are wrinkles.Bones become brittle and because this increases the probability of fracture.Hair discolored, broken and often drop out.Of course, for people who are trying to preserve their youth, many of these problems are solvable.There are various cosmetic products and procedures with proper and regular use can mask the visible changes.But these changes will sooner or later become apparent.
Psychological aging
Psychological aging might not be noticeable to others, but it happens not always.Older people often vary greatly in nature.They become inattentive, irritable, quickly get tired.And it happens often it is because they see the manifestation of physiological aging.They can not affect the irreversible processes in the body and because of this often experience a deep emotional drama.
So what age is considered elderly?
Due to the fact that the body of each person is different, there are similar changes in all different ways.And there comes a physiological and psychological aging is not always at the same time.Strong-willed people, optimists can take your age and maintain an active lifestyle, thereby slowing down physiological aging.So to answer the question of what age is considered elderly, it is sometimes quite difficult.It is not always the number of past years is indicative of the state of man’s inner world.
Most people who look after their health, feel the first changes in your body and try to adapt to them, they reduce the negative manifestation.If you regularly deal with his health, then possibly move the approach of old age.Therefore, those who fall into the category of «old age» according to WHO classification, can not always feel that way.Or, on the contrary, those who have overcome the 65-year milestone, consider themselves very old man.
Therefore, it is useful to recall once more that the proverb says: «A man as old as he feels.»
The elderly age according to the WHO classification is how much? What age is elderly?
Everyone knows that the elderly is someone who is no longeryoung, who begins to grow old. Then in the human body there are irreversible changes. However, graying hair, wrinkles and shortness of breath do not always indicate the onset of old age. But how to determine the very age when a person can be ranked as an elderly person?
It used to be that older age iswhen the person has passed for 20. We remember a lot of vivid historical examples, when young people entered into marriage, having barely reached the age of 12-13 years. By the standards of the Middle Ages, a woman at the age of 20 was considered an old woman. However, today is not the Middle Ages. Much has changed.
Later this figure changed several times and young people began to be considered twenty years old. It is this age that symbolizes the beginning of an independent life, which means prosperity, youth.
Modern views on age
In a modern society again all somehowchanges. And today, most of the young people, without hesitation, will rank among the elderly those who have barely crossed the thirty-year boundary. Proof of this is the fact that employers are also wary of job seekers over 35. And what about those who stepped over 40?
But in fact, it would seem, to this age manacquires some kind of self-confidence, life experience, including professional. At this age, he has a firm life position, clear goals. This is the age when a person is able to really assess their strengths and be responsible for their own actions. And suddenly, as the verdict sounds: «Elderly.» At what age can the individual be considered elderly, we will try to understand.
Age boundaries
All who were fortunate enough to cross this bar,are considered long-livers. Unfortunately, up to 90, and even more so to 100 few live. The reason for this is the various diseases to which a person is exposed, the ecological situation, as well as the living conditions.
So what happens? What is the elderly age according to the WHO classification significantly younger?
What sociological research shows
According to sociological surveys, annuallyconducted in different countries, the people themselves are not going to grow old. And they are ready to consider themselves elderly only when they reach the age of 60-65 years. Apparently the bills on increasing the retirement age come from here.
Elderly people, however, need more timegive their health. In addition, the decline in attention and speed of information perception does not always allow people after 60 years to quickly adapt to the changing situation. This is especially important in the conditions of scientific and technological progress. People who have reached a certain age sometimes find it difficult to master innovative technologies. But few people think about the fact that for many people this is the strongest psychological trauma. They suddenly begin to feel worthless, unnecessary. This aggravates the already aggravated situation of revaluation of age.
My years are my wealth
Classification of age by WHO is notan absolute criterion for assigning a person to a certain age category. After all, not only the number of years characterizes a person’s condition. Here it is appropriate to recall a famous proverb that says that a person is as old as he feels himself. Probably, this expression is more indicative of a person’s age than the age classification of WHO. This is due not only to the psychoemotional state of a person and to the degree of deterioration of the body.
Elderly age is for many grumbling, badmemory, a whole bunch of chronic diseases. However, all the above disadvantages can also characterize a relatively young person. Today, this is far from being a criterion for placing a person in a certain age category.
Middle age crisis. What’s his threshold today?
Everyone is well aware of the notion of crisismiddle-aged. And who can answer the question about the age at which he often comes? Before you determine this age, let’s deal with the very notion.
Under the crisis here is understood such a time whena person begins to rethink values, beliefs, assess life lived and his actions. Probably, such a period in life also comes exactly when people have lived behind their years, experience, mistakes and disappointments. Therefore, this life period is often accompanied by emotional instability, even profound and prolonged depression.
The onset of such a crisis is inevitable, lastinghe can from several months to several years. And its duration depends not only on the individual characteristics of the person and on his lived life, but also on the profession, the situation in the family and other factors. Many come out victorious from this life collision. And then the average age does not give way to aging. But it also happens that out of this struggle come out aged and lost interest in life people who have not reached even 50 years.
What the World Health Organization says
As we have seen above,WHO classification falls within the range of 60 to 75 years. According to the results of sociological research, representatives of this age group are young at heart and are not going to write themselves down into old people. By the way, according to the same research carried out a dozen years ago, everyone who reached the age of 50 or more referred to the elderly. The current age classification by WHO shows that these are middle-aged people. And it is completely possible that this category will only be young.
Few in youth think about whatage is considered elderly. And only with the years, crossing one line after another, people understand that at any age «life is just beginning.» Only having accumulated a huge life experience, people start to think about how to prolong youth. Sometimes it turns into a real fight with age.
Signs of aging
The elderly age in WHO is characterized by the fact thatpeople are reduced life activity. What does this mean? Elderly people become inactive, acquire a lot of chronic diseases, they decrease care, memory worsens.
However, the old age according to the WHO classification, thisnot just the age range. Researchers have long come to the conclusion that the aging process takes place in two directions: physiological and psychological.
Physiological aging
As for physiological aging, itmost understandable and visible to others. Because with the human body there are certain irreversible changes that are visible to him, as well as others. Everything changes in the body. The skin becomes dry and flabby, this leads to the appearance of wrinkles. Bones become brittle and because of this the probability of fractures increases. Hair is discolored, broken and often falling out. Of course, for people trying to keep their youth, many of these problems are solvable. There are various cosmetic preparations and procedures that, if properly and regularly used, can mask visible changes. But these changes will sooner or later become noticeable.
Psychological aging
Psychological aging may not be sovisible to others, but this is not always the case. The elderly often change their character. They become inconsiderate, irritable, quickly get tired. And this happens often precisely because they observe the manifestation of the aging of the physiological. They are unable to influence the irreversible processes in the body and because of this often experience a deep emotional drama.
So what age is elderly?
Due to the fact that the body of each person hastheir characteristics, there are similar changes in all in different ways. And physiological and psychological aging is not always simultaneous. Strong in spirit people, optimists are able to take their age and maintain an active lifestyle, thereby slowing down the physiological aging. Therefore, it is sometimes difficult to answer the question of what age is considered elderly. After all, not always the number of years lived is an indicator of the state of the inner world of man.
Often people who are monitoring their health,feel the first changes in their body and try to adapt to them, reduce their negative manifestation. If you regularly take care of your health, then you can move away the approach of old age. Therefore, those people who fall into the category of «old age» according to WHO classification, can not always feel that way. Or, on the contrary, those who overcome the 65-year boundary, consider themselves ancient old men.
Therefore, it will be superfluous to recall once again what folk wisdom says: «A person is so old for how long he feels himself».
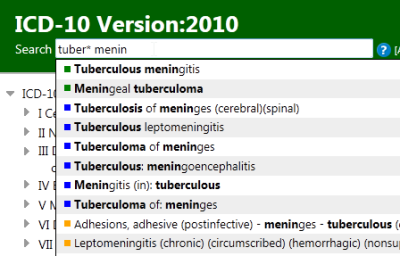
International Statistical Classification of Diseases and Related Health Problems (ICD)
ICD serves a broad range of uses globally and provides critical knowledge on the extent, causes and consequences of human disease and death worldwide via data that is reported and coded with the ICD. Clinical terms coded with ICD are the main basis for health recording and statistics on disease in primary, secondary and tertiary care, as well as on cause of death certificates. These data and statistics support payment systems, service planning, administration of quality and safety, and health services research. Diagnostic guidance linked to categories of ICD also standardizes data collection and enables large scale research.
For more than a century, the International Classification of Diseases (ICD) has been the basis for comparable statistics on causes of mortality and morbidity between places and over time. Originating in the 19 th century, the latest version of the ICD, ICD-11, was adopted by the 72 nd World Health Assembly in 2019 and came into effect on 1 st January 2022.
ICD purpose and uses
As a classification and terminology ICD-11:
ICD-11 Highlights
ICD-11 use cases
Uses of the ICD are diverse and widespread and much of what is known about the extent, causes and consequences of human disease worldwide relies on use of data classified according to ICD. See below just a few examples:
Classifications and Terminologies
WHO Family of International Classifications (FIC)
The WHO Family of International Classifications and Terminologies includes:
These Reference Classifications serve as the global standards for health data, clinical documentation and statistical aggregation.
Benefits of WHO-FIC
ICD-11, ICF and ICHI are key for effective knowledge representation and data transfer.
WHO Family of International Classifications (WHO-FIC) allows all healthcare workers (and patients) to communicate using one (technical) language.
In a hyper-connected world, WHO-FIC with their shared terminology are key for supporting natural language processing (NLP).
WHO-FIC with their shared terminology are key for effective text mining or text analytics (the process of deriving high-quality information from plain and unstructured text).
Used by
Reference Classifications
International Statistical Classification of Diseases and related health problems:
Diagnoses, injuries, findings, primary care.
The Foundation Component represents the entire WHO-FIC universe. It is a multidimensional collection of interconnected entities and synonyms. These entities consist of diseases, disorders, injuries, external causes, signs and symptoms, functional descriptions, interventions, and extension codes. ICD-11 statistical core (MMS) is derived from this foundation, ICF and ICHI will follow. Currently, with over hundred thousand entities and the ontological design of the foundation component, more than one million terms can be captured.
The Foundation Component also includes WHO terminologies such as:
Derived classifications are extensions of reference classifications, and are created for use within a specialty setting and are derived from the common foundation.
Related classifications
Related classifications are complementary to reference and derived classifications, and cover specialty areas not otherwise described in the Family of International Classifications (FIC).
WHO’s new International Classification of Diseases (ICD-11) comes into effect
World Health Organization Age Classification
Age Standardization Of Rates: A New WHO Standard
Age 48 People Used
Classifications World Health Organization
World 42 People Used
and the International Classification of Health Interventions (ICHI). These Reference Classifications serve as the global standards for health data, clinical documentation and statistical aggregation. WHO-FIC Maintenance Platform. Benefits of WHO-FIC. ICD-11, ICF and ICHI are key for effective knowledge representation and data transfer. WHO Family of …
Who Age Group Classification 2021 Erinbethea.com
Who 49 People Used
Appropriate classifications of the age group for risk stratification are 0–14 years old (pediatric group), 15–47 years old (young group), 48–63 years old (middle age group) and ≥ 64 years old (elderly group).. What are the medical age groups? Personal health care (PHC) spending by type of good or service and by source of funding (private health insurance, Medicare, Medicaid, out …
What Is The WHO Standard Age Group Classification? Study.com
What 61 People Used
The WHO standard age group classification is a set of standardized definitions which places people into certain categories based on their age. Under See full answer below. Become a …
65 Years Old Is Still Young! Brilio
Years 36 People Used
PROVISIONAL GUIDELINES ON STANDARD INTERNATIONAL AGE
STANDARD 53 People Used
Classifications in the different subject areas consist of between 18 and 54 age groups, counting single years as separate age groups and excluding the classification of population by size and
Is Anyone Aware Of Acceptable Age Classification
Anyone 49 People Used
Old Age According To The Who Classification Is How Much
Old 57 People Used
That says world health organization As we have considered above, older age according to the who classification falls within the range from 60 to 75 years. According to the results of sociological researches, the representatives of this age category are young at heart and not going to burn themselves in the elderly.
World (WHO 20002025) Standard Standard Populations
Standard 52 People Used
The World (WHO 2000-2025) Standards database is provided for 18 and 19 age groups, as well as single ages. To derive the single ages from the 5-year age group proportions, we used the Beers «Ordinary» Formula. For more information on why we use single ages, refer to 2000 U.S. Standard Population vs. Standard Million.
Aging Fits Disease Criteria Used By World Health Organization
Aging 61 People Used
Aging meets World Health Organisation (WHO) criteria used for classifying conditions as diseases, according to a team of scientists from the International Longevity Alliance, the Biogerontology Research Foundation, and the Department of Risk Factor Prevention.
Table 1, World Health Organization (WHO) Classification Of
Table 59 People Used
Table 1 World Health Organization (WHO) classification of nutritional status of infants and children. Nutritional status: Age: birth to 5 years Indicator and cut-off value compared to the median of the WHO child growth standards a: Obese: Weight-for-length/height b or BMI-for-age >3 standard deviations (SD) of the median: Overweight: Weight-for-length/height b or BMI-for …
Ageing World Health Organization
Ageing 33 People Used
Ageing and Health in the Western Pacific. The Western Pacific Region has one of the largest and fastest growing older population in the world. There are over 700 million people aged 65 and over in the world and more than 240 million of them reside in the Western Pacific Region. This number is expected to double by 2050.
World Health Organization Age Classification
Age Standardization of Rates: A new WHO Standard
2 hours ago world population age-structure was constructed for the period 2000-2025. The use of an average world population, as well as a time series of observations, removes the effects of historical events such as wars and famine on population age composition. The terminal age group in the new WHO standard population has been extended out to 100 years and
World Health Organization Age Group Classification 2021
7 hours ago That says world health organization. As we have considered above, older age according to the who classification falls within the range from 60 to 75 years. According to the results of sociological researches, the representatives of this age category are young at heart and not going to burn themselves in the elderly. More › 491 People Used
7 hours ago Appropriate classifications of the age group for risk stratification are 0–14 years old (pediatric group), 15–47 years old (young group), 48–63 years old (middle age group) and ≥ 64 years old (elderly group).. What are the medical age groups? Personal health care (PHC) spending by type of good or service and by source of funding (private health insurance, Medicare, Medicaid, out …
World Health Organization Age Classification 2020
8 hours ago In 2016, the world health organization drafted a global health sector strategy on hiv. Isbn 978 92 4 156504 2 (nlm classification: By 2020, the number of people aged 60 years and older will outnumber children younger than 5 years. To make achievements towards these targets, the draft lists actions that countries and the who can take.
5 hours ago Benefits of WHO-FIC. ICD-11, ICF and ICHI are key for effective knowledge representation and data transfer.. WHO Family of International Classifications (WHO-FIC) allows all healthcare workers (and patients) to communicate using one (technical) language. In a hyper-connected world, WHO-FIC with their shared terminology are key for supporting natural language …
8 hours ago That says world health organization As we have considered above, older age according to the who classification falls within the range from 60 to 75 years. According to the results of sociological researches, the representatives of this age category are young at heart and not going to burn themselves in the elderly.
World health organization age group classification 2021
Just Now World Health Organisation (WHO) AGE Platform Isbn 978 92 4 156504 2 (nlm classification: By 2020, the number of people aged 60 years and older will outnumber children younger than 5 years. The terminal age group in the new WHO standard population has been extended out to 100 years and In 2016, the world health organization drafted a global
World Health Organization Age Classification 2020
6 hours ago World health organization age classification 2020. (iii) culture and leisure complex center for new class of elders; The who standard age group classification is a set of. However the health organization had done a new research recently, according to average health quality and life expectancy, and defined a new criterion that divides human age
Is anyone aware of acceptable age classification
Just Now The World Health Organization (WHO) and the United Nations defines ‘Adolescents’ as individuals in the 10-19 years age group and ‘Youth’ as the 15-24 year age group. While ‘Young People’ covers the age range 10-24 years. As children up to the age of 18, most adolescents are protected under the Convention on the Rights of the Child.
8 hours ago Table 1. World Health Organization (WHO) classification of nutritional status of infants and children Nutritional status Age: birth to 5 years Indicator and cut-off value compared to the median of the WHO child growth standardsa Obese Weight-for-length/heightb or BMI-for-age >3 standard deviations (SD) of the median
PROVISIONAL GUIDELINES ON STANDARD INTERNATIONAL …
3 hours ago Classifications in the different subject areas consist of between 18 and 54 age groups, counting single years as separate age groups and excluding the classification of population by size and
Just Now Events. All →. WHO Global Health Facilities Database (GHFD) launch as part of this year’s UN Statistical Commission. 10 March 2022 15:00 – 16:30 CET. Country progress and way forward in phasing down the use of dental amalgam. 11 March 2022 15:30 – 16:30 CET. Sixty-sixth session of the Commission on the Status of Women (CSW 66) 14 – 25
United Nations has not classified 18 to 65-year-olds as
1 hours ago Social media posts in South Korea claim the United Nations (UN) has reclassified 18 to 65-year-olds as “youth”. The claim is false: representatives from various UN agencies said there was no such system, and UN publications define “youth” as …
World Health Organization Reference Curves
Author(s):
 | Mercedes de Onis |
| Dr Mercedes de Onis is the Coordinator of the Growth Assessment and Surveillance Unit of the Department of Nutrition at WHO in Geneva. | |
| View Author’s Full Biography |
Introduction
Childhood overweight and obesity are major public health problems worldwide (1,2). Traditionally, a heavy child meant a healthy child, and the concept “bigger is better” was widely accepted. Today, this perception has drastically changed based on evidence that overweight and obesity in childhood are associated with a wide range of serious health complications and increased risk of premature illness and death later in life (2,3).
Anthropometric references play a central role in identifying children that are overweight or obese, or at risk of becoming so. The assessment of growth based on the appropriate use and interpretation of anthropometric indices is the most widely accepted technique to identify growth problems in individual children and assess the nutritional status of groups of children (4). The correct interpretation of accurate and reliable anthropometric measurements to assess risk, classify children according to variable degrees of overweight and obesity, or evaluate child growth trajectories, is heavily dependent on the use of appropriate growth curves to compare and interpret anthropometric values (5-10).
This chapter presents the growth charts the World Health Organization (WHO) developed for preschool age children (WHO Child Growth Standards) and school-aged children and adolescents (WHO Growth Reference for School-aged Children and Adolescents); it also discusses issues related to their appropriate use for identifying overweight and obese children.
WHO child growth standards (0-60 months)
In April 2006 the World Health Organization released new standards for assessing the growth and development of children from birth to five years of age (11,12). The new standards were developed to replace the National Center for Health Statistics (NCHS)/WHO international growth reference (13), whose limitations have been described in detail elsewhere (4,14).
The origin of the Child Growth Standards dates from the early 1990s when WHO conducted a comprehensive review of anthropometric references. The review showed that the growth pattern of healthy breastfed infants deviated significantly from the NCHS/WHO international reference (15,16). In particular, the reference was inadequate for assessing the growth pattern of healthy breastfed infants (17). An expert group recommended the development of new standards, adopting a novel approach that would describe how children should grow when free of disease and receiving care that followed healthy practices such as breastfeeding and non-smoking (18). This approach would permit the development of a normative standard as opposed to a reference that merely described how children grew in a particular place and time. Although standards and references both serve as a basis for comparison, each enables a different interpretation. Since a standard defines how children should grow, deviations from the pattern it describes are evidence of abnormal growth. A reference, on the other hand, does not provide as sound a basis for making such value judgments, although in practice references often are mistakenly used as standards.
Following the World Health Assembly’s endorsement of these recommendations in 1994, the WHO Multicentre Growth Reference Study (MGRS) (19) was launched in 1997 to collect primary growth data that would allow the construction of new growth charts consistent with best health practices.
The MGRS, whose goal was to describe the growth of healthy children, was a population-based study conducted in six countries from diverse geographical regions: Brazil, Ghana, India, Norway, Oman, and the USA (19). The study combined a longitudinal follow-up from birth to 24 months with a cross-sectional component of children aged 18–71 months. In the longitudinal component, mothers and newborns were enrolled at birth and visited at home a total of 21 times at weeks 1, 2, 4 and 6; monthly from 2–12 months; and bimonthly in the second year (19).
The study populations lived in socioeconomic conditions favourable to growth. The individual inclusion criteria were: no known health or environmental constraints to growth, mothers willing to follow MGRS feeding recommendations (i.e. exclusive or predominant breastfeeding for at least 4 months, introduction of complementary foods by 6 months of age, and continued breastfeeding to at least 12 months of age), no maternal smoking before and after delivery, single term birth, and absence of significant morbidity. Rigorously standardized methods of data collection and procedures for data management across sites yielded high-quality data (11,12).
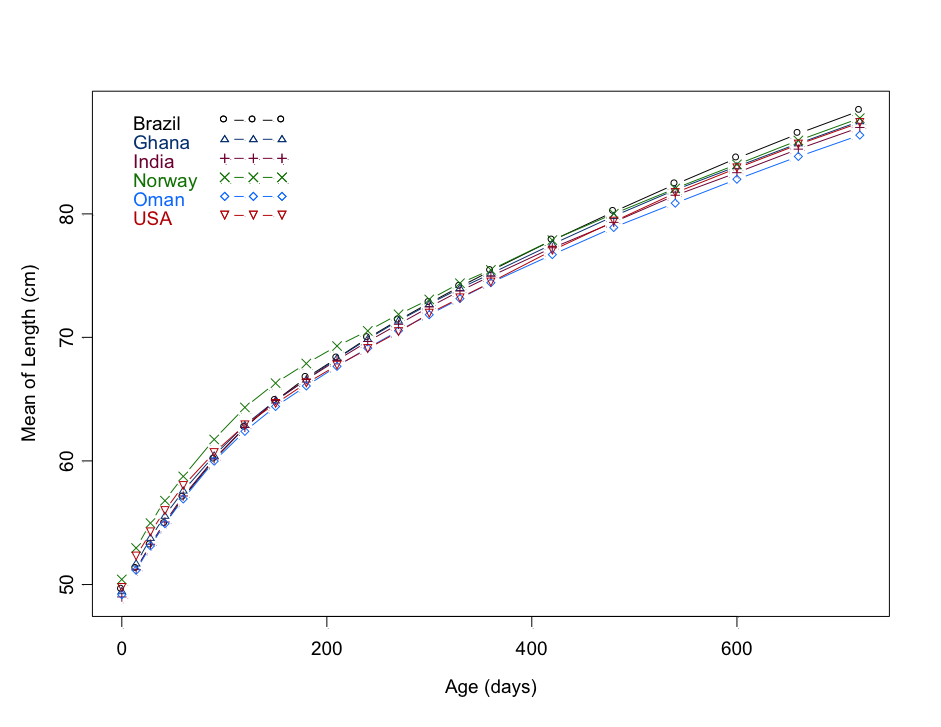
The length of children was strikingly similar among the six sites (Figure 1), with only about 3% of variability in length being due to inter-site differences compared to 70% for individuals within sites (20). The similarity in growth during early childhood across human populations means either a recent common origin as some suggest (21) or a strong selective advantage associated with the current pattern of growth and development across human environments. Data from all sites were pooled to construct the standards, following state-of-the-art statistical methodologies (11,22).
Figure 1. Mean length (cm) from birth to two years for the six WHO Multicentre Growth Reference Study sites
Weight-for-age, length/height-for-age, weight-for-length/height, and body mass index (BMI)-for-age percentile and z-score values were generated for boys and girls aged 0-60 months (11). Standards for head circumference, mid-upper arm circumference, and triceps and subscapular skinfolds were released in 2007 (23); and growth velocity standards for weight, length, and head circumference were issued in 2009 (24). Figure 2 presents a generic growth chart for body mass index-for-age in percentile values for girls aged 0–60 months. The full set of tables and charts is available at the growth standards website (www.who.int/childgrowth/en) together with tools like software, macros, and training materials that facilitate application. The disjunction observed at 24 months in the length/height-based charts represents the change from measuring recumbent length (i.e., lying down) to standing height in children below and above 2 years of age, respectively.
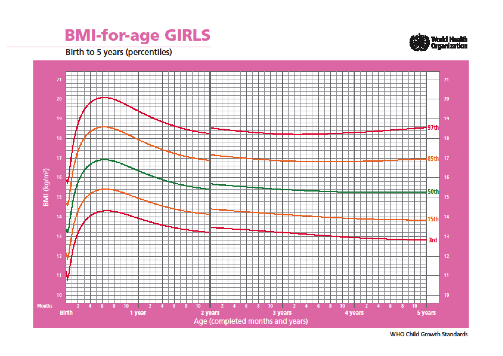
Figure 2. Body mass index-for-age in percentile values for girls aged 0 to 60 months
Detailed evaluation of the WHO standards as part of their introduction has provided an opportunity to assess their impact on child health programmes. Since their release in 2006, the standards have been widely implemented globally, with over 130 countries thus far having adopted them (25). Reasons for adoption include: 1) providing a more reliable tool for assessing growth that is consistent with the Global Strategy for Infant and Young Child Feeding; 2) protecting and promoting breastfeeding; 3) enabling monitoring of malnutrition’s double burden, stunting and overweight; 4) promoting healthy growth and protecting the right of children to reach their full genetic potential; and 5) harmonizing national growth assessment systems. In adopting the WHO growth standards, countries have harmonized best practices in child growth assessment and established the breastfed infant as the norm against which to assess compliance with the right of children to achieve their full genetic growth potential.
The WHO standards provide an improved tool for monitoring the rapidly changing rate of growth in early infancy (9,26). They also demonstrate that healthy children from around the world who are raised in healthy environments and follow recommended feeding practices have strikingly similar patterns of growth. The ancestries of the children included in the WHO standards were widely diverse. They included people from Europe, Africa, the Middle East, Asia and Latin America. In this regard they are similar to growing numbers of populations with increasingly diverse ethnicities. These results indicate that we should expect the same potential for child growth in any country. They also imply that deviations from this pattern must be assumed to reflect adverse conditions that require correction, e.g. inadequate or lack of breastfeeding, nutrient-poor or energy-excessive complementary foods, unsanitary environments, deficient health services and/or poverty.
Technical and scientific research has validated the robustness of the WHO standards and improved understanding of the broad benefits of their use:
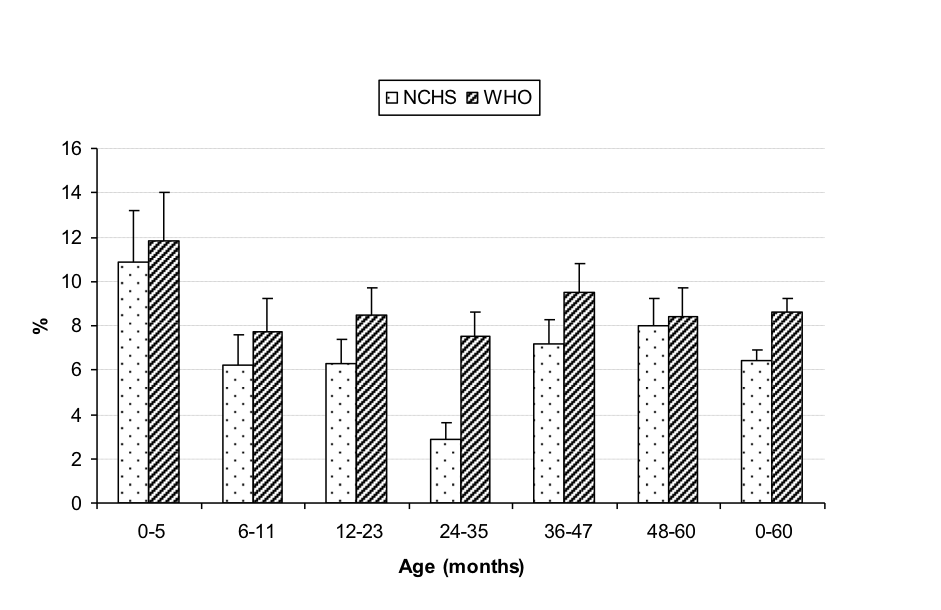
Figure 3. Prevalence of overweight (above +2 SD weight-for-length/height) by age based on the WHO standards and the NCHS reference in the Dominican Republic.
WHO growth reference for school-aged children and adolescents (61 months-19 years)
Much less is known about the growth and nutritional status of school-age children and adolescents. Reasons for this lack of knowledge include the rapid changes in somatic growth, problems of dealing with variations in maturation, and difficulties in separating normal variations from those associated with health risks.
The release of the WHO standards for preschool children and increasing public health concern over childhood obesity stirred interest in developing appropriate growth curves for school-age children and adolescents. As countries proceeded to implement WHO growth standards for preschool children, the gap across all centiles between these standards and existing growth references for older children became a matter of concern. The 1977 NCHS reference (13) and more recent examples such as the CDC 2000 reference (33,34), the IOTF cut-off points (35) and other contemporary references (36-38) all suffer from a biological drawback characterised by weight-based curves, such as the BMI, that are markedly skewed to the right, thereby redefining overweight and obesity as ‘normal’ (39,40). The upward skewness of these references results in an underestimation of overweight and obesity and an overestimation of undernutrition (e.g., prevalence of thinness or children below the 3rd percentile) (41,42). The latter is worrisome as it might prompt the overfeeding of healthy, constitutionally small children.
A potential approach to overcoming this flaw would be to use lower cut-offs to screen for overweight and obesity (40). However, better still would be to use growth curves based on samples that have achieved expected linear growth while not being affected by excessive weight gain relative to linear growth (43). The case made for using a national reference has traditionally been that it is more representative of a given country’s children than any other reference could possibly be. But given the child obesity epidemic, this is no longer valid for weight or BMI. No sooner is a new reference produced than it is out of date.
The need to harmonise growth assessment tools, conceptually and pragmatically, prompted evaluation of the feasibility of developing a single international growth reference for school-aged children and adolescents (41). Recognising the limitations of existing reference curves (e.g. the NCHS/WHO growth reference, the CDC 2000 growth charts, and the IOTF cut-offs) for assessing childhood obesity, the expert group recommended that appropriate growth curves for these age groups be developed for clinical and public health applications. It also agreed that a multicentre study, similar to that leading to the development of the WHO Child Growth Standards from birth to 5 years of age, would not be feasible for older children because it would be impossible to control the dynamics of their environment. It was thus decided that a growth reference should be constructed for this age group using available historical data (43).
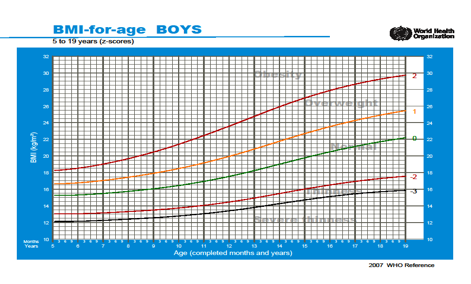
Following the expert group recommendations, WHO proceeded to reconstruct the 1977 NCHS/WHO growth reference for the period 5-19 years. It used the original sample (a non-obese sample with expected heights), supplemented with data from the WHO Child Growth Standards (to facilitate a smooth transition at 5 years), and applied state-of-the-art statistical methods (44). The new curves are closely aligned with the WHO Child Growth Standards at 5 years, and the recommended adult cut-offs for overweight and obesity at 19 years (BMI of 25 and 30, respectively)(Figure 4). The full set of tables and charts for height, weight and BMI can be found at: www.who.int/growthref/en, including application tools such as software for clinicians and public health specialists (45).
Figure 4. WHO BMI-for-age cut-offs for defining obesity, overweight, thinness and severe thinness in school-age and adolescent boys
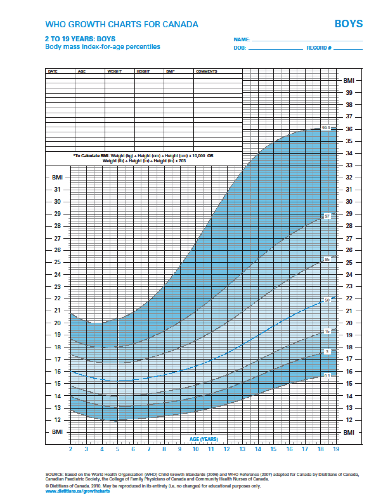
The WHO reference for school-age children and adolescents provides a suitable reference for the 5 to 19 years age group to be used in conjunction with the WHO Child Growth Standards from 0 to 5 years. Since its release in 2007 many countries have switched to using these charts including developed countries, for example Canada (Figure 5), Switzerland (46) and several others in Europe (47).
Figure 5. WHO Growth Charts for Canada. Body mass index-for-age percentiles, 2 to 19 years: boys
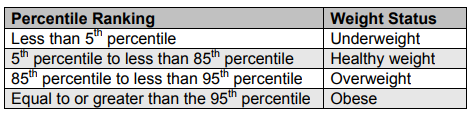
Defining childhood overweight and obesity in individuals and populations
The classification of overweight and obesity is based not only on the use of an appropriate reference population with which to compare the individual child or community; it is also grounded in the selection of a suitable anthropometric indicator together with appropriate cut-off points to classify children according to severity levels which best identify risk of overweight/obesity-related morbidity and mortality.
The body mass index, a measure of body mass relative to height, has emerged as the most practical, universally applicable, inexpensive and non-invasive anthropometric indicator for classifying overweight and obesity (4). Although there is some reluctance to describe children as obese on the basis of BMI alone, i.e. without taking into account a more direct measure of body fat (48), recognition of the difficulties inherent in obtaining more proximate measures of body fat and lack of references to interpret them has resulted in BMI-for-age alone being used to define overweight and obesity. In its favour, increased BMI-for-age in childhood and adolescence is associated with higher percentages of body fat (49-51) and known risk factors for cardiovascular disease (52). It is important to note that, in preschool-age children, weight-for-length (below two years of age) and height (above two years of age) are also valid indicators for classifying young children as overweight and obese, and can be used instead of BMI-for-age as they yield very similar results (1).
The cut-off points WHO recommends for classifying overweight and obesity in preschool-age children (0-5 years) are detailed in the training course on child growth assessment (53). Children above +1SD are described as being “at risk of overweight”, above +2SD as overweight, and above +3SD as obese. WHO has opted for a cautious approach because young children are still growing in terms of height and there are few data on the functional significance of the upper end of the BMI-for-age distribution cut-offs at such young ages in healthy populations like the WHO standards (54). Caution is all the more important given the risks for very young children, in light of their nutrient requirements for growth and development, of being placed on restrictive diets.
For older children, the WHO adolescence BMI-for-age curves at 19 years closely coincide with the definitions for adult overweight (BMI 25) at +1 SD and adult obesity (BMI 30) at +2 SD, which were derived based on associations with mortality (4). As there were no similar associations with functional outcomes in the school age and adolescent periods, the BMI cut-offs at 19 years where tracked back along the +1SD and +2SD lines to age 5 years (44)(Figure 4). Recent research shows that obese and overweight school-age children and adolescents as defined by these BMI-for-age cut-offs are at substantially increased risk for adverse levels of several cardiovascular disease risk factors such as hypertension, high insulin, high HOMA, high triglycerides, low HDL-Cho, high LDL-Cho, and high uric acid (55). These results provide evidence that the WHO cut-offs for childhood overweight and obesity are well-suited to identifying children with metabolic and vascular risk.
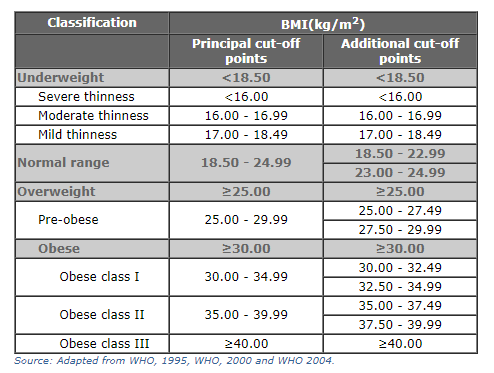
Table 1 summarizes the WHO classification of nutrition conditions in children and adolescents based on anthropometry.
Table 1: WHO Classification of nutrition conditions in children and adolescents based on anthropometry
| Classification | Condition | Age: Birth to 60 months 1,3 Indicator and cut-off | Age: 61 months to 19 years 2,3 Indicator and cut-off |
| Based on body mass index (BMI) | Possible risk of overweight | BMI-for-age (or weight-for-height) > 1SD | |
| Overweight | BMI-for-age (or weight-for-height) > 2SD | BMI-for-age >1SD(equivalent to BMI 25 kg/m 2 at 19 y) | |
| Obese | BMI-for-age (or weight-for-height) > 3SD | BMI-for-age >2SD (equivalent to BMI 30 kg/m 2 at 19 y) | |
| Thin | BMI-for-age  |
In assessing levels of severity for overweight and obesity in children under age 5 years, it is important to consider the actual value in kg of “excess” weight at different cut-offs for a still-growing 5-year-old in contrast to an adolescent who has reached adult height. For example, the “excess weight” carried by a boy of median height-for-age with a BMI-for-age of 2 SD at 19 years is 23.3 kg, while the equivalent “excess” for a boy at age 5 is 3.7 kg. Assuming that there is “excess weight” in both cases, its implications are likely greater for the former, who has reached his adult height, than for the latter, who could still grow (in terms of height) into his weight (56). When evaluating young children, clinicians might even prefer to avoid classifying a child at this age (0-5 years), and focus instead on the individual growth trajectory and the clinical assessment. Clinicians can also assess more proximate measures of body fat in individual children such as the triceps and subscapular skinfolds for which WHO standards are also available (24,26).
Conclusion
Growth curves are an essential tool in paediatric practice. Their value resides in helping to determine the degree to which physiological needs for growth and development are being met during the important childhood period. However, their usefulness goes far beyond assessing children’s nutritional status. Many governmental and international intergovernmental and nongovernmental agencies rely on growth charts for assessing the general well-being of populations, formulating health and related policies, and planning interventions and monitoring their effectiveness.
Accurate interpretation of child growth depends on prescriptive standards or, if unavailable, on reference data that accurately estimate the prevalence of overweight and obesity. Using the right growth curves is crucial since the accurate evaluation of growth trajectories and the appropriate choice of interventions to improve child health are determined on this basis.
There is broad international consensus concerning the utility of the WHO Child Growth Standards for assessing the growth of children 0 to 5 years of age. The standards are derived from children who were raised in environments that minimised constraints to growth such as poor diets and infection. In addition, their mothers followed healthy practices such as breastfeeding and not smoking during and after pregnancy. The standards depict normal human growth under optimal environmental conditions and can be used to assess children everywhere, regardless of ethnicity, socioeconomic status and type of feeding. They also demonstrate that healthy children from around the world who are raised in healthy environments and follow recommended feeding practices have strikingly similar patterns of growth.
The International Pediatric Association (57) and several other national and international professional associations have endorsed the use of the WHO growth standards. The European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) (42,58) has also recommended their use in Europe. According to ESPGHAN, infants who are breastfed for the first 12 months of life show a slower growth pattern during infancy, which is likely to be associated with less obesity and improved health later in life. Another justification for their recommendation is that use of the standards has the potential to encourage prolonged breastfeeding and increase awareness about early obesity (42).
To complement the growth standards for under-five children, WHO developed a growth reference for school-aged children and adolescents. The reference’s curves are closely aligned with the WHO Child Growth Standards at 5 years, and the recommended adult cut-offs for overweight and obesity at 19 years. They fill the growth-curve gap and provide an appropriate reference for the 5 to 19 years age group. Obesity and overweight defined using the WHO BMI-for-age cut-offs identify children with higher metabolic and vascular risk, while emphasising the importance of preventing overweight and obesity in childhood to reduce cardiovascular risk.
As a final note, it is essential that the same reference data be used in assessing both individuals (clinical use) and populations (health planning use) to ensure coherence between what paediatricians see in their daily practice and the population-based data health planners use in designing treatment and preventive services.
Note: WHO holds the copyright for the WHO Child Growth Standards and the WHO Growth Reference for School-aged Children and Adolescents.
Mental Health
In this entry we present the latest estimates of mental health disorder prevalence and the associated disease burden. Most of the estimates presented in this entry are produced by the Institute for Health Metrics and Evaluation and reported in their flagship Global Burden of Disease study.
For 2017 this study estimates that 792 million people lived with a mental health disorder. This is slightly more than one in ten people globally (10.7%)
Mental health disorders are complex and can take many forms. The underlying sources of the data presented in this entry apply specific definitions (which we describe in each relevant section), typically in accordance with WHO’s International Classification of Diseases (ICD-10). This broad definition incorporates many forms, including depression, anxiety, bipolar, eating disorders and schizophrenia.
Mental health disorders remain widely under-reported — in our section on Data Quality & Definitions we discuss the challenges of dealing with this data. This is true across all countries, but particularly at lower incomes where data is scarcer, and there is less attention and treatment for mental health disorders. Figures presented in this entry should be taken as estimates of mental health disorder prevalence — they do not reflect diagnosis data (which would provide the global perspective on diagnosis, rather than actual prevalence differences), but are imputed from a combination of medical, epidemiological data, surveys and meta-regression modelling where raw data is unavailable. Further information can be found here.
It is also important to keep in mind that the uncertainty of the data on mental health is generally high so we should be cautious about interpreting changes over time and differences between countries.
The data shown in this entry demonstrate that mental health disorders are common everywhere. Improving awareness, recognition, support and treatment for this range of disorders should therefore be an essential focus for global health.
The table here provides a summary of the data which follows on mental health and substance use disorders. Clicking on a given disorder will take you to the relevant section for further data and information.
Related entries:
The Global Burden of Disease study aggregates substance use disorders (alcohol and drug use disorders) with mental health disorders in many statistics. In the discussion of the prevalence we have followed this practice, but we will change it in future updates of this research.
We address substance use disorders (alcohol and drug use disorders) in separate entries on Substance Use and Alcohol Consumption.
| Disorder | Share of global population with disorder (2017) |
|---|
[difference across countries]
11.9% females
All our interactive charts on Mental Health
Empirical View
Prevalence of mental health and substance use disorders
The predominant focus of this entry is the prevalence and impacts of mental health disorders (with Substance Use and Alcohol Use disorders covered in individual entries). However, it is useful as introduction to understand the total prevalence and disease burden which results from the broad IHME and WHO category of ‘mental health and substance use disorders’. This category comprises a range of disorders including depression, anxiety, bipolar, eating disorders, schizophrenia, intellectual developmental disability, and alcohol and drug use disorders.
Mental and substance use disorders are common globally
In the map we see that globally, mental and substance use disorders are very common: around 1-in-7 people (15%) have one or more mental or substance use disorders.
Click to open interactive version
Prevalence of mental health disorders by disorder type
It’s estimated that 970 million people worldwide had a mental or substance use disorder in 2017. The largest number of people had an anxiety disorder, estimated at around 4 percent of the population.
Click to open interactive version
Prevalence of mental health disorders by genders
The scatterplot compares the prevalence of these disorders between males and females. Taken together we see that in most countries this group of disorders is more common for women than for men. However, as is shown later in this entry and in our entries on Substance Use and Alcohol, this varies significantly by disorder type: on average, depression, anxiety, eating disorders, and bipolar disorder is more prevalent in women. Gender differences in schizophrenia prevalence are mixed across countries, but it is typically more common in men. Alcohol and drug use disorders are more common in men.
Click to open interactive version
Deaths from mental health and substance use disorders
The direct death toll from mental health and substance use disorders is typically low. In this entry, the only direct death estimates result from eating disorders, which occur through malnutrition and related health complications. Direct deaths can also result from alcohol and substance use disorders; these are covered in our entry on Substance Use.
However, mental health disorders are also attributed to significant number of indirect deaths through suicide and self-harm. Suicide deaths are strongly linked — although not always attributed to — mental health disorders. We discuss the evidence of this link between mental health and suicide in detail later in this entry.
In high-income countries, meta-analyses suggest that up to 90 percent of suicide deaths result from underlying mental and substance use disorders. However, in middle to lower-income countries there is evidence that this figure is notably lower. A study by Ferrari et al. (2015) attempted to determine the share disease burden from suicide which could be attributed to mental health or substance use disorders. 1
Based on review across a number of meta-analysis studies the authors estimated that only 68 percent of suicides across China, Taiwan and India were attributed to mental health and substance use disorders. Here, studies suggest a large number of suicides result from the ‘dysphoric affect’ and ‘impulsivity’ (which are not defined as a mental and substance use disorder). It is important to understand the differing nature of self-harm methods between countries; in these countries a high percentage of self-harming behaviours are carried out through more lethal methods such as poisoning (often through pesticides) and self-immolation. This means many self-harming behaviours can prove fatal, even if there was no clear intent to die.
As a result, direct attribution of suicide deaths to mental health disorders is difficult. Nonetheless, it’s estimated that a large share of suicide deaths link back to mental health. Studies suggest that for an individual with depression the risk of suicide is around 20 times higher than an individual without.
Disease burden of mental health and substance use disorders
Health impacts are often measured in terms of total numbers of deaths, but a focus on mortality means that the burden of mental health disorders can be underestimated. 2 Measuring the health impact by mortality alone fails to capture the impact that mental health disorders have on an individual’s wellbeing. The ‘disease burden‘ – measured in Disability-Adjusted Life Years (DALYs) – considers not only the mortality associated with a disorder, but also years lived with disability or health burden. The map shows DALYs as a share of total disease burden; mental and substance use disorders account for around 5 percent of global disease burden in 2017, but this reaches up to 10 percent in several countries. These disorders have the highest contribution to overall health burden in Australia, Saudi Arabia and Iran.
Click to open interactive version
Depression
Definition of depression
Depressive disorders occur with varying severity. The WHO’s International Classification of Diseases (ICD-10) define this set of disorders ranging from mild to moderate to severe. The IHME adopt such definitions by disaggregating to mild, persistent depression (dysthymia) and major depressive disorder (severe).
All forms of depressive disorder experience some of the following symptoms:
Mild persistent depression (dysthymia) tends to have the following diagnostic guidelines:
“Depressed mood, loss of interest and enjoyment, and increased fatiguability are usually regarded as the most typical symptoms of depression, and at least two of these, plus at least two of the other symptoms described on page 119 (for F32.-) should usually be present for a definite diagnosis. None of the symptoms should be present to an intense degree. Minimum duration of the whole episode is about 2 weeks. An individual with a mild depressive episode is usually distressed by the symptoms and has some difficulty in continuing with ordinary work and social activities, but will probably not cease to function completely.”
Severe depressive disorder tends to have the following diagnostic guidelines:
“In a severe depressive episode, the sufferer usually shows considerable distress or agitation, unless retardation is a marked feature. Loss of self-esteem or feelings of uselessness or guilt are likely to be prominent, and suicide is a distinct danger in particularly severe cases. It is presumed here that the somatic syndrome will almost always be present in a severe depressive episode. During a severe depressive episode it is very unlikely that the sufferer will be able to continue with social, work, or domestic activities, except to a very limited extent.”
The series of charts below present the latest global estimates of the prevalence and disease burden of depressive disorders. Depressive disorders, as defined by the underlying source, cover a spectrum of severity ranging from mild persistent depression (dysthymia) to major (severe) depressive disorder. The data presented below includes all forms of depression across this spectrum.
Prevalence of depressive disorders
The share of population with depression ranges mostly between 2% and 6% around the world today. Globally, older individuals (in the 70 years and older age bracket) have a higher risk of depression relative to other age groups.
Click to open interactive version
Click to open interactive version
In 2017, an estimated 264 million people in the world experienced depression. A breakdown of the number of people with depression by world region can be seen here and a country by country view on a world map is here.
In all countries the median estimate for the prevalence of depression is higher for women than for men.
DALYs from depression
The chart found here shows the health burden of depression as measured in Disability Adjusted Life Years (DALYs) per 100,000. A time-series perspective on DALYs by age is here.
Depression is complicated – this is how our understanding of the condition has evolved over time
People often think of depression as a single, uniform condition – deep sadness and a loss of interest in the activities that someone usually enjoys. But depression is complicated and it’s difficult to define what it means in an objective way.
This is because depression is a condition of the mind: it is diagnosed based on people’s psychological symptoms and behavior, not from a brain scan or markers in their blood or DNA.
When we diagnose depression, we have to rely on people to recall their own symptoms. We have to trust that doctors will observe and probe their symptoms reliably. We have to analyze this information to understand what people with depression experience that other people don’t.
Our ability to do all of these things accurately has changed over time, and so has our understanding of depression.
This comes down to three factors.
First, many countries now screen for depression in the general population, not just in a subset of people who are seen by a small number of doctors. In many studies, researchers track patients over long periods of time to understand how the condition progresses.
Second, we use questionnaires and interviews that treat depression as a condition that can occur at different levels and change with time.
Third, we have better statistical tools to help us refine questionnaires and understand how symptoms are related to one another.
Let’s look at each of these factors in more detail before we explore how they have informed our understanding of depression.
Surveying depression in the general population
Depression traces back to a condition called ‘melancholia.’ The concept of melancholia itself shifted in meaning several times in history. In ancient Greek medicine, it referred to a general condition of sadness and fear. From the 16th century, it was generally considered a type of insanity, and symptoms such as delusions and suspicion became more of a focus in these descriptions. Some people with these symptoms would likely be diagnosed with schizophrenia today.
From the late 18th century onwards, these symptoms became less emphasized, while fatigue and distress became more central to the diagnosis. Over the same time, the word depression was increasingly used in descriptions of melancholia. Since the 20th century, melancholia has been the name given to a severe subtype of depression. 3
In the 19th century in Britain, for example, the diagnosis of melancholia was mainly used to decide who to admit to asylums. It was diagnosed based on the judgment of individual physicians who used different methods, and many asylums used broad definitions of suicidality. Talking about death, drinking too much alcohol, refusing food, having thoughts of guilt or damnation, having a fear of persecution, and any kind of self-harm could all be considered suicidal tendencies. 4
Different asylums in Britain used different classification systems. This meant that statistics were difficult to compare between regions and were controversial, even at the time. Asylums would only record the overall number of patients with each condition – they wouldn’t record the symptoms of individual patients. 5 In contrast, in Imperial Germany, detailed information about asylum patients was collected using census cards. 6
Some psychiatrists such as Emil Kraepelin and Philippe Pinel monitored people in asylums in a systematic way. They noted which symptoms they had and how their illness changed over long periods of time. With that information, they designed systems to classify people with disorders. 7
For example, Kraepelin noticed that some people with psychosis also had periods of depression, while others did not. He called the former condition ‘manic depression’ (which we would now understand as bipolar disorder or depression) and the latter ‘dementia praecox’ (which we now understand as schizophrenia).
These kinds of classifications began to be applied at large in asylums across Europe.
At the same time, psychologists began to devise questionnaires to measure people’s symptoms empirically. They developed various scales and tested them with college students before applying them to adults in the general population. Large organizations such as the American Psychological Association developed criteria that could be used to diagnose patients in a standardized way.
Depression is a condition that is increasingly recognized and surveyed in the population as a whole.
Now, we collect data on depression from two sources. First, we have data on diagnoses made by doctors. In many countries, doctors inquire about people’s symptoms and how much they correspond to the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM). They also use tests to rule out medical conditions, such as thyroid disorders, that result in similar symptoms. Second, we have data on the severity of depression. This data is collected from patients and the general population, using many different questionnaires and rating scales. 8 But there are still gaps in our knowledge. Data is lacking especially in many poorer places around the world. Even within high-income countries, people with poorer health or severe depression are much less likely to respond to these community surveys or report their symptoms accurately. If we didn’t take this into account, we would underestimate the prevalence of depression in the population. 9
Measuring depression on levels
The second reason that we understand depression more accurately now is that we ask more nuanced questions about symptoms.
Depression as measured by Kraepelin focused only on whether symptoms were present or absent. But the measures that are used for screening or diagnosis today go much further. 10 Now, people are asked about how frequent or severe their symptoms are.
For example, if someone has trouble sleeping, how many days does that occur each week? If they feel guilt, how often do they feel guilty? How guilty do they feel?
Do they often think about things they did wrong a long time ago? Do they blame themselves for having depression, seeing it as punishment? Do they hear voices accusing them or see hallucinations that threaten them?
We can use more specific questions like this to rate each symptom on levels that relate to how frequent or severe they are. We can place possible answers on a range from, say, 0 to 3. A person’s scores across all the symptoms can then be added up to give a total, and we can use cut-offs to classify an episode as ‘mild’, ‘moderate’ or ‘severe’ depression.
This was a huge step forward. It meant we could find out if patients with mild depression tended to be different from those with severe depression. We could also find out if they responded differently to treatment.
Most importantly though, these ratings have allowed us to record subtle changes over time. Many of these scales were developed as antidepressants were discovered and psychotherapy became more widely used, and the scales were used to track how patients improved while on these treatments. With a crude diagnosis, it would be difficult to detect subtle improvements in patients. 11
What this means is that the way we conceptualize depression today is not as a fixed condition, but as something that can occur at varying degrees and that can potentially resolve.
People might experience symptoms on some days but not others, and they might have symptoms that become milder with time. The questionnaires we use probe symptoms in a way that measures how they might change, and how they might be treatable.
Analyzing depression with more rigour
We’ve seen how depression has been screened in the wider population and how it is measured in a more nuanced way.
But how would we find out whether these questionnaires were actually measuring depression? How would we know that people’s symptoms were being interpreted in a consistent way?
In the 19th and 20th centuries, statisticians began to develop techniques to measure many aspects of questionnaires, so they could refine them. They were interested in understanding how consistently the questions measured the same underlying concept.
They were also concerned with testing how people’s responses on a questionnaire reflected their behavior in the real world. They could do this, for example, by estimating how their scores on a depression questionnaire correlated with their ability to work or study.
They began to put more focus into understanding how much we could rely on the judgment of individual doctors, instead of treating them as infallible experts.
This was important because patients were included in clinical trials based on their scores on these questionnaires. If doctors had wildly different methods of scoring patients on the questionnaires, it would be very hard to compare patients with each other. It would also be hard to compare patients’ scores at the start of a trial to their scores at the end.
Finally, they were interested in understanding how the symptoms of depression related to each other, and whether it was appropriate to simply add up people’s scores into a total. In the 20th century, statisticians developed methods such as factor analysis and item response theory that could be used to dig into these questions. 12
These issues are explained in more detail in the box below. Until recently, it was difficult to apply some of these techniques in datasets that had a large number of people or questions because they required a lot of computational power. 13
With all of that in mind, what do we know about depression now?
What are the challenges of measuring depression?
Content validity: We might want to know whether the questionnaires were measuring depression at all. How would we be sure of this?
We could first think about which emotions and behaviors we associate with depression – sadness, tiredness, guilt, a loss of energy, and so on – and we could make sure that the questionnaires ask about all of these emotions.
Criterion validity: We could also find out if peoples’ responses to the questions are correlated with other things we associate with depression.
For example, if someone is severely depressed, we might expect that they are also less sociable and that they perform poorly at work or school. We could test whether this is the case for people who scored high on a questionnaire for depression.
Discriminant validity: We could also test whether their responses are uncorrelated with things we don’t associate with depression, such as their height or intelligence.
Internal consistency: Another important thing we’d want to know is whether the questions were actually tapping into the same phenomenon.
Do all the questions measure depression or are some measuring other concepts instead? To test for this, we could look at how closely people’s answers to different questions align with each other.
One consequence of this focus is that scores shouldn’t also measure other concepts.
For example, some people have phases of depression, but also have phases of mania at other times (where they might feel highly irritable or excited). Some of these symptoms seem to be opposites of depression. So, these symptoms should be scored as part of separate concepts, such as a manic phase in bipolar disorder, if we wanted a scoring system with high internal consistency.
Inter-rater reliability: If multiple doctors could not come to agreement about how depressed patients were, despite using the same questionnaire, it would hardly be useful. It would make it very difficult to compare patients with each other, especially because many of them would only be seen by a single doctor before they received treatment.
Fortunately, there are straightforward ways to test this: we could measure how consistent different doctors were at diagnosing the same patients.
Latent trait measurement: Apart from the issues above, we’d also want to find out what the scores on a questionnaire tell us about the severity of depression.
For example, we might wonder if it is appropriate to simply add up the ratings across all the questions to get a total score. And we might wonder how the questions are related to each other.
Latent class analysis: On the other side of the questions are the people who answer them. We might wonder if we can classify people who respond to the questionnaires into clusters based on how they respond. How different are these clusters, and do they matter? Answering these questions is the aim of latent class analysis, which was developed in the middle of the 20th century.
Sleeping problems and low energy tend to be the most common symptoms of depression
First of all, we know that some of the symptoms of depression are common in the population, even among those who do not suffer from depression.
You can see this in the chart below. It lists symptoms of depression and shows responses from the general US population. The questions come from the PHQ-9 (the patient health questionnaire), which is a popular rating scale for depression that is used around the world and covers all the symptoms in the DSM diagnostic criteria for major depression. 14
This questionnaire asks people about how often they have experienced symptoms of depression in the last two weeks. Half of the respondents (51%) had low energy, and more than one-third (37%) had trouble sleeping. 15 Sleeping problems and low energy are also some of the most common symptoms in people who are diagnosed with moderate or severe depression.
Click to open interactive version
People experience different combinations of symptoms
Even though some symptoms are common, depression is complicated. What makes it complicated is not the prevalence of individual symptoms, but rather the differences in the combinations of symptoms that patients experience. We see these combinations in the chart below, using symptoms in the Quick Inventory of Depressive Symptoms (QIDS-16), another questionnaire that covers all of the symptoms of depression in the DSM. 16
On the horizontal bars, you can see which symptoms patients have. In this chart, symptoms are marked as present if people experienced them to a moderate or severe degree.
The first thing to notice in this chart is that patients can experience many combinations of symptoms. What’s surprising is how uncommon each combination is. The most common combination is experienced by less than 2% of patients. The combinations of people’s symptoms vary widely.
The second thing to notice is that the most widely reported combination is, in fact, no symptoms at all. This is shown as ‘none’ in the chart. Many patients were diagnosed with moderate or severe depression but didn’t report having any of the individual symptoms to a moderate or severe degree. Instead, patients with the profile of “none” had all of the symptoms to a mild degree. This gave them a total score that was high, and meant they would still be considered to have moderate or even severe depression.
Think about the way that depression questionnaires are scored: each item is rated on a scale and the ratings across all the scales are added together.
This means that people can end up with a high total by rating many symptoms at a ‘mild’ level, or by rating some symptoms ‘severe’ and others ‘absent’, or something in between.
You might wonder if we should treat these different possibilities as equivalent to each other.
Is this a bug or a feature of questionnaires?
If it was a feature, it would imply that when people are mildly depressed, they would probably only experience a few symptoms, such as those that are common, like insomnia. Meanwhile, when people are more severely depressed, they would be more likely to experience more symptoms, including ones that are uncommon, like self-blame and suicidal thoughts.
In the 20th century, statisticians such as Georg Rasch, Jane Loevinger and Robert J Mokken developed models that could be used to test this assumption.
These models test whether people who have uncommon symptoms also have more symptoms overall. They also test whether the scores assigned to each level are appropriate. These assumptions seem to be valid for some questionnaires, including the PHQ-9 and the Hamilton Rating Scale for Depression. 17 This means that adding up people’s scores on these questionnaires is an appropriate way to understand how severely they are depressed.
Depression is an umbrella condition which contains subtypes
We can find out how people’s responses to questionnaires are related to each other through a method called factor analysis.
Using this method, researchers have usually found that some symptoms are more likely to occur together. In other words, the symptoms are part of groups – they reflect underlying traits called ‘latent factors.’ The latent factors that researchers have usually found are sadness, guilt, changes in sleep and appetite, and despair about the future. 18
These latent factors also correlate with each other to a moderate degree, and researchers often find an underlying “general dimension” of depression.
If you knew where someone placed on this general dimension, you would be able to roughly predict which symptoms they had and how many symptoms they had. But their specific symptoms would still be informative and important to understand.
To investigate this more, some researchers use a method called “latent class analysis.” What this does is it tries to identify whether people can be classified into subtypes based on how they respond to questionnaires.
Plenty of studies have used latent class analysis to understand whether there are subtypes of depression. But different studies have identified very different numbers of subtypes, which might be because they analyzed different sets of questions.
Some subtypes relate to how severely people experience depression, while others relate to which symptoms they have. But it is unclear what they mean, how valid some of them are, and how well they have been measured. 19 For example, one subtype is called atypical depression, which usually refers to patients who sleep excessively and gain weight.
According to the DSM 5 criteria, people can only be diagnosed with atypical depression if they have ‘mood reactivity’, which refers to when someone can respond positively to good things that happen in their life.
This contrasts with another subtype of depression, called melancholic depression, where people have more severe sadness and find it difficult to feel happy even during these circumstances.
But there is lots of evidence that goes against the idea that mood reactivity is important for identifying people with atypical depression. In other words, people with symptoms of typical or atypical depression are equally likely to have mood reactivity. 20
The different subtypes of depression are not stable over time. Studies that follow patients for long periods of time find that those who have multiple episodes of depression tend to fluctuate between having some episodes that are considered typical and others that are considered atypical or melancholic. 21
The symptoms of depression tend to change over time
This brings us to another important fact about depression: the symptoms change over time. This is true for which symptoms people report as well as how severe they are.
You can see this in the chart, among people who are diagnosed with depression. Patients’ total scores declined over time after they were diagnosed. The curves of depression scores shift towards the left when patients are surveyed months after the initial questionnaire. This effect is found across many different questionnaires, as shown.
One explanation for this is that their symptoms become milder over time. For example, patients are likely to seek help when they have very severe symptoms, which would become milder later on. This is known as ‘regression to the mean.’ Another explanation is that there is a change in the combination of symptoms they report. 22
Episodes of depression can occur frequently
Some people have episodes of depression frequently. We know this because researchers have regularly interviewed the same people over many years. This gives us more accurate results than relying on them to remember which symptoms they had in the past. One study tracked people’s symptoms over a period of more than thirteen years. 23 It took the average person two to three years after their first depressive episode to have a year without depression. This measure – of how long it takes until the average person has a full year without depression – is known as the ‘median time to recovery’.
People’s experiences of depression varied widely. Half of the patients recovered within the same year. In contrast, a small proportion of patients (15%) did not recover even more than 20 years later; they had depression in every year of the study. You can see this in the chart.
Even among those that recovered, almost half (45%) had another episode of depression during the period of the study.
What all of this tells us is that the condition can progress in different ways.
Some people experience episodes very infrequently: possibly only a single episode followed by years or decades without any recurrences. Others have episodes frequently.
Episodes of depression can last a long time
Apart from having episodes of depression frequently, some people also have episodes that last for years.
The DSM criteria requires patients to have symptoms of depression for at least two weeks before they can be diagnosed, but an episode of depression lasts around three months on average. 24 There is a lot of variation between people. When people have episodes that last over two years, their condition is labeled chronic depression.
Is there something different about these patients?
People who have chronic depression tend to be different from the average patient in several ways. They are more likely to also have other conditions, such as anxiety disorder, and more likely to have a family history of mental illness. They are also more likely to have had depression for the first time when they were young, typically under the age of 25. 25
This is another way that depression is complex: it occurs at widely different times in people’s lives. The most likely age when people develop depression for the first time (the modal age of onset) is around 19. 26 But most patients develop it much later than this. In this meta-analysis, the median age of onset was around 31, while a quarter of people developed depression for the first time when they were older than 46 years old. There are large differences in the age of onset, as you can see in the chart.
Depression is complicated
How do we pull this knowledge together to understand depression as a whole?
One simple way to think about depression is to imagine episodes as a series of waves (shown below), where each episode lasts for weeks or months, before the episode ends.
For some people, this will be their only experience of depression for years, possibly ever. After a single wave of symptoms, they will have recovered.
For others, even after an episode of severe depression, they might still have a high baseline level of symptoms. Their level of “normalcy” might still be mild depression.
In this way, we can think of people’s symptoms getting progressively worse during an episode, improving, and potentially worsening again, resulting in a relapse.
Episodes of depression can last different lengths of time. Some people will have episodes that are mild, while others will have episodes that are severe. Many will have a combination of mild and severe episodes. Some will experience many episodes of depression, while others will only experience one episode or none at all.
Conclusion
Depression is one of the most common mental health conditions in the world, so the intricacies of the condition have important consequences for a large number of people. Our understanding of depression influences how we diagnose the condition. It influences how we manage and treat it, and how we track changes in its levels over time.
There is a lot we already know about depression, but there is still a lot that is less clear.
Depression is a condition of the mind, which makes it difficult to study. We still have to rely on people to report their symptoms accurately. Studies have suggested there are many subtypes of depression, but we have limited information on how valid they all are and how to define them.
Depression is a condition of the mind, but that doesn’t mean it’s impossible to understand. With wider surveys, granular scales and more rigorous analysis, we’re uncovering just how complex this condition is. We’re able to find out how the symptoms are related to each other and how common they are.
We now know that people with depression experience different symptoms, with different levels of severity, at different times in their lives, and have episodes lasting different lengths of time. People’s symptoms vary and change over time and we can now measure how that happens.
In the following posts, we’ll explore more of these topics in detail. We’ll see how common depression is and how it varies between people.
We’ll look into antidepressant medication: how it is prescribed, how many people use it, and how effective it is. Finally, we’ll find out what we don’t know about depression and antidepressants, and why it has been difficult to answer many important questions about this condition that affects so many people worldwide.
Anxiety disorders
Definition of anxiety disorders
Anxiety disorders arise in a number of forms including phobic, social, obsessive compulsive (OCD), post-traumatic disorder (PTSD), or generalized anxiety disorders.
The symptoms and diagnostic criteria for each subset of anxiety disorders are unique. However, collectively the WHO’s International Classification of Diseases (ICD-10) note frequent symptoms of:
“(a) apprehension (worries about future misfortunes, feeling “on edge”, difficulty in concentrating, etc.);
(b) motor tension (restless fidgeting, tension headaches, trembling, inability to relax);
(c) autonomic overactivity (lightheadedness, sweating, tachycardia or tachypnoea, epigastric discomfort, dizziness, dry mouth, etc.).”
The series of charts here present global data on the prevalence and disease burden which results from this range of anxiety disorders.
Prevalence of anxiety disorders
The prevalence of anxiety disorders across the world varies from 2.5 to 7 percent by country. Globally an estimated 284 million people experienced an anxiety disorder in 2017, making it the most prevalent mental health or neurodevelopmental disorder. Around 63 percent (179 million) were female, relative to 105 million males.
Click to open interactive version
Click to open interactive version
In all countries women are more likely to experience anxiety disorders than men. Prevalence trends by age can be found here.
DALYs from anxiety disorders
The chart found here shows the health burden of depression as measured in Disability Adjusted Life Years (DALYs) per 100,000. A time-series perspective on DALYs by age is here.
Bipolar disorder
Definition of Bipolar disorder
Bipolar disorder (also termed bipolar affective disorder) is defined by the WHO’s International Classification of Diseases (ICD-10) as follows:
“This disorder is characterized by repeated (i.e. at least two) episodes in which the patient’s mood and activity levels are significantly disturbed, this disturbance consisting on some occasions of an elevation of mood and increased energy and activity (mania or hypomania), and on others of a lowering of mood and decreased energy and activity (depression). Characteristically, recovery is usually complete between episodes, and the incidence in the two sexes is more nearly equal than in other mood disorders. As patients who suffer only from repeated episodes of mania are comparatively rare, and resemble (in their family history, premorbid personality, age of onset, and long-term prognosis) those who also have at least occasional episodes of depression, such patients are classified as bipolar.”
The charts here present global data on the prevalence and disease burden of bipolar disorder.
Prevalence of bipolar disorder
The prevalence of bipolar disorder across the world varies from 0.3 to 1.2 percent by country. Globally, an estimated 46 million people in the world had bipolar disorder in 2017, with 52 and 48 percent being female and male, respectively.
In almost all countries women are more likely to experience bipolar disorder than men. Prevalence of bipolar disorder by age can be found here.
Click to open interactive version
Click to open interactive version
DALYs from bipolar disorder
The chart found here shows the health burden of depression as measured in Disability Adjusted Life Years (DALYs) per 100,000. A time-series perspective on DALYs by age is here.
Eating disorders
Eating disorders are defined as psychiatric conditions defined by patterns of disordered eating. This therefore incorporates a spectrum of disordered eating behaviours. The underlying sources presented here present data only for the disorders of anorexia and bulimia nervosa (as defined below). It is however recognised that a large share of eating disorders fall outwith the definition of either anorexia or bulimia nervosa (these are often termed ‘eating disorders not otherwise specified’; EDNOS) — some estimates report at least 60 percent of eating disorders do not meet the standard criteria. 28
It is therefore expected that the data presented below significantly underestimates the true prevalence of eating disorders, since it concerns only clinically-diagnosed anorexia and bulimia nervosa.
Anorexia nervosa
“Anorexia nervosa is a disorder exemplified by deliberate weight loss, and associated with undernutrition of varying severity.
For a definite diagnosis, the ICD note that all the following are required:
(a) Body weight is maintained at least 15% below that expected (either lost or never achieved), or Quetelet’s body-mass index4 is 17.5 or less. 4 Quetelet’s body-mass index = weight (kg) to be used for age 16 or more – 139 – Prepubertal patients may show failure to make the expected weight gain during the period of growth;
(b) The weight loss is self-induced by avoidance of “fattening foods”. One or more of the following may also be present: self-induced vomiting; self-induced purging; excessive exercise; use of appetite suppressants and/or diuretics;
(c) There is body-image distortion in the form of a specific psychopathology whereby a dread of fatness persists as an intrusive, overvalued idea and the patient imposes a low weight threshold on himself or herself;
(d) A widespread endocrine disorder involving the hypothalamic – pituitary – gonadal axis is manifest in women as amenorrhoea and in men as a loss of sexual interest and potency. (An apparent exception is the persistence of vaginal bleeds in anorexic women who are receiving replacement hormonal therapy, most commonly taken as a contraceptive pill.) There may also be elevated levels of growth hormone, raised levels of cortisol, changes in the peripheral metabolism of the thyroid hormone, and abnormalities of insulin secretion;
(e) If onset is prepubertal, the sequence of pubertal events is delayed or even arrested (growth ceases; in girls the breasts do not develop and there is a primary amenorrhoea; in boys the genitals remain juvenile). With recovery, puberty is often completed normally, but the menarche is late.”
Bulimia nervosa
“Bulimia nervosa is an illness defined by repeated behaviours of overeating, preoccupation with control of body weight, and the adoption of extreme measures to mitigate the impacts of overeating.
For a definite diagnosis, the ICD note that all the following are required:
(a) There is a persistent preoccupation with eating, and an irresistible craving for food; the patient succumbs to episodes of overeating in which large amounts of food are consumed in short periods of time.
(b) The patient attempts to counteract the “fattening” effects of food by one or more of the following: self-induced vomiting; purgative abuse, alternating periods of starvation; use of drugs such as appetite suppressants, thyroid preparations or diuretics. When bulimia occurs in diabetic patients they may choose to neglect their insulin treatment.
(c) The psychopathology consists of a morbid dread of fatness and the patient sets herself or himself a sharply defined weight threshold, well below the premorbid weight that constitutes the optimum or healthy weight in the opinion of the physician. There is often, but not always, a history of an earlier episode of anorexia nervosa, the interval between the two disorders ranging from a few months to several years. This earlier episode may have been fully expressed, or may have assumed a minor cryptic form with a moderate loss of weight and/or a transient phase of amenorrhoea.”
Prevalence of eating disorders
The prevalence of eating disorders (anorexia and bulimia nervosa) ranges from 0.1 to 1 percent by country. Globally an estimated 16 million had clinical anorexia and bulimia nervosa in 2017. Bulimia was more common: around 79 percent had bulimia nervosa.
Click to open interactive version
Click to open interactive version
In every country women are more likely to experience an eating disorder than men. Eating disorders tend to be more common in young adults aged between 15 and 34 years old. Trends in prevalence by age can be found here.
Deaths from eating disorders
Direct deaths can result from eating disorders through malnutrition and related health complications. The chart shows the estimated number of direct deaths from anorexia and bulimia nervosa. Evidence suggests that having an eating disorder can increase the relative risk of suicide; suicide deaths in this case are not included here.
Trends in death rates from eating disorders can be found here.
Click to open interactive version
DALYs from eating disorders
The chart found here shows the health burden of eating disorders as measured in Disability Adjusted Life Years (DALYs) per 100,000. A time-series perspective on DALYs by age is here.
Schizophrenia
Schizophrenia is defined by the IHME based on the definition within the WHO’s International Classification of Diseases (ICD-10) as:
“The normal requirement for a diagnosis of schizophrenia is that a minimum of one very clear symptom (and usually two or more if less clear-cut) belonging to any one of the groups listed as (a) to (d) below, or symptoms from at least two of the groups referred to as (e) to (h), should have been clearly present for most of the time during a period of 1 month or more:
The following charts present global-level data on the prevalence of schizophrenia.
Prevalence of schizophrenia
The prevalence of schizophrenia typically ranges from 0.2 to 0.4 percent across countries. It’s estimated that 20 million people in world had schizophrenia in 2017; the number of men and women with schizophrenia was approximately the same (around 10 million each).
Click to open interactive version
Click to open interactive version
Overall the prevalence of schizophrenia is slightly higher in men than women. Prevalence by age can be found here.
DALYs from schizophrenia
The chart found here shows the health burden of schizophrenia as measured in Disability Adjusted Life Years (DALYs) per 100,000. A time-series perspective on DALYs by age is here.
Correlates, Determinants & Consequences
Risk factors for mental health
The determinants, onset and severity of mental health disorders are complex – they can rarely be attributed to a single factor. Identifying potential risk factors form an important element of health research, potential prevention and in some cases, appropriate treatment; nonetheless, many risk factors remain only correlates of observed patterns in mental health. They therefore need to be interpreted carefully.
The World Health Organization synthesize the potential contributors to mental health and wellbeing into three categories: 29
In the table we see the WHO’s breakdown of potential adverse and protective factors for mental health within these three categories. These factors often interact, compound or negate one another and should therefore not be considered as individual traits or exposures. For example, particular individual traits may make a given person more vulnerable to mental health disorders with the onset of a particular economic or social scenario — the instance of one does not necessarily result in a mental health disorder, but combined there is a significantly higher vulnerability.
| Level | Adverse Factors | Protective Factors |
|---|---|---|
| Individual attributes | Low self-esteem | Self-esteem, confidence |
| Cognitive/emotional immaturity | Ability to solve problems & manage stress or adversity | |
| Difficulties in communicating | Communication skills | |
| Medical illness, substance use | Physical health, fitness | |
| Social circumstances | Loneliness, bereavement | Social support of family & friends |
| Neglect, family conflict | Good parenting/family interaction | |
| Exposure to violence/abuse | Physical security & safety | |
| Low income & poverty | Economic security | |
| Difficulties or failure at school | Scholastic achievement | |
| Work stress, unemployment | Satisfaction & success at work | |
| Environmental factors | Poor access to basic services | Equality of access to basic services |
| Injustice & discrimination | Social justice, tolerance, integration | |
| Social & gender inequalities | Social & gender equality | |
| Exposure to war or disaster | Physical security & safety |
Risk factors through the life-course
The risk factors and influencers on mental health vary significantly for an individual as they move through the life-course. The following are acknowledged risk factors for a given stage of life. 30
– Pre-conception and pre-natal period
A given individual’s mental health and wellbeing can be influenced by factors present prior to conception or birth. Pregnancies which are unwanted or in adolescence can increase the likelihood of detrimental behaviours of the mother during pregnancy, and the environmental or family conditions of childhood. 31
During pregnancy, detrimental behaviours including tobacco, alcohol and drug use can increase the likelihood of later mental health disorders for children; malnutrition, low-birth weight and micronutrient deficiency (for example, iodine deficiency) can also influence later mental health vulnerabilities. 32
– Infancy and early childhood
There is a large base of evidence which shows that emotional attachment in early childhood has a considerable impact on later vulnerability to mental health and wellbeing. 33 As a result, particular risk factors include separation from the primary caregiver, in some cases post-natal depression in mothers (which can result in sub-optimal attachment), and parents for whom communication and social interaction is challenging. Child maltreatment and neglect has been found to have a significant impact on vulnerabilities to mental wellbeing. 34 Malnutrition, poor access to basic services and disease and parasites are also important contributors.
– Childhood
Childhood conditions form a critical component of health and wellbeing later in life. Negative experiences, either at home or outside of the home (for example, bullying in school) can have lifelong impacts on the development of core cognitive and emotional skills. Poor socioeconomic conditions also have a significant effect on vulnerability to mental health disorders; in a study in Sweden, the authors found that children raised in families of poor socioeconomic backgrounds had an increased risk of psychosis. 35
Poor economic resources, shown through poor housing conditions for example, can be seen by children as shameful or degrading and affect aspects of childhood learning, communication and interaction with peers.
Children with a parent who has a mental illness or substance use disorder have a higher risk of psychiatric problems themselves. 36 This effect between generations can occur as a result of genetic, biological, psychological and social risk factors.
– Adolescence
Adolescence is typically the stage of life where mental health disorders tend to become more apparent. The risk factors and contributors to wellbeing in childhood apply equally to those in adolescence. In addition, several other contributing factors appear. It is in the years of adolescence that the use of substances including alcohol and drugs first appear.
Substance use is particularly hazardous and harmful for adolescents because individuals are still developing both mentally and physically. Peer pressure, and media influences also become more prominent over these years. Exposure to substance use is not only an important risk factor for other mental health disorders, but also linked to poorer educational outcomes, more risky sexual behaviour and increased exposure to violence and conflict.
– Adulthood
Experiences and emotional capabilities developed through childhood and adolescence are important factors in the effect that particular events and scenarios in adulthood have on mental health outcomes.
The WHO highlight that critical to wellbeing in adulthood is the allocation and balance between work and leisure time. Exposure to high stress and anxiety is strongly influenced by the share of time working, caring for others, or time spent in an insecure economic environment. Individuals with poor socioeconomic security, and in particular unemployment, are also at higher risk to mental health disorders.
These factors, balanced with the amount of time spent on ‘consumption’ activities, including leisure time and supportive family and friends, often determine the propensity for poor mental health and wellbeing. Community structures can have a significant positive impact on these outcomes — individuals who have poor access to such communities, either through social exclusion, neighbourhood violence/crime, or lack of respite care have a higher risk of mental health disorders.
Physical health also has an important impact on mental wellbeing; an individual’s ‘physical capital’ can influence their sense of esteem and social inclusion. Individuals with chronic illness or disability are at higher risk of poor mental health; this is particularly true for conditions with high rates of stigmatisation, such as HIV/AIDS.
– Older age
Individuals of older age are of notably high risk of poorer mental health and wellbeing. This typically results from notable changes in life conditions (such as a cease in employment which affects both the feeling of contribution and economic freedom), higher social exclusion, and loneliness. This is particularly true when an older individual begins to lose close family and friends. Bereavement in general is an important predictor of mental health disorders such as depression.
A decline in physical health can have major impacts on life capabilities by affecting an individual’s mobility and freedom. Older individuals are also at higher risk of abuse or neglect from carers and in some cases, family members.
Link between mental health and suicide
The link between mental health and substance use disorders and suicide is well-documented. 37 It is however true that not all suicides – or suicide attempts – are attributed to underlying mental health or substance use disorders; as shown in the chart, there is not a direct relationship between mental health prevalence and suicide rates. 38
We cover suicide statistics more broadly in our full entry on Suicide, however here we attempt to distil the key findings on the links between mental health and substance use and suicide. Although mental health and substance use disorders is within the top-five causes of disease burden globally (as measured by Disability-Adjusted Life Years; DALYs), accounting for approximately 7 percent of the burden, several authors have highlighted that such figures — since they do not include suicide DALYs — underestimate the true cost of mental health disorders. 39
Providing a more accurate estimate of total mental health burden therefore requires some understanding of the connection between these disorders and suicide.
Meta-analyses of psychological autopsy studies of suicide across high-income countries suggest that up to 90 percent of suicides occur as a result of an underlying mental health or substance use disorder. 40
While available data and studies are more scarce across lower-to-middle income countries, evidence across countries including China, Taiwan and India suggest that this proportion is significantly lower elsewhere. 41
These studies suggest a large number of suicides resultant from the ‘dysphoric affect’ and ‘impulsivity’ (which are not defined as a mental and substance use disorder). In such cases, understanding the nature of self-harm methods between countries is important; in these countries a high percentage of self-harming behaviours are carried out through more lethal methods such as poisoning (often through pesticides) and self-immolation. This means that in a high number of cases self-harming behaviours can prove fatal, even if there was not a clear intent to die.
A study by Ferrari et al. (2015) attempted to determine the share disease burden from suicide which could be attributed to mental health or substance use disorders. 42
Based on review across a number of meta-analysis studies the authors estimated that 68 percent of suicides across China, Taiwan and India were attributed to mental health and substance use disorders; across other countries this share was approximately 85 percent. In their estimates of total attributable disease burden, the authors concluded that mental health and substance use disorders were responsible for 62 percent of total DALYs from suicide.
Weight-for-age
Charts
z-scores: girls
z-scores: boys
Percentiles: girls
Percentiles: boys
Tables
z-scores: girls
Girls table- Weight-for-age: Birth to 13 weeks (z-scores)
Download: PDF ǀ Excel
Girls table- Weight-for-age: Birth to 5 years (z-scores)
Download: PDF ǀ Excel
z-scores: boys
Boys table- Weight-for-age: Birth to 13 weeks (z-scores)
Download: PDF ǀ Excel
Boys table- Weight-for-age: Birth to 5 years (z-scores)
Download: PDF ǀ Excel
Percentiles: girls
Girls table- Weight-for-age: Birth to 13 weeks (percentiles)
Download: PDF ǀ Excel
Girls table- Weight-for-age: Birth to 5 years (percentiles)
Download: PDF ǀ Excel
Percentiles: boys
Boys table- Weight-for-age: Birth to 13 weeks (percentiles)
Download: PDF ǀ Excel
Boys table- Weight-for-age: Birth to 5 years (percentiles)
Download: PDF ǀ Excel
Agents Classified by the IARC Monographs, Volumes 1–132
| Group 1 | Carcinogenic to humans | 122 agents |
|---|---|---|
| Group 2A | Probably carcinogenic to humans | 93 agents |
| Group 2B | Possibly carcinogenic to humans | 319 agents |
| Group 3 | Not classifiable as to its carcinogenicity to humans | 501 agents |
For definitions of these groups, please see the Preamble.
It is strongly recommended to consult the complete Monographs on these agents, the publication date, and the list of studies considered. Significant new information might support a different classification.
For agents that have not been classified, no determination of non-carcinogenicity or overall safety should be inferred.
Read the IARC Monographs Q&A for answers to commonly asked questions on the evaluation process.
Although care was taken in preparing these lists, mistakes may be present.
Obesity
Obesity is most commonly measured using the body mass index (BMI) scale. The World Health Organization define BMI as: “ a simple index of weight-for-height that is commonly used to classify underweight, overweight and obesity in adults.” 1
BMI values are used to define whether an individual is considered to be underweight, healthy, overweight or obese. The WHO defines these categories using the cut-off points: an individual with a BMI between 25.0 and 30.0 is considered to be ‘overweight’; a BMI greater than 30.0 is defined as ‘obese’. 2
Summary
Related research entries
Food per person – food availability has increased significantly in most countries across the world. How does the supply of calories, protein and fats vary between countries? How has this changed over time?
Hunger and Undernourishment – obesity rates have now overtaken hunger rates globally. But it remains the case that high levels of obesity and hunger can occur in a country at any given time. How does undernourishment vary across the world? How has it changed over time?
Micronutrient Deficiency – getting sufficient intake of calories (a requirement for obesity) does not guarantee an individual gets the full range of essential vitamins and minerals (micronutrients) for good health. Dietary diversity varies significantly across the world. How common is micronutrient deficiency and who is most at risk?
Obesity is one of the leading risk factors for early death
Obesity is responsible for 4.7 million premature deaths each year
Obesity is one of the world’s largest health problems – one that has shifted from being a problem in rich countries, to one that spans all income levels.
The Global Burden of Disease is a major global study on the causes and risk factors for death and disease published in the medical journal The Lancet. 3 These estimates of the annual number of deaths attributed to a wide range of risk factors are shown here. This chart is shown for the global total, but can be explored for any country or region using the “change country” toggle.
Obesity – defined as having a high body-mass index – is a risk factor for several of the world’s leading causes of death, including heart disease, stroke, diabetes and various types of cancer. 4 Obesity does not directly cause of any of these health impacts but can increase their likelihood of occurring. In the chart we see that it is one of the leading risk factors for death globally.
According to the Global Burden of Disease study 4.7 million people died prematurely in 2017 as a result of obesity. To put this into context: this was close to four times the number that died in road accidents, and close to five times the number that died from HIV/AIDS in 2017. 5
Click to open interactive version
The global distribution of health impacts from obesity
8% of global deaths are the result of obesity
Globally, 8% of deaths in 2017 were the result of obesity – this represents an increase from 4.5% in 1990.
This share varies significantly across the world. In the map here we see the share of deaths attributed to obesity across countries.
Across many middle-income countries – particularly across Eastern Europe, Central Asia, North Africa, and Latin America – more than 15% of deaths were attributed to obesity in 2017. This most likely results from having a high prevalence of obesity, but poorer overall health and healthcare systems relatively to high-income countries with similarly high levels of obesity.
In most high-income countries this share is in the range of 8 to 10%. This is about half the share of many middle-income countries. The large outliers among rich countries are Japan and South Korea: there only around 5% of premature deaths are attributed to obesity.
Across low-income countries – especially across Sub-Saharan Africa – obesity accounts for less than 5% of deaths.
Click to open interactive version
There is a 10-fold difference in death rates from obesity across the world
Death rates from obesity give us an accurate comparison of differences in its mortality impacts between countries and over time. In contrast to the share of deaths that we studied before, death rates are not influenced by how other causes or risk factors for death are changing.
In the map here we see differences in death rates from obesity across the world. Globally, the death rate from obesity was around 60 per 100,000 in 2017.
The overall picture does in fact match closely with the share of deaths: death rates are high across middle-income countries, especially across Eastern Europe, Central Asia, North Africa and Latin America. Rates there can be close to 200 per 100,000. This is more than ten times greater than rates at the bottom: Japan and South Korea have the lowest rates in the world at 14 and 20 deaths per 100,000, respectively.
When we look at the relationship between death rates and the prevalence of obesity we find a positive one: death rates tend to be higher in countries where more people have obesity. But what we also notice is that for a given prevalence of obesity, death rates can vary by a factor of four. 23% of Russian and Norwegian are obese, yet Russia’s death rate is four times higher. Clearly it’s not only the prevalence of obesity that plays a role but also other factors such as underlying health, other confounding risk factors (such as alcohol, drugs, smoking and other lifestyle factors) and healthcare systems.
Click to open interactive version
What share of adults are obese?
13% of adults in the world are obese
Globally, 13% of adults aged 18 years and older were obese in 2016. 6 Obesity is defined as having a body-mass index equal to or greater than 30.
In the map here we see the share of adults who are obese across countries. Overall we see a pattern roughly in line with prosperity: the prevalence of obesity tends to be higher in richer countries across Europe, North America, and Oceania. Obesity rates are much lower across South Asia and Sub-Saharan Africa.
More than one-in-three (36%) of adults in the United States were obese in 2016. In India this share was around 10 times lower (3.9%).
The relationship between income and obesity generally holds true – as we see in the comparison here. But there are some notable exceptions. The small Pacific Island States stand out clearly: they have very high rates of obesity – 61% in Nauru and 55% in Palau – for their level of income. At the other end of the spectrum, Japan, South Korea and Singapore have very low levels of obesity for their level of income.
Related charts – share of men and women that are obese. This map allows you to explore the share of men that are obese; this map allows you to explore this data for women across the world. This chart shows the comparison of obesity in men and women.
Click to open interactive version
What share of adults are overweight?
39% of adults in the world are overweight or obese
Globally, 39% of adults aged 18 years and older were overweight or obese in 2016. 7 Being overweight is also defined based on body-mass index: the threshold value is lower than for obesity, with a BMI equal to or greater than 25.
In the map here we see the share of adults who are overweight or obese across countries. The overall pattern is very closely aligned with the distribution of obesity across the world: the share of people who are overweight tends to be higher in richer countries and lower at lower incomes. What is of course true is that the share who are overweight (have a BMI greater than or equal to 25) is much higher than the share that are obese (a BMI of 30 or greater).
In most high-income countries, around two-thirds of adults are overweight or obese. In the US, 70% are. At the lowest end of the scale, across South Asia and Sub-Saharan Africa around 1-in-5 adults have a BMI greater than 25.
Related charts – share of men and women that are overweight or obese. This map allows you to explore the share of men that are overweight or obese; this map allows you to explore this data for women across the world.
Click to open interactive version
Body Mass Index (BMI)
Mean BMI in adult women
Body Mass Index (BMI) is used to define the share of individuals that are underweight, in the ‘healthy’ range, overweight and obese.
In the map here we see the distribution of mean BMI for adult women – aged 18 years and older – across the world. The global mean BMI for women in 2016 was 25 – just on the threshold from the WHO’s ‘healthy’ to ‘overweight’ classification. This has increased from a mean BMI of 22 – in the mid-range of ‘healthy’ – in the 1970s.
Click to open interactive version
Mean BMI in adult men
Body Mass Index (BMI) is used to define the share of individuals that are underweight, in the ‘healthy’ range, overweight and obese.
In the map here we see the distribution of mean BMI for adult men – aged 18 years and older – across the world. The global mean BMI for men in 2016 was 24.5 – just on the threshold from the WHO’s ‘healthy’ to ‘overweight’ classification. This has increased from a mean BMI of 21.7 – in the mid-range of ‘healthy’ – in the 1970s.
Click to open interactive version
Childhood obesity
Share of children that are overweight
Obesity and overweight in children are also measured on the basis of body-mass-index (BMI). However, interpretation of BMI scores is treated differently for children and adolescents. Weight categories are defined in relation to WHO Growth Standards – a child is defined as overweight if their weight-for-height is more than two standard deviations from the median of the WHO Child Growth Standards.
The World Health Organization reports that the share of children and adolescents aged 5-19 who are overweight or obese has risen from 4% in 1975 to around 18% in 2016. 8
In the map here we see the share of very young children – aged 2 to 4 years old – who are overweight based on WHO Child Growth Standards. In many countries as many as every third or fourth child is overweight.
Click to open interactive version
What are the drivers of obesity?
At a basic level, weight gain – eventually leading to being overweight or obesity – is determined by a balance of energy. 9 When we consume more energy – typically measured in kilocalories – than the energy expended to maintain life and carry out daily activites, we gain weight. This is a called an energy surplus. When we consume less energy than we expend, we lose weight – this is an energy deficit.
This means there are two potential drivers of the increase in obesity rates in recent decades: either an increase in kilocalorie intake i.e. we eat more; or we expend less energy in daily life through lower activity levels. Both elements are likely to play a role in the rise in obesity.
To tackle obesity it’s likely that interventions which address both components: energy intake and expenditure are necessary. 10
Daily supply of calories
Over the past century – but particularly over the past 50 years – the supply of calories has increased across the world. In the 1960s, the global average supply of calories (that is, the availability of calories for consumers to eat) was 2200kcal per person per day. By 2013 this had increased to 2800kcal.
Across most countries, energy consumption has therefore increased. If this increase was not met with an increase in energy expenditure, weight gain and a rise in obesity rates is the result.
In the chart here we see the relationship between the share of men that are overweight or obese (on the y-axis) versus the daily average supply of kilocalories per person. Overall we see a strong positive relationship: countries with higher rates of overweight tend to have a higher supply of calories.
If you press ‘play’ on the interactive timeline you can see how this has changed for each country over time. Most countries move upwards and to the right: the supply of calories has increased at the same time as obesity rates have increased.
Click to open interactive version
Definitions & Measurement
How do we measure obesity in adults?
The most common metric used for assessing the prevalence of obesity is the body mass index (BMI) scale. The World Health Organization define BMI as: “ a simple index of weight-for-height that is commonly used to classify underweight, overweight and obesity in adults. It is defined as the weight in kilograms divided by the square of the height in metres (kg/m 2 ). For example, an adult who weighs 70kg and whose height is 1.75m will have a BMI of 22.9.” 11
Measured BMI values are used to define whether an individual is considered to be underweight, healthy, overweight or obese. The WHO defines these categories using the cut-off points in the table. For example, an individual with a BMI between 25.0 and 30.0 is considered to be ‘overweight’; a BMI greater than 30.0 is defined as ‘obese’. 12
How do we measure obesity in children and adolescents?
Is BMI an appropriate measure of weight-related health?
The merits of using BMI as an indicator of body fat and obesity are still contested. A key contention to the use of BMI indicators is that it provides a measure of body mass/weight rather than providing a direct measure of body fat. Whilst physicians continue to use BMI as a general indicator of weight-related health risks, there are some cases where its use should be considered more carefully 14 :
Physicians must therefore evaluate BMI results carefully on a individual basis. Despite outlier cases where BMI is an inappropriate indicator of body fat, its use provides a reasonable measure of the risk of weight-related health factors across most individuals across the general population.
World Health Organisation (WHO)
WHO works in close cooperation with the European Union on health promotion and healthy ageing. The Global Network of Age-friendly Cities and Communities (GNAFCC) was established to foster the exchange of experience and mutual learning between cities and communities worldwide. Any city or community that is committed to creating inclusive and accessible urban environments to benefit their ageing populations is welcome to join. GNAFCC helps cities and communities support active and healthy ageing by better addressing older people’s needs across eight dimensions: the built environment, transport, housing, social participation, respect and social inclusion, civic participation and employment, communication, and community support and health services. AGE is a GNAFCC institutional affiliate and we are working collaboratively to promote age-friendly environments at the EU level. In the frame of the European Year 2012 AGE and its partners call on the European Commission to launch an EU Covenant of Mayors on Demographic Change that will seek to create the political framework to bring together local and regional authorities across the EU who want to find smart and innovative solutions to support active and healthy ageing and develop age-friendly environments.
WHO Europe network of Healthy Cities is another useful initiative that engages local governments in health development through a process of political commitment, institutional change, capacity-building, partnership-based planning and innovative projects. About 90 cities are members of the WHO European Healthy Cities Network, and 30 national Healthy Cities networks across the WHO European Region have more than 1400 cities and towns as members.
You can encourage your local authorities to become more age-friendly and to join the Global Network of Age-Friendly Cities and Communities and/or the Healthy Cities network. You can also encourage them to support the call for a European Covenant of Mayors on Demographic Change and to join this movement when it will be launched. If you wish to be kept informed of the latest developments at EU level, register on the EU virtual network on age-friendly environments set up by AGE (link available on AGE homepage).
Blindness and vision impairment
Key facts
Definitions
The International Classification of Diseases 11 (2018) classifies vision impairment into two groups, distance and near presenting vision impairment.
Distance vision impairment:
Near vision impairment:
Prevalence
Globally, at least 2.2 billion people have a near or distance vision impairment. In at least 1 billion – or almost half – of these cases, vision impairment could have been prevented or has yet to be addressed.
This 1 billion people includes those with moderate or severe distance vision impairment or blindness due to unaddressed refractive error (88.4 million), cataract (94 million), glaucoma (7.7 million), corneal opacities (4.2 million), diabetic retinopathy (3.9 million), and trachoma (2 million), as well as near vision impairment caused by unaddressed presbyopia (826 million) (1).
In terms of regional differences, the prevalence of distance vision impairment in low- and middle-income regions is estimated to be four times higher than in high-income regions (1). With regards to near vision, rates of unaddressed near vision impairment are estimated to be greater than 80% in western, eastern and central sub-Saharan Africa, while comparative rates in high-income regions of North America, Australasia, Western Europe, and of Asia-Pacific are reported to be lower than 10% (2).
Population growth and ageing are expected to increase the risk that more people acquire vision impairment.
Causes
Globally, the leading causes of vision impairment are:
There is substantial variation in the causes between and within countries according to the availability of eye care services, their affordability, and the eye care literacy of the population. For example, the proportion of vision impairment attributable to cataract is higher in low- and middle-income countries than high-income countries. In high income countries, diseases such as glaucoma and age-related macular degeneration are more common.
Among children, the causes of vision impairment vary considerably across countries. For example, in low-income countries congenital cataract is a leading cause, whereas in middle-income countries it is more likely to be retinopathy of prematurity. As in adult populations, uncorrected refractive error remains a leading cause of vision impairment in all countries amongst children.
Impact of vision impairment
Personal impact
Young children with early onset severe vision impairment can experience delayed motor, language, emotional, social and cognitive development, with lifelong consequences. School-age children with vision impairment can also experience lower levels of educational achievement.
Vision impairment severely impacts quality of life among adult populations. Adults with vision impairment often have lower rates of workforce participation and productivity and higher rates of depression and anxiety. In the case of older adults, vision impairment can contribute to social isolation, difficulty walking, a higher risk of falls and fractures, and a greater likelihood of early entry into nursing or care homes.
Economic impact
Vision impairment poses an enormous global financial burden. For example, the annual global costs of productivity losses associated with vision impairment from uncorrected myopia and presbyopia alone were estimated to be US$ 244 billion and US$ 25.4 billion, respectively.
Strategies to address eye conditions to avoid vision impairment
While a large number of eye diseases can be prevented (e.g. infections, trauma, unsafe traditional medicines, perinatal diseases, nutrition-related diseases, unsafe use or self-administration of topical treatment), this is not possible for all.
Each eye condition requires a different, timely response. There are effective interventions covering promotion, prevention, treatment and rehabilitation which address the needs associated with eye conditions and vision impairment; some are among the most cost-effective and feasible of all health care interventions to implement. For example, uncorrected refractive error can be corrected with spectacles or surgery while cataract surgery can restore vision.
Treatment is also available for many eye conditions that do not typically cause vision impairment, such as dry eye, conjunctivitis and blepharitis, but generate discomfort and pain. Treatment of these conditions is directed at alleviating the symptoms and preventing the evolution towards more severe diseases.
Vision rehabilitation is very effective in improving functioning for people with an irreversible vision impairment that can be caused by eye conditions such as diabetic retinopathy, glaucoma, consequences of trauma and age-related macular degeneration.
WHO response
WHO’s work is guided by the recommendations of the WHO World report on vision (2019) and the resolution on «integrated, people-centred eye care, including preventable blindness and vision impairment» that was adopted at 73rd World Health Assembly in 2020. The key proposal of the report and resolution is to make integrated people-centred eye care (IPEC) the care model of choice and to ensure its widespread implementation. It is expected that by shaping the global agenda on vision, the report and resolution will assist Member States and their partners in their efforts to reduce the burden of eye conditions and vision impairment and achieve the Sustainable Development Goals (SDGs), particularly SDG target 3.8 on universal health coverage.
Some of WHO’s key areas of work and activities in the prevention of blindness include:
References
1) Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years: evaluating the prevalence of avoidable blindness in relation to “VISION 2020: the Right to Sight”. Lancet Global Health 2020. doi.org/10.1016/S2214-109X(20)30489-7
2) Vision Loss Expert Group of the Global Burden of Disease Study. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet Global Health 2020. doi: 10.1016/S2214-109X(20)30425-3
3) Fricke, TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Suit MH, Naduvilath T, Naidoo K, Global Prevalence of Presbyopia and Vision Impairment from Uncorrected Presbyopia: Systematic Review, Meta-analysis, and Modelling, Ophthalmology. 2018 May 9
The World report on ageing and health: a policy framework for healthy ageing
Affiliations
The World report on ageing and health: a policy framework for healthy ageing
Authors
Affiliations
Abstract
Although populations around the world are rapidly ageing, evidence that increasing longevity is being accompanied by an extended period of good health is scarce. A coherent and focused public health response that spans multiple sectors and stakeholders is urgently needed. To guide this global response, WHO has released the first World report on ageing and health, reviewing current knowledge and gaps and providing a public health framework for action. The report is built around a redefinition of healthy ageing that centres on the notion of functional ability: the combination of the intrinsic capacity of the individual, relevant environmental characteristics, and the interactions between the individual and these characteristics. This Health Policy highlights key findings and recommendations from the report.
Copyright © 2016 World Health Organization. Published by Elsevier Ltd/Inc/BV. All rights reserved. Published by Elsevier Ltd.. All rights reserved.
Figures
Figure 1. Mortality at different ages for…
Figure 1. Mortality at different ages for countries of low, middle, and high income, 2012
Years of life lost per…
Years of life lost per 100 000 population, 2012 Top ten causes in…
Range and mean intrinsic capacity…
Range and mean intrinsic capacity of men and women in countries in the…
Physical functioning across the life…
Physical functioning across the life course, stratified by ability to manage on current…
A public health framework for…
A public health framework for healthy ageing
Применение международной классификации функционирования, ограничений жизнедеятельности и здоровья для оценки реабилитации больных сердечно-сосудистыми заболеваниями
А.К. НУРГАЗИЗОВА, В.В. СЕРГЕЕВА, А.Ю. РОДИОНОВА
Санкт-Петербургский институт усовершенствования врачей-экспертов Министерства труда и социальной защиты Российской Федерации, 194044, г. Санкт-Петербург, Большой Сампсониевский пр., д. 11/12
Нургазизова Альбина Камильевна — аспирант кафедры терапии, МСЭ и реабилитации № 2, тел. +7-931-247-32-98, e-mail: miledinyr@yandex.ru
Сергеева Вера Владимировна — доктор медицинских наук, профессор кафедры терапии, МСЭ и реабилитации № 2, тел. +7-921- 992- 22-35, e-mail: vera.sergeeva.208@mail.ru
Родионова Анна Юрьевна — кандидат медицинских наук, ассистент кафедры терапии, МСЭ и реабилитации № 2, тел. +7-921-563-98-93, e-mail: rodionova.aniuta@yandex.ru
В статье рассмотрена одна из классификаций Всемирной организации здравоохранения — Международная классификация функционирования, ограничений жизнедеятельности и здоровья. Показана связь с Международной классификацией болезней 10-го пересмотра. Приведены определения, которые используются в классификации, а также специалисты, которые могут использовать данный инструмент в своей работе. Рассмотрены такие домены, как функции, структуры организма, активность и участие, а также факторы окружающей среды. Приведены буквенное обозначение доменов и их числовая оценка. Показана возможность не только качественной оценки нарушенных функций, но и количественной, выраженной в процентах. На примере больных с сердечно-сосудистой патологией показана широта оценки нарушенных функций и возможность ее использования в динамике для оценки эффективности проводимой реабилитации.
Ключевые слова: Международная классификация функционирования, ограничений жизнедеятельности и здоровья, домен, функции организма.
A.K. NURGAZIZOVA, V.V. SERGEYEVA, A.Yu. RODIONOVA
Saint Petersburg Institute of Expert Doctors Improvement of the Ministry of Labor and Social Protection of the Russian Federation, 11/12 Bolshoy Sampsoniyevskiy Prospekt, Saint-Petersburg, Russian Federation 194044
Implementation of the international classification of functioning, disabilities and health for the assessment of rehabilitation of patients with cardiovascular diseases
Nurgazizova A.K. — postgraduate student of the Department of Therapy, Medical Social Expertise and Rehabilitation № 2, tel. +7-931-247-32-98, e-mail: miledinyr@yandex.ru
Sergeyeva V.V. — D. Med. Sc., Professor of the Department of Therapy, Medical Social Expertise and Rehabilitation № 2, tel. +7-921- 992- 22-35, e-mail: vera.sergeeva.208@mail.ru
Rodionova A.Yu. — Cand. Med. Sc., Assistant Lecturer of the Department of Therapy, Medical Social Expertise and Rehabilitation № 2, tel. +7-921-563-98-93, e-mail: rodionova.aniuta@yandex.ru
The article considers one of the classifications of the world health organization – the international classification of functioning, disabilities and health. It shows the relationship with the International classification of diseases, 10th revision. The definitions used in the classification are listed, as well as specialists who can use the scale in their work. Such domain functions are reviewed, as functions and structures of the organism, activity and participation, as well as environmental factors. The domains codes and their numerical evaluation are given. The opportunity of not only qualitative, but also quantitative (percentage) evaluation of disturbed functions is proved. For example, the wide range of damaged functions can be described for the patients with a cardiovascular pathology, thus giving the opportunity to use it in dynamics to assess the rehabilitation effectiveness.
Key words: international classification of functioning, disabilities and health, domain, functions of the body.
Международная классификация функционирования, ограничений жизнедеятельности и здоровья (МКФ) принадлежит к семье международных классификаций. Она представляет собой ценный инструмент, позволяющий на международном уровне описывать и сравнивать популяционные данные о здоровье. В Международных классификациях Всемирной организации здравоохранения изменения здоровья (болезнь, расстройство, травма и т.п.) изначально классифицированы в Международной классификации болезней 10-го пересмотра (МКБ-10), которая определяет их этиологическую структуру. Функционирование и ограничения жизнедеятельности, связанные с изменениями здоровья, классифицируются в МКФ. Поскольку, МКБ-10 и МКФ дополняют друг друга, пользователям рекомендуется применять обе классификации одновременно [1, 13]. Совместная информация, относящаяся к диагнозу и функционированию, дает более широкую и значимую картину здоровья людей или популяции, которая может быть использована при принятии решений [2]. Каждая из классификаций имеет свою целевую аудиторию. МКБ-10 предназначена главным образом для врачей первичного звена медицинской помощи. МКФ — для всех специалистов, работающих или задействованных в сфере реабилитации: врачей, психологов, терапевтов, педагогов, экономистов, юристов, политиков и т.д. [3].
Всеобъемлющая цель МКФ — обеспечить унифицированным стандартным языком и определить рамки для описания показателей здоровья и показателей, связанных со здоровьем [1, 4, 12]. Она вводит определения составляющих здоровья и некоторых, связанных со здоровьем, составляющих благополучия (таких как образование и труд). Таким образом, домены, имеющиеся в МКФ, могут рассматриваться как домены здоровья и как домены, связанные со здоровьем. Эти домены описаны с позиции организма, индивида и общества посредством двух основных перечней: 1. функции и структуры организма; 2. активность и участие.
Информация в МКФ систематизирована в двух частях. Часть 1 включает в себя функционирование и ограничение жизнедеятельности, 2-я часть охватывает контекстовые факторы. Каждая часть включает две составляющие: 1. Составляющие функционирования и ограничения жизнедеятельности. Составляющая организм включает две классификации, одна для функций систем организма, другая для структур организма. Разделы в обеих классификациях построены в соответствии с системами организма. Составляющая активность и участие охватывает полный круг доменов, обозначающих аспекты функционирования с индивидуальной и социальной позиций. 2. Составляющие контекстовых факторов. Перечень окружающих факторов — это первая составляющая контекстовых факторов. Окружающие факторы влияют на все составляющие функционирования и ограничений жизнедеятельности и систематизированы по принципу: от непосредственно окружающих индивида до общего окружения. Личностные факторы являются составляющей факторов контекста, но они не классифицированы в МКФ из-за больших социальных и культурных вариаций, связанных с ними [4, 5].
Международная классификация функционирования построена на основе следующих важных принципов: универсальность, утилитарность, нейтральность, достоверность, валидность, сопоставимость, акцент на позитивных аспектах, взаимодействие с факторами окружающей среды, интерактивность. В соответствии с данными принципами данная классификация может быть применима ко всем людям, независимо от состояния здоровья или возраста. Показатели здоровья и показатели, связанные со здоровьем, при любом изменении здоровья могут быть описаны с помощью МКФ [3, 11].
МКФ не классифицирует людей, а дает описание ситуаций, исходя из функционирования и его ограничений у человека, поэтому служит своеобразным каркасом для систематизации этой информации, основываясь на взаимодействии характеристик здоровья и контекстовых факторов, которые приводят к ограничениям жизнедеятельности. МКФ выстраивает информацию во взаимосвязанном и легко понятном виде [6, 1, 7].
МКФ использует буквенно-цифровую систему, в которой буквы b, s, d, е используются для обозначения функций (b) и структур (s) организма, активности и участия (d) и факторов окружающей среды (е). За этими буквами следует числовой код.
К соответствующему домену классификации при оценке нарушенных функций, структур организма и категорий активности и участия подбирается вариант количественной оценки:
xxx.0 НЕТ проблем (никаких, отсутствуют, ничтожные…) 0-4%
xxx.1 ЛЕГКИЕ проблемы (незначительные, слабые,…) 5-24%
xxx.2 УМЕРЕННЫЕ проблемы (средние, значимые,…) 25-49%
xxx.3 ТЯЖЕЛЫЕ проблемы (высокие, интенсивные…) 50-95%
xxx.4 АБСОЛЮТНЫЕ проблемы (полные…) 96-100%
xxx.8 не определено
xxx.9 не применимо [5, 8, 4, 9, 10].
Для оценки факторов окружающей среды МКФ предлагает общий определитель с негативной и позитивной шкалами, обозначающими степень выраженности конкретного фактора в виде барьера или облегчения, при этом точка указывает на барьеры, а знак (+) указывает на облегчающие факторы [10]:
xxx.0 НЕТ барьеров (никаких, отсутствуют, ничтожные…) 0-4%
xxx.1 НЕЗНАЧИТЕЛЬНЫЕ барьеры (легкие, небольшие, слабые) 5-24%
xxx.2 УМЕРЕННЫЕ барьеры (средние) 25-49%
xxx.3 ВЫРАЖЕННЫЕ барьеры (резко выраженные, тяжелые) 50-95%
xxx.4 АБСОЛЮТНЫЕ барьеры (полные…) 96-100%
xxx+0 НЕТ облегчающих факторов (отсутствуют, ничтожные) 0-4%
xxx+1 НЕЗНАЧИТЕЛЬНЫЕ облегчающие факторы (легкие, небольшие, слабые) 5-24%
ххх+2 УМЕРЕННЫЕ облегчающие факторы (средние) 25-49%
ххх+3 ВЫРАЖЕННЫЕ облегчающие факторы (резко выраженные, значимые…) 50-95%
ххх+4 АБСОЛЮТНЫЕ облегчающие факторы (полные) 96-100%
Ниже приведено 2 примера больных с сердечно-сосудистыми заболеваниями.
Больной Л., 55 лет. Клинический диагноз:
Основной: Гипертоническая болезнь II стадии, артериальная гипертензия 2-й ст., риск сердечно-сосудистых осложнений 3.
Сопутствующий: сахарный диабет 2-го типа, компенсирован диетой. Ожирение II степени.
Основная профессия: менеджер по продажам.
Больной М., 58 лет. Клинический диагноз:
Основной: ИБС. Стенокардия напряжения III ФК. Атеросклеротический кардиосклероз. Постинфарктный кардиосклероз (ОИМ от 2010 г.). Гипертоническая болезнь III стадии, артериальная гипертензия 3-й ст., риск сердечно-сосудистых осложнений 4.
Осложнение основного заболевания: Хроническая сердечная недостаточность II А ст. (II ФК по NYHA).
Сопутствующий: ЦВБ. Дисциркуляторная энцефалопатия II ст. МКБ. Микролиты почек. Хронический пиелонефрит, латентное течение. ХБП II ст. ХПН 0 ст.
Основная профессия: электрик.
Оценка нарушенных функций с помощью МКФ при первичном обращении больных в бюро медико-социальной экспертизы (бюро МСЭ) представлена в табл. 1.
Таблица 1.
Оценка нарушенных функций с помощью МКФ на примере больных М. и Л.
| Нарушенные функции | Больной М., 58 лет | Больной Л., 55 лет |
| Умственные функции (b 110-b 180) | b 1400.1 — легкое снижение устойчивости внимания b 1401.1 — легкое нарушение переключения внимания b 1441.1 — легкое нарушение долговременной памяти b 1442.1 — легкое нарушение воспроизведения, хранящегося в памяти b 1643.1 — легкое нарушение познавательной гибкости | b 1341.1 — легкое нарушение начала сна b1343.1 — легкое нарушение качества сна b1520.1 — легкое нарушение адекватности эмоций |
| Сенсорные функции и боль (b 210-b 280) | b 2351.2 — нарушение вестибулярной равновесия b 2401.2 — умеренное нарушение, связанное с появлением головокружения b 2400.2 — умеренное нарушение, связанное с ощущением звона или шума в ушах b 28010.3 — выраженное нарушение, связанное с ощущением боли в голове и шее b 28011.2 — умеренное нарушение, связанное с ощущением боли в грудной клетке b 2803.2 — умеренное нарушение, связанное с ощущением иррадиирущей боли в дерматоме | b 28010.2 — умеренная боль в голове и шее |
| Функции голоса и речи (b 310-b 340) | не нарушены | не нарушены |
| Функции сердечно-сосудистой, крови, иммунной и дыхательной систем (b 410-b 460) | b 4102.2 — умеренные нарушения сократительной силы миокарда b 4103.2 — умеренные нарушения кровоснабжения сердца b 4150.2 — умеренные нарушения функции артерий b 4152.1 — легкие нарушения функции вен b 4200.3 — выраженное повышение артериального давления b 4202.3 — выраженное нарушение поддержания артериального давления b 4400.2 — умеренные нарушения темпа дыхания b 4550.2 — умеренные нарушения общей физической выносливости b 4551.2 — умеренные нарушения аэробного резерва b 4552.2 — умеренное чувство утомляемости. b 460.1 — легкие нарушения ощущений, связанных с функционированием сердечно-сосудистой и дыхательной систем. | b 4150.2 — умеренное нарушение функции артерий b 4200.2 — умеренное повышение артериального давления b 4550.2 — умеренное нарушение общей физической выносливости b 4552.2 — умеренная утомляемость |
| Функции пищеварительной, эндокринной систем и метаболизма (b 510-b 555) | не нарушены | b 5401.1 — легкое нарушение углеводного обмена b 5403.2 — умеренное нарушение обмена жиров |
| Урогенитальные и репродуктивные функции (b 610-b 670) | b 6100.1 — легкие нарушения фильтрации | не нарушены |
| Нейромышечные, скелетные и связанные с движением функции (b 710-b 780) | не нарушены | не нарушены |
| Функции кожи и связанных с ней структур (b 810-b 860) | не нарушены | не нарушены |
Как видно из представленной таблицы, несмотря на наличие у обоих больных сердечно-сосудистых заболеваний, МКФ позволяет показать разницу как нарушенных функций, так и их выраженности. При оценке нарушенных функций в процентном соотношении у больного М. колебались в пределах от 0 до 85%, а у больного Л. — от 0 до 44%.
В табл. 2 представлена оценка нарушенных структур организма на примере больного М. и больного Л.
Таблица 2.
Оценка нарушенных структур с помощью МКФ на примере больных М. и Л.
| Нарушенные структуры | Больной М., 58 лет | Больной Л., 55 лет |
| Структуры нервной системы (s 110-s 150) | s 1000.1 — легкое нарушение структуры долей коры | Не нарушены |
| Глаз, ухо и относящиеся к ним структуры (s 210-s 260) | s 2601.1 — легкое нарушение вестибулярного лабиринта | Не нарушены |
| Структуры, участвующие в голосообразовании и речи (s 310-s 340) | Не нарушены | Не нарушены |
| Структуры сердечно-сосудистой, иммунной и дыхательной систем (s 410-s 430) | s 4100.2.2 — умеренные нарушения структуры сердца с поражением передней стенки левого желудочка s 4101.3 — выраженные нарушения структуры артерий s 4102.1 — легкие нарушения структуры вены s 4301.2 — умеренные нарушения структуры легких | s 4101.2 — умеренные нарушения структуры артерий |
| Структуры, относящиеся к пищеварительной системе, метаболизму и эндокринной системе (s 510-s 580) | Нет нарушений | s 550.1 — легкие нарушения структуры поджелудочной железы s 5800.1 — легкие нарушения структуры гипофиза |
| Структуры, относящиеся к урогенитальной и репродуктивной системам (s 610-s 630) | s 6100.1.3 — легкое нарушение структуры почек с обеих сторон | Не нарушений |
| Структуры, связанные с движением (s 710-s 770) | Нет нарушений | Нет нарушений |
| Кожа и относящиеся к ней структуры (s 810-s 840) | Нет нарушений | Нет нарушений |
Как видно из представленной таблицы, у больного М. наблюдались более выраженные структурные нарушения и составляли от 0 до 85%. У больного Л. структурные нарушения составляли от 0 до 44%.
В табл. 3 представлена оценка основных категорий активности и участия больных М. и Л. согласно положениям МКФ.
Таблица 3.
Оценка категорий активности и участия у больных М. и Л.
| Категории активности и участия | Больной М., 58 лет | Больной Л., 55 лет |
| Обучение и применение знаний (d 110-d 177) | d 1551.1 — легкие затруднения при приобретении комплексных навыков. d 160.1 — легкие нарушения концентрации внимания d 1750.1 — легкое нарушение при решении сложных проблем. | d 160.1 — легкие нарушения концентрации внимания |
| Общие задачи и требования (d 210-d 240) | d 2101.1 — легкое затруднение при выполнении сложных задач d 2200.1 — легкое затруднение при выполнении многоплановых задач d 2401.1 — легкие затруднения при преодолении стресса d 2402.1 — легкие затруднения при преодолении кризисных ситуаций | d 2401.1 — легкие затруднения при преодолении стресса d 2402.1 — легкие затруднения при преодолении кризисных ситуаций |
| Общение (d 310-d 360) | Нет нарушений | Нет нарушений |
| Мобильность (d 410-d 480) | d 4501.2 — умеренные затруднения при ходьбе на дальние расстояния d 4502.2 — умеренные затруднения при ходьбе по различным поверхностям d 4551.2 — умеренные затруднения при преодолении препятствий d 4552.2 — умеренные затруднения при беге d 4553.2 — умеренные затруднения при прыжках d 4602.2 — умеренные затруднения при передвижении вне своего дома и вне других зданий d 4700.2 — умеренные затруднения при использовании транспорта, в котором движущей силой является человек | d 4552.1 — легкие затруднения при беге d 4553.1 — легкие затруднения при прыжках |
| Самообслуживание (d 510-d 570) | Нет нарушений | Нет нарушений |
| Бытовая жизнь (d 610-d 660) | d 6100.3 — значительные трудности в покупке жилья d 6101.3 — значительные трудности при аренде жилья d 6102.3 — значительные трудности в благоустройстве жилья d 6200.1 — легкие затруднения при осуществлении покупок. d 6400.2 — умеренные затруднения при стирке и сушке белья и одежды d 6401.1 — легкие затруднения при уборке на кухне и мытье посуды d 6402.2 — умеренные затруднения при уборке жилой части. d 6501.2 — умеренные затруднения при поддержании сохранности жилья и обстановки d 6506.1 — легкие затруднения при заботе о животных | Нет нарушений |
| Межличностные взаимодействия и отношения (d 710-d 770) | Нет нарушений | Нет нарушений |
| Главные сферы жизни (d 810-d 870) | d 8451.2 — умеренные трудности при выполнении трудовых обязанностей d 8502.2 — умеренные затруднения при осуществлении полной трудовой занятости d 8700.2 — умеренные затруднения при использовании личных экономических ресурсов | Нет нарушений |
| Жизнь в сообществах, общественная жизнь и гражданская жизнь (d 910-d 950) | d 9201.2 — умеренные затруднения при участии в спортивных состязаниях | d 9201.1 — легкие затруднения при участии в спортивных состязаниях |
Как видно из приведенной таблицы, у больного М. наблюдается более выраженные нарушения категорий активности и участия по сравнению с больным Л., что в основном проявляется при оценке мобильности, бытовой жизни и главных сфер жизни. Так, у больного М. имеется большее количество нарушенных категорий мобильности и бытовой жизни в связи с выраженной одышкой и возникновением болей в сердце при выполнении привычной физической нагрузки для данного больного. Большое количество нарушенных категорий в главных сферах жизни вероятнее всего у больного М. объясняется тем, что больной в связи с основным заболеванием не может продолжать работу в основной профессии в прежних условиях, что требует проведения мер профессиональной адаптации и обуславливает необходимость мер социальной защиты. У больного М. нарушенные категории активности и участия могут быть оценены в диапазоне 0-95%, а у больного Л. — 0-20%.
В табл. 4 представлена оценка факторов окружающей среды, которые непосредственно оказывают влияние на состояние больных М. и Л.
Таблица 4.
Оценка факторов окружающей среды больных М. и Л.
| Факторы окружающей среды | Больной М., 58 лет | Больной Л., 55 лет |
| Продукция и технологии (е 110-е 165) | е 1101+2 — умеренное облегчение при помощи лекарственных веществ е 1150+2 — умеренное облегчение при использовании основных изделий и технологий для личного повседневного использования е 1200+2-умеренное облегчение при использовании основных изделий и технологий для персонального передвижения и перевозки внутри и вне помещений е 1250+2-умеренное облегчение при использовании основных средств и технологий коммуникации | е 1101+3 — значительное облегчение при помощи лекарственных веществ е 1150+3 — значительное облегчение при использовании основных изделий и технологий для личного повседневного использования |
| Природное окружение и изменения окружающей среды, осуществляемые человеком (е 210-е 260) | е 2250.2 — умеренный барьер в виде изменения температуры е 2251.2 — умеренный барьер в виде повышенной влажности е 2252.2 — умеренный барьер в виде колебания атмосферного давления е 2253.2 — умеренные нарушения в виде осадков, е 2254.2 — умеренный барьер в виде сильного ветра | 2252.1 — незначительный барьер в виде колебания атмосферного давления |
| Поддержка и взаимосвязи (е 310-е 360) | е 310+2 умеренный облегчающий фактор в виде помощи членов семьи и ближайших родственников е 330.2 умеренный барьер в виде лиц, обладающих властью и авторитетом е 355+2 умеренный облегчающий фактор в виде помощи профессиональных медицинских работников | е 310+3 значительный облегчающий фактор в виде помощи членов семьи и ближайших родственников е 330+1 незначительный облегчающий фактор в виде лиц, обладающих властью и авторитетом е 355+3 значительный облегчающий фактор в виде помощи профессиональных медицинских работников |
| Установки (е 410-е 465) | е 410+2 умеренный облегчающий фактор в виде индивидуальных установок семьи и ближайших родственников е 430.2 умеренный барьер в виде индивидуальных установок лиц, обладающих властью и авторитетом е 450+2 умеренный облегчающий фактор в виде индивидуальных установок профессиональных медицинских работников | е 410+3 значительный облегчающий фактор в виде индивидуальных установок семьи и ближайших родственников е 430+1 легкий облегчающий фактор в виде индивидуальных установок лиц, обладающих властью и авторитетом е 450+3 значительный облегчающий фактор в виде индивидуальных установок профессиональных медицинских работников |
| Службы, административные системы и политика (е 510-е 595) | е 5800+2 — умеренный облегчающий фактор в виде службы здравоохранения е 5801+2 — умеренный облегчающий фактор в виде административных систем здравоохранения е 5802+2 — умеренный облегчающий фактор в виде политики здравоохранения | е 5800+2 — умеренный облегчающий фактор в виде службы здравоохранения е 5801+2 — умеренный облегчающий фактор в виде административных систем здравоохранения е 5802+2 — умеренный облегчающий фактор в виде политики здравоохранения |
Примечание: под доменами e 5800, е 5801, е 5802 подразумевается доступность медицинской помощи (амбулаторно-поликлинической, стационарной, реабилитационных мероприятий на этапе санаторно-курортного лечения), а также наличие федеральных и региональных программ развития медицинской помощи
Из представленной таблицы видно, что у больного М. присутствуют барьеры в виде природных факторов, которые воздействуют на больного, в том числе во время трудового процесса (1/3 рабочего времени больной задействован в ремонтных работах наружного освещения) и индивидуальных установок работодателя, что еще раз подчеркивает, что больной нуждается в мерах профессиональной реабилитации, правовой защите и социальной помощи. При оценке факторов окружающей среды у больного М. оценка колебалась в диапазоне 0-49%, причем как в сторону наличия барьеров, так и в сторону наличия облегчающих факторов, а у больного Л. 0-98%, при этом у данного пациента преобладали абсолютные облегчающие факторы, в связи с чем, несмотря на наличие умеренно выраженных структурно-функциональных нарушений нами не отмечено высоких степеней выраженности ограничений жизнедеятельности, что отразилось на доменах активности и участия (присутствовали только легкие нарушения).
Была проанализирована динамика изменения состояния на примере выраженности нарушенных функций больного М. при первичном и повторном обращении в бюро МСЭ после проведения реабилитационных мероприятий (рис. 1).
Рисунок 1.
Динамика восстановления нарушенных функций больного М. после проведения реабилитационных мероприятий
Как видно из представленного рисунка, первый график отражает выраженность нарушенных функций больного М. при первичном обращении в бюро МСЭ. Второй график наглядно показывает положительную динамику в результате проведения реабилитационных мероприятий.
На рис. 2 представлена динамика изменения выраженности нарушенных функций больного Л. при первичном обращении в бюро МСЭ и через год на амбулаторном приеме в поликлинике после проведения реабилитационных мероприятий.
Рисунок 2.
Динамика восстановления нарушенных функций больного Л. после проведения реабилитационных мероприятий
Как видно из представленного рисунка, график выраженности нарушенных функций больного Л. при первичном обращении в бюро МСЭ и график выраженности нарушенных функций после проведения реабилитационных мероприятий не пересекаются. Данный факт отражает полноту проведения реабилитации, а также более высокий реабилитационный потенциал по сравнению с больным М.
Таким образом, собственные исследования подтверждают, что МКФ является вполне приемлемым и оптимальным инструментом для оценки нарушенных функций у больных, динамики их изменения и реабилитационного потенциала. Учитывая широту охвата доменов функций, данная классификация применима для больных с поражением различных органов и систем, а также для оценки степени их выраженности.
Возможность применения МКФ разнообразна, однако наиболее оправдано ее применения в клинических исследованиях для оценки клинико-функционального состояния больных.
1. Международная классификация функционирования, ограничений жизнедеятельности и здоровья (краткая версия) / под ред. Г.Д. Шостка, М.В. Коробова, А.В. Шаброва. — СПб: СПбИУВЭК, 2003. — 228 с.
2. Кочубей А.В. Анализ информативности историй болезни стоматологических ортопедических пациентов с позиций международной классификации функционирования, ограничений жизнедеятельности и здоровья / А.В. Кочубей, С.А. Филюк // Кубанский медицинский вестник. — 2012. — № 3. — С. 88-91.
3. Буйлова Т.В. Международная классификация функционирования как ключ к пониманию философии реабилитации / Т.В. Буйлова // Медиаль. — 2013. — № 2. — С. 26-31.
4. Коробов М.В. Международная классификация функционирования, ограничений жизнедеятельности и здоровья: основные положения: учебно-методическое пособие / М.В. Коробов. — СПб: СПбИУВЭК, 2011. — 35 с.
5. Заболотных И.И. Кодификатор ограничений жизнедеятельности при патологии внутренних органов с учетом положений международной классификации функционирования, ограничений жизнедеятельности и здоровья (МКФ) / И.И Заболотных. — СПб: ФГБУ СПб НЦЭПР им. Г.А. Альбрехта ФМБА России, 2012. — 25 с.
6. Коробов М.В. МКФ. Классификация функций и структур организма: учебно-методическое пособие / М.В. Коробов. — СПб.: СПбИУВЭК, 2011. — 34 с.
7. Орлова Г.Г. Роль и значение международной классификации функционирования, ограничений жизнедеятельности и здоровья (МКФ) в организации должной профилактической помощи населению / Г.Г. Орлова и др. // Фундаментальные исследования. — 2013. — № 3. — С. 358-361.
8. Коробов М.В. Критерии оценки ограничений жизнедеятельности как основа медико-социальной экспертизы больных терапевтического профиля / М.В. Коробов, В.В. Сергеева, И.А. Дубинина // Новые Санкт-Петербургские врачебные ведомости. — 2005. — № 1. — С. 13-16.
9. Коробов М.В. МКФ. Классификация категорий активности и участия: учебно-методическое пособие / М.В. Коробов. — СПб: СПбИУВЭК, 2011. — 31 с.
10. Коробов М.В. МКФ. Классификация факторов окружающей среды: учебно-методическое пособие / М.В. Коробов. — СПб: СПбИУВЭК, 2011. — 31 с.
11. Grill E. Validation of International Classification of Functioning, Disability, and Health (ICF) Core Sets for early postacute rehabilitation facilities: comparisons with three other functional measures/ E. Grill and all // Am J Phys Med Rehabil. — 2006. — Vol. 85. — P. 640-649.
12. Stucki G. Application of the International Classification of Functioning, Disability and Health (ICF) in clinical practice / G. Stucki and all // Disabil Rehabil. — 2002. — Vol. 24. — P. 281-282.
13. World Health Organization. International Classification of Functioning, Disability and Health: ICF. Geneva: WHO, 2001. — P. 3-29.
1. Mezhdunarodnaya klassifikatsiya funktsionirovaniya, ogranicheniy zhiznedeyatel’nosti i zdorov’ya (kratkaya versiya), pod red. G.D. Shostka, M.V. Korobova, A.V. Shabrova [The International Classification of Functioning, Disability and Health (short version). Edit. by G.D. Shostka, M.V. Korobov, A.V. Shabrov]. Saint Petersburg: SPbIUVEK, 2003. 228 p.
2. Kochubey A.V., Filyuk S.A. Analysis informative dental histories of patients with orthopedic products International Classification of Functioning, Disability and Health. Kubanskiy meditsinskiy vestnik, 2012, no. 3, pp. 88-91 (in Russ.).
3. Buylova T.V. International classification of functioning as the key to understanding the philosophy of rehabilitation. Medial’, 2013, no. 2, pp. 26-31 (in Russ.).
4. Korobov M.V. Mezhdunarodnaya klassifikatsiya funktsionirovaniya, ogranicheniy zhiznedeyatel’nosti i zdorov’ya: osnovnye polozheniya: uchebno-metodicheskoe posobie [International Classification of Functioning, Disability and Health: Key: Textbook]. Saint Petersburg: SPbIUVEK, 2011. 35 p.
5. Zabolotnykh I.I. Kodifikator ogranicheniy zhiznedeyatel’nosti pri patologii vnutrennikh organov s uchetom polozheniy mezhdunarodnoy klassifikatsii funktsionirovaniya, ogranicheniy zhiznedeyatel’nosti i zdorov’ya (MKF) [Codificator Disability in the pathology of internal organs with the provisions of the International Classification of Functioning, Disability and Health (ICF)]. Saint Petersburg: FGBU SPb NTsEPR im. G.A. Al’brekhta FMBA Rossii, 2012. 25 p.
6. Korobov M.V. MKF. Klassifikatsiya funktsiy i struktur organizma: uchebno-metodicheskoe posobie [Classification of functions and structures: Textbook]. Saint Petersburg: SPbIUVEK, 2011. 34 p.
7. Orlova G.G. et al. The role and importance of the international Classification of Functioning, Disability and Health (ICF) in the organization of proper preventive care. Fundamental’nye issledovaniya, 2013, no. 3, pp. 358-361 (in Russ.).
8. Korobov M.V., Sergeeva V.V., Dubinina I.A. Disability evaluation criteria as a basis for medical and social examination medical patients. Novye Sankt-Peterburgskie vrachebnye vedomosti, 2005, no. 1, pp. 13-16 (in Russ.).
9. Korobov M.V. MKF. Klassifikatsiya kategoriy aktivnosti i uchastiya: uchebno-metodicheskoe posobie [Classification categories of activity and participation: Textbook]. Saint Petersburg: SPbIUVEK, 2011. 31 p.
10. Korobov M.V. MKF. Klassifikatsiya faktorov okruzhayushchey sredy: uchebno-metodicheskoe posobie [Classification of environmental factors: Textbook]. Saint Petersburg: SPbIUVEK, 2011. 31 p.
11. Grill E. et al. Validation of International Classification of Functioning, Disability, and Health (ICF) Core Sets for early postacute rehabilitation facilities: comparisons with three other functional measures. Am J Phys Med Rehabil., 2006, vol. 85, pp. 640-649.
12. Stucki G. Application of the International Classification of Functioning, Disability and Health (ICF) in clinical practice. Disabil Rehabil., 2002, vol. 24, pp. 281-282.
13. World Health Organization. International Classification of Functioning, Disability and Health: ICF. Geneva: WHO, 2001. Pp. 3-29.
Age Structure
What is the age structure of the world population and in countries around the world? How did it change over time and what can we expect for the future? These are the question that this entry focuses on.
The global median age has increased from 21.5 years in 1970 to over 30 years in 2019. The global population breakdown by age shows that a quarter (26%) are younger than 14 years, 8% are older than 65, while half of the world population is the working age bracket between 25 and 65.
The global population pyramid
The global population pyramid: How global demography has changed and what we can expect for the 21st century
In 1950 there were 2.5 billion people on the planet. Now in 2019, there are 7.7 billion. By the end of the century, the UN expects a global population of 11.2 billion. This visualization of the population pyramid makes it possible to understand this enormous global transformation.
Population pyramids visualize the demographic structure of a population. The width represents the size of the population of a given age; women on the right and men on the left. The bottom layer represents the number of newborns and above it, you find the numbers of older cohorts. Represented in this way the population structure of societies with high mortality rates resembled a pyramid – this is how this famous type of visualization got its name.
In the darkest blue, you see the pyramid that represents the structure of the world population in 1950. Two factors are responsible for the pyramid shape in 1950: An increasing number of births broadened the base layer of the population pyramid and a continuously-high risk of death throughout life is evident by the pyramid narrowing towards the top. There were many newborns relative to the number of people at older ages.
The narrowing of the pyramid just above the base is testimony to the fact that more than 1 in 5 children born in 1950 died before they reached the age of five. 1
Through shades of blue and green the same visualization shows the population structure over the last decades up to 2018. You see that in each subsequent decade the population pyramid was larger than before – in each decade more people of all ages were added to the world population.
If you look at the green pyramid for 2018 you see that the narrowing above the base is much less strong than back in 1950; the child mortality rate fell from 1-in-5 in 1950 to fewer than 1-in-20 today.
In comparing 1950 and 2018 we see that the number of children born has increased – 97 million in 1950 to 143 million today – and that the mortality of children decreased at the same time. If you now compare the base of the pyramid in 2018 with the projection for 2100 you see that the coming decades will not resemble the past: According to the projections there will be fewer children born at the end of this century than today. The base of the future population structure is narrower.
We are at a turning point in global population history. Between 1950 and today, it was a widening of the entire pyramid – an increase in the number of children – that was responsible for the increase of the world population. From now on is not a widening of the base, but a ‘fill up’ of the population above the base: the number of children will barely increase and then start to decline, but the number of people of working age and old age will increase very substantially. As global health is improving and mortality is falling, the people alive today are expected to live longer than any generation before us.
At a country level “peak child” is often followed by a time in which the country benefits from a “demographic dividend” when the proportion of the dependent young generation falls and the share of the population of working age increases. 3
This is now happening on a global scale. For every child younger than 15 there were 1.8 people of working age (15 to 64) in 1950; today there are 2.5; and by the end of the century, there will be 3.4. 4
Richer countries have benefited from this transition in the last decades and are now facing the demographic problem of an increasingly larger share of retired people that are not contributing to the labor market. In the coming decades, it will be the poorer countries that can benefit from this demographic dividend.
The change from 1950 to today and the projections to 2100 show a world population that is becoming healthier. When the top of the pyramid becomes wider and looks less like a pyramid and instead becomes more box-shaped, the population lives through younger ages with a very low risk of death and dies at an old age. The demographic structure of a healthy population at the final stage of the demographic transition is the box shape that we see for the entire world in 2100.
Politics and Massive Corruption at the World Health Organization (WHO)
This article, translated from French, was written prior to Wuhan Coronavirus epidemic outbreak
Would the world be getting along any better without this outfit, which is in theory such a good idea? Would we be in better health?
The question is as serious as it is relevant.
Though even one death is one too many, compared with the alarmist forecasts from this professional organisation that were foisted on all the ministries of health the world over, one could say that the H1N1 viral pandemic, version 2009, has so far produced not much more than a mouse.
But what a fabulous show for the media!
What a brilliantly organized panic!
How many millions of euros spent, and best of all, what worrying rumours, about the health risks linked this time to the vaccination, which might not even work!
Thus arose a psychosis that might have stolen the headlines even from a much more palpable threat, much more deadly and with effects that have already been felt to the bone by a large part of the world’s population: the climatic effects of pollution and of the way of life engendered by the currently prevailing ideology, that of extreme and unfair capitalism, «deregulated» as it is called in the sober phraseology of its well-heeled master thieves.
We have been shown people with serious faces and a professional air, the sort to whom ordinary mortals tend to ascribe genuine competence and evident integrity.
Their herald, elevated by some to hero, is called Margaret Chan. If her manner does not excite much sympathy, her curriculum vitae speaks for itself.
WHO: the Facts
Like other world organisations born from the ashes of the war of 1940-45 (the WTO, successor to GATT, the IMF, the UN, successor to the League of Nations), the WHO is a sort of transnational superministry, in this case for health.
Its power overrides that of its national equivalents. It is not subjected to genuinely democratic electoral procedures, in the sense of representing the choice expressed by the populations of its member countries. This is true of all these organisations that in fact control our daily lives in their respective fields. Its constitution came into force on 7 April 1948.
All these organisations are in a way like the arms, the tentacles of an enormous octopus whose purpose is to coordinate, improve and reinforce significant action on a planetary scale.
To clarify a crucial point: it would be misleading to think that these organisations undertake anything at all independently of each other. One could as well imagine that the liver can go on doing its own thing without being at all involved with the heart or the kidneys.
All of them work towards the same goals, each in their own specialist sphere, and all of them answer to the UN and to those who provide their funding.
The WHO has nothing to blame itself for
If you go to the official WHO site, you will of course get the impression that this organisation has a spotless record, and deserves to be praised for its humanitarian deeds.
It’s a bit like Monsanto, this multinational that dominates the market in agribusiness and wants to impose on the whole world its GM seeds complete with the Terminator gene (1), yet which tries to make you believe that the well-being and development of poor countries is its main concern.
Anyway, as in any court of law, it’s democratic, enlightened, modern, to give the «accused» party the chance to put its case.
As for the accusations of corruption and collusion with the pharmaceutical companies in the context of the worldwide vaccination campaign of 2009, it is Margaret Chan in person who has stepped up to the plate to defend the reputation of the WHO.
It’s important to realise that the accusations are weighty, well argued, and made by institutions that are well established, and pronounced by scientists and investigative journalists who are credible and trustworthy. It is difficult to dismiss all of them as a handful of conspiracy theorists, as regularly happens nowadays as soon as an interesting and well-argued debate is launched on a sensitive issue (the official version of the 9/11 attacks, the GIEC’s theory of global warming, Iran’s nuclear intentions, and so on).
It’s true that there is a certain logic in having a measure of collaboration between the WHO and the pharmaceutical companies that produce the medications.
However it is legitimate to ask questions about the exact part played by these firms in the decisions finally taken by the WHO, and on their real influence.
According to the WHO, there are many guarantees in place for managing potential conflicts of interest, as well as how they are perceived by public opinion.
The external experts who advise the WHO are [. ] obliged to provide a declaration of absence of conflict of interest as well as full professional and financial details that might compromise the impartiality of their opinions. Procedures are in place to identify, research and evaluate any potential conflicts of interest, to divulge them and take appropriate measures, such as excluding an expert from a consultative body, an expert study group or a meeting.
Still according to the WHO, the members of the Emergency Committee have to swear to the absence of any conflict of interest. The members of the Committee are chosen from a list of about 160 experts covering a range of areas of public health. The international health regulations (IHR) that came into force in 2007 envisage also a ruling that aims to coordinate the response to public health emergencies on an international scale, such as the H1N1virus pandemic. But the IHR also includes provisions for setting up, if a pandemic arises, an Emergency Committee that advises the Director General on such questions as the need to raise the level of alert, to recommend temporary measures, and so on. All the members of the Emergency Committee will have signed a confidentiality agreement, provided a declaration of no conflict of interest, and agreed to devote time as a consultant to fulfil their duty, without compensation.
Admirable principles, but without any basis in fact!
More details regarding France:
Who are the French experts? On behalf of France, we find among the consultants for the WHO and the Group SAGE, several members of the Agence de Médecine Préventive (AMP), an agency that lists its industrial partner as Sanofi Pasteur, Sanofi Aventis. We also find Prof. Daniel Floret, President of the Comité Technique de Vaccination, who lists numerous collaborations with the pharmaceutical industry; several members of the Sanofi Pasteurlaboratory, declared as such; a member of the Sanofi Pasteur MSD laboratory; and some other members from the pharmaceutical industry who are based in France.
Thanks to the site Santé log for providing the extracts (in italic, above) of a document from the WHO.
The WHO must give an account of itself
If, unlike most people who only stop to admire the window display, we actually go into the shop, we’ll discover two things:
While the fine words are there to soothe our feelings of distrust, it is still true that the close ties between the WHO experts and the pharmaceutical industry are very dangerous, very obscure and difficult to unravel.
If the complexity that characterizes all modern institutions bewilders the outsider and puts major hurdles in the way of ordinary people like me pursuing their interests, it is an unintended consequence of modernity and of the ever-multiplying range of tasks and objectives.
Being deliberately obscure is something else. It is intended to hide something, to conceal intentionally.
The financing of the WHO
In the beginning, the WHO was supposed to receive funds only from the governments of United Nations members, but a few years ago, in order to swell its coffers WHO set up what it calls a «private partnership» that allows it to receive financial support from private industries. But which industries?
Since that time its credibility, seriously tarnished, has not improved very much, and its independence is seriously questioned because of its total lack of transparency with regard to the scientific proof that supports its recommendations, and its collusion with the multinationals. It is obvious that on the world stage, business and politics have a powerful influence on health. (2)
The spotless reputation of the WHO was already besmirched by a book that came out in 1997, Le OMS : Bateau ivre de la santé publique [The WHO, the drunken sailor of public health], ed. L’Harmattan, by Bertrand Deveaud, a journalist, and Bertrand Lemennicier, professor of economics, who had spent two years making enquiries throughout the world and consulting numerous official and confidential reports. Two medical journals well-respected by the profession had already sown doubts as to the integrity and the infallibility of the WHO, The British Medical Journal (BMJ) in regard to the management of the bird flu in 2005, and The Lancet (3), which described the WHO as an institution that was corrupt and on its last legs.
Doctors Andrew Oxman and Atle Fretheim, from the Norwegian Knowledge Centre for the Health Services and Dr John Lavis, from McMaster University in Canada, interviewed the management of the WHO and analysed its various recommendations. Andrew Oxman concluded that «it is difficult to evaluate the confidence tha tone can have in the recommendations of the WHO without knowing how they were prepared.»* (*Obscurity).
«We know that our credibility is at stake,» admitted Dr Tikki Pang, director of research for the WHO. «The lack of time and the shortage of information and of money can sometimes compromise the work of the WHO.» Some senior officials of the organisation have also admitted that in many cases the proof that was supposed to be the basis of a recommendation did not exist.
Many testimonies have revealed that when the results don’t match those that the industries and companies are hoping for in order to validate their products, standards are altered and the results manipulated.
Contrary to any procedure that is genuinely scientific and independent, which should base its conclusions on the verified results of its experiments, it seems that the tendency is to do just the opposite, and that results are adapted to produce the desired conclusions; desired that is by the firms producing the medicines, vaccines, and other products concerned.
To cite one example:
Dr Oxman criticized the WHO for having its own quality control methods. In 1999 when its views on the treatment of hypertension were criticised, mainly because of the high price of the medicines recommended without any proof that they were more effective than cheaper ones, the Organisation published some «recommendations for preparing recommendations» which led to a revision of the advice on treating hypertension. (5)
Other murky issues have been brought to the surface by courageous researchers: cholesterol and statins (6), mobile telephony, with manipulation of the data on the harmfulness of electromagnetic radiation (7). and of course, serious doubts are being expressed on the real danger of the 2009 viral H1N1 pandemic, which has enabled the pharmaceutical companies to rake in millions of dollars of profit.
The bank JP Morgan on Wall Street estimated that, thanks mainly to the pandemic alert issued by the WHO, the pharmaceutical giants, who also finance the work of the ESWI run by Albert Osterhaus, were set to make $7.5-$10 billion profit. (8)
The ESWI, European Scientific Working group on Influenza, describes itself as «a multidisciplinary group of leaders of opinion on the flu, whose purpose is to fight against the repercussions of a flu epidemic or pandemic». As its members themselves explain, the ESWI, directed by Osterhaus, is the central pivot «between the WHO in Geneva, the Institut Robert Koch in Berlin and the University of Connecticut in the United States».
The most significant thing about the ESWI is that its work is entirely financed by the same pharmaceutical laboratories that are making millions thanks to the pandemic emergency, while it is the pronouncements made by the WHO that compel the governments of the whole world to buy and to stock the vaccines. The ESWI receives funding from the manufacturers and distributors of the H1N1 vaccines, such as Baxter Vaccines, MedImmune, GlaxoSmithKline, Sanofi Pasteur and others, including
Novartis, who produces the vaccine, and the distributor of Tamiflu, Hofmann-La Roche.(9)
Nicknamed «Dr Flu», Albert Osterhaus, the best known virologist in the world, official consultant on the H1N1 virus to the British and Dutch governments and head of the Department of Virology in the Medical Centre of Erasmus University, has a seat among the élite of the WHO gathered together in the SAGE Group, and is president of the ESWI, which is supported by the pharmaceutical industry.
In its turn the ESWI recommended extraordinary measures to vaccinate the whole world, considering that there was a high risk of a new pandemic which, they insisted, could be comparable to the terrifying pandemic of «Spanish» flu in 1918. (10)
Albert Osterhaus is not the only senior consultant to the WHO whose name is implicated in the dossiers on corruption and possible collusion between the WHO and the pharmaceutical firms, and an industry that wants to sell its products whatever it costs: others are David Salisbury (3)(9), Frederick Hayden (9), Arnold Monto (9), Henry L. Niman, Klaus Stöhr (11).
Professor David Salisbury, who is attached to the British Ministry of Health, is the head of SAGE at the WHO. At the same time he directs the Consultative Group on H1N1 at the WHO. Salisbury is a fervent defender of the pharmaceutical industry. In Britain the health action group One Click (10) accused him of concealing the proven correlation between vaccine use and the steep increase in autism in children, as well as the correlation between the vaccine Gardasil and cases of paralysis and even death.
Dr Frederick Hayden is at the same time member of SAGE at the WHO and of the Wellcome Trust in London; in fact he is one of the close friends of Osterhaus. In exchange for «consultative» services, Hayden receives money from Roche and from GlaxoSmithKline as well as from other pharmaceutical giants engaged in producing goods connected with the H1N1 crisis. (12)
There is yet another member of the WHO enjoying close relations with the vaccine manufacturers who profit from SAGE’s recommendations, in the person of Dr Arnold Monto, a consultant paid by the vaccine manufacturers MedImmune, Glaxo and ViroPharma. (13)
As for «Dr Flu» Osterhaus, it’s so bad that the Dutch Parliament (15) has serious doubts about him and has opened an enquiry into conflict of interest and bribery.
Outside the Netherlands and the Dutch media, only a few lines in the well-respected British journal Science (16) have made mention of the sensational investigation into the affairs of Osterhaus, who still has the confidence of his Minister of Health.
What all these experts have in common is the concealment of their connections with the pharmaceutical companies while they hold a senior and influential position in the decision-making hierarchy at the WHO, and the fact that they are never challenged. The conflict of interest is obvious, yet systematically minimized.
It is not their expertise or their intrinsic competence that is being questioned, but their independence and their integrity.
It is not the WHO that should investigate the WHO
It’s as if the accused was allowed to lead the enquiry into the crimes imputed to them. If I were an impartial prosecutor, not aiming for scandal or publicity but only for the truth, whatever it may be, even if it is worse than the worst of the lies, I would call to the bar:
Dr Wolfgang Wodarg, president of the Health Commission of the Council of Europe. This member of the German parliament, an epidemiologist, has just requested the Council for a commission of enquiry. In his interview with the paper Der Spiegel, Dr. Wodarg did not hesitate to talk about «one of the greatest medical scandals of the century». (17)
Next, Alison Katz,
A researcher who spent 17 years at the WHO, and who on 22 January 2007 sent an open letter to the new director of the agency, the Chinese Margaret Chan, accusing the organisation of «corruption, nepotism, violation of its statutes and ineffectiveness in its internal control system», and concluding that «the WHO has become a victim of neo-liberal globalisation». She denounced «the commercialisation of science and the close ties between the industry and academic institutions» and «corporatist» private science, and considered that «the WHO ought to be the leader of a movement to transform the way in which scientific research is done, including its sources of funding, as well as the acquisition and use of knowledge» and that the officials of an international organization do not have the right «not to know». (18)
Tom Jefferson: «[. ] one of the most bizarre characteristics of this flu, and of all the saga that has played out, is that year after year people make more and more pessimistic forecasts. So far none of them has come true, but these people are still there repeating their predictions. For instance, what happened to the bird flu that was supposed to kill us all off? Nothing. But that doesn’t stop these people from making their predictions. Sometimes you get the feeling that the whole industry is starting to hope for a pandemic.»
Der Spiegel: «Who are you referring to? The WHO?»
When he was asked if the WHO had deliberately declared a pandemic emergency in order to create a huge market for the H1N1 vaccines and medications, Jefferson replied:
«Don’t you find it remarkable that the WHO had changed its definition of a pandemic? The old one specified a new virus, one that spread rapidly, for which there was no immunity and that caused a high rate of illness and of death. Now these last two points on the levels of infection have been deleted, and that’s how the A flu became classed in the pandemic category.» (21)
Very conveniently, the WHO published the new definition of a pandemic in April 2009, just in time to enable them, on the advice coming from, among others, SAGE, «Dr Flu» (alias Albert Osterhaus), and David Salisbury, to declare that mild cases of the flu, renamed A H1N1, signalled a pandemic emergency. (22)
Yes, Tom Jefferson, Alison Katz, Wolfgang Wodarg, among others, and investigative journalists who are neither conspiracy fanatics nor yes-men, would be on my list of witnesses to call.
Conclusions
The vaccines have been bought, the recommendations given and millions of doses of poison already injected.
Does the truth frighten us so much that we prefer lies, and more and more of them, in our controlled lives, even when it is our health that is at stake?
It may all look very complicated but actually it is very easy.
For each new item of information, a «lite» sweetened version is made up, relayed by the bought-and-paid-for media and sold to us, the viewers, who swallow it without question.
The main drivers of this globalisation are fear and ignorance, the result of this insipid simplification of everything, which takes away any depth, any questioning that is necessary, in fact indispensable, if one wants to understand what is really happening.
It’s the same again with the dogmatic statements about manmade global warming. This no longer brooks any discussion, any further research, any questioning: it’s a heresy to even think of it. Human CO2 is the Al Qaeda equivalent of the uncertainty factor in global warming.
It’s the same again with pandemics and other health cataclysms of the future. As the GIEC tells us about CO2, the WHO simplifies the problem for us and we thank them: «Get vaccinated. Don’t ask any questions. We have the most trustworthy and competent experts. The pharmaceutical firms, overflowing with philanthropy, are working day and night to save us.» And we believe it.
Humanity of the 21st century is in grave danger, a deadly danger that lurks within each of us.
It’s not Umar Farouk Abdulmutallab (24), this Nigerian student of 23, the Christmas present from Al Qaeda to the war strategy of Peace Obama.
It’s not a virus, the St Valentine’s present to Baxter, GSK, Novartis and the rest.
It’s not our CO2, Nature’s present to our bankrupt politicians. It’s not even Al Gore, that serial sweet talker, condemned by the courts in Great Britain for no less than 11 flagrant lies and misrepresentations noted in his film, which inconveniences only the truth. (25) It’s not Al Qaeda, or any other extremist Islamic organisation.
All those are nothing but scary monsters that press the fear button, that’s to say, they are enemies but relatively minor ones.
It’s our abdication. That’s our enemy number one.
We are living in a time when globalisation has not, as it was expected to in the beginning, brought about a world that is better governed, more just, more transparent, but on the contrary, has created a system that is harder to decipher and understand, and is all-powerful.
This brew of omnipotence and dense secrecy, of being all-powerful and totally resistant to democratic investigation, is deadly. That’s the greatest threat to mankind today.
We have surrendered, preferring to go on deluding ourselves, when so many signs that something is going wrong should have impelled us to regain control.
Instead of which we put ourselves in the hands of these great authorities who are suspected of bribery and corruption, endowed with bad faith and a cynicism that balks at nothing.
Guided by the media and looking only at the things they turn their spotlight on, held by the hand, we choose to believe them instead of asking questions.
Given the present situation, I’ll answer my own question without hesitating:
The world would be getting along much better without these international organisations whose original mission has been hijacked for the sake of financial profits for the few.
As far as the WHO is concerned, we would be in much better health.
Sources
WTO: World Trade Organisation, succeeded GATT in 1994.
IMF: international Monetary Fund, created in 1944. http://en.wikipedia.org/wiki/IMF
LON: League of Nations, created in 1919, in the aftermath of the First World War. http://en.wikipedia.org/wiki/League_of_Nations
UN: United Nations Organisation, continuation of the LON, created in 1945. http://en.wikipedia.org/wiki/United_Nations
Notes
4. Sylvie Simon, op. cit.
8. Quoted in the Dutch article by Louise Voller & Kristian Villesen, «Stærk lobbyisme bag WHO-beslutningom massevaccination», Information, Copenhagen, 15 November 2009.
9. http://www.voltairenet.org/article163315.html, article by F. William Engdahl, an American journalistwho has published many works devoted to questions of energy and geopolitics. engdahl.oilgeopolitics.net/Swine_Flu/Flu_Pope/flu_pope.html
Cyrille Godefroy éd., 2007) et OGM : semences de destruction: L’arme de la faim (Jean-Cyrille Godefroy éd., 2008).
12. Jane Bryant et al., «The One Click Group Response: Prof. David Salisbury Threatens Legal Action», 4 March 2009. Download
13. William Engdahl, op.cit.
15. Tweede Kamer der Staten-Generaal (Lower Chamber of the Dutch Parliament.)
16. Martin Enserink, in «Holland, the Public Face of Flu Takes a Hit», Science, 16 October 2009, Vol. 326, n° 5951, pp. 350-351 ; DOI : 10.1126/science.326_350b.
19. William Engdahl, op. cit.
20. Conversation with Tom Jefferson: C’est toute une industrie qui espère une pandémie de grippe, Der Spiegel, 21 July 2009.
22. Article in Dutch, Louise Voller & Kristian Villesen, «Mystisk ændring af WHO’s definition af enpandemi», Copenhagen Information, 15 November 2009.
World Health Organisation (WHO) Structure, Objectives and Activities
The following information contains short notes and details on the structure, objectives and activities of the World Health Organisation (WHO) which is an important agency of the UNO. It is also contains information on the World Health Reports.
The World Health Organization (WHO) came into being in the year 1948 on the 7th of April, which also was celebrated as the first World Health Day. Its headquarters was, and still is, based in Geneva, Switzerland. It is a well endowed subsidiary of the United Nations Organization (UNO). Incidentally, it was Jawaharlal Nehru, the first prime minister of independent India who proposed the establishment of such an organization. Its basic function is to take the world’s health matters in its hands and is responsible for the coordinating efforts to generally improve public health all throughout the world. The World Trade Organization also aims at providing each and every human being on earth access to fundamental and vital healthcare. Eradication of poverty and diseases is also on the top most agenda of the WHO.
Formation Structure and Working of the World Health Organization(WHO):
The WHO constitutes of all the 191 United Nations members and also the self governing islands Cook Islands and Niue. The WHO also has got what are known as Associate Members. These Associate Members such as Tokelau and Puerto Rico have the same right to complete information as the other member states. However their rights to vote in WHO assemblies are curbed. A few other states have been granted the observer status. There are currently only 4 such states and they comprise of the Vatican City, the Chinese Taipei, The Order of Malta and Palestine. The observer status is conferred upon these states by the World Health Assembly and the criteria governing this appointment are that the states have to have a responsible contribution to health issues. It may also be noted that such members can also be an organization regardless of whether it’s government funded or otherwise. All of the member states send delegates who represent the respective member for the World Health Assembly, the supreme power of the World Health Organization. The World Health Assembly has an annual meeting in the month of May and its primary functions are approval of the WHO curriculum and also to set the WHO budget for the next two years. Another of its functions is to study dominant policy queries and to decide the course of plan.
Objectives of the World Health Organization (WHO):
World Health Report:
The primary impediment for a human being to get access to proper medical assistance and healthcare is the question of financial prowess. Along with this obtrusion comes the complication of proximity of the health centers. Salubrious health is mandatory for man’s welfare and providing it economically is amongst the World Health Organization’s primary motives. Following the footsteps of the WHO, all the member states of the WHO look forward to implementing various schemes and programs to ensure every citizen has a passage to the best healthcare services. With a view to provide the member nations a definite planning avenue, the World Health Organization came out with its leading publication, the ‘World Health Report’ which was first published in the year 1995. The health report basically chalks out how a member nation can proceed in terms of changing their financial artifices appropriately; so as to speed up the process of attaining the objective of ‘universal coverage’ that is providing healthcare services to all and sundry. The next step after achieving this goal is, like any successful endeavor, to sustain the achievement endlessly. The basis for these reports is research findings and developments, and lessons from past experiences of plan implementation. The world health report provides vital data and procedures for all member nations regardless of their developing stages in healthcare issues, and proposes paths in which the global community can work together so that the lesser fortunate nations get adequate healthcare coverage. Each year, the World Health Report provides a specialized and sophisticated appraisal on international health, including details pertaining to all nations concentrating on a particular topic. The Health Report provides basic background foundational information upon which nations can formulate policy and funding decisions. Any organization, university, professional or for that matter anyone with a personal interest in the issues of world health can avail of the World Health Report.
Activities of the World Health Organization:
The most commendable achievements of the WHO are in the fight against and successful eradication of the worlds most deadly communicable diseases. Coordination in efforts from all nations in the containment of such deadly diseases such as malaria, H1N1, tuberculosis, AIDS has been and continuously collaborated by the WHO. It also promotes and funds programs to prevent the occurrence of such diseases through vaccination and also to treat them through ground-breaking medicines. The WHO patronizes the distribution of secure drugs and medication throughout the world to fight against the outbreak of such communicable diseases. The first disease ever to be eradicated by mere human collaboration was small pox after 20 years of battling against it in the year 1980. Needless to mention, it was the WHO that carried forward this campaign. Polio is next on the WHOs list and is near eradication; we can look forward to a polio free world in a few years.
It also initiates a variant of health campaigns like propagating against the consumption of tobacco through smoking and other means. Another propaganda is promoting the consumption of vegetarian foods such as vegetables and fruits. WHO experts are currently engaged in researching on a permanent vaccine against Influenza, which is a very common chronic illness. WHO is also funding programs in member states so that they independently address the grievances associated within the nation and conduct extensive research on such subjects territorially. In this regard, the WHO has opened up 6 Regional Offices all around the globe. The World Health Organization is also constantly engaging itself in data collection activities, and is very statistics oriented when it comes to providing a basis for future planning. In this regard, the WHO has already conducted ambitious survey programs like the World Health Survey, Study on Global Aging and Adult Health, WHO Disability Assessment Scales etc. The WHO also collaborates its activities with various NGOs around the world.
10 facts on ageing and health
Today, for the first time in history, most people can expect to live into their sixties and beyond. A longer life represents an important opportunity, not only for older people and their families, but also for societies as a whole. Additional years provide the chance to pursue new activities such as further education or a long neglected passion, while continuing to make valuable contributions to family and community. Yet the extent of these opportunities depends heavily on one factor: health.
Fact 1: The world’s population is rapidly ageing
The number of people aged 60 years or older will rise from 900 million to 2 billion between 2015 and 2050 (moving from 12% to 22% of the total global population). Population ageing is happening more quickly than in the past. For example, while France had almost 150 years to adapt to a change from 10% to 20% in the proportion of the population that was older than 60 years, places like Brazil, China and India will have slightly more than 20 years to make the same adaptation.
Fact 2: There is little evidence that older people today are in better health than their parents
The proportion of older people in high-income countries needing help from another person to carry out basic activities such as eating and washing may have declined slightly over the past 30 years. However, there has been little change in the prevalence of less severe limitations in functioning.
Fact 3: The most common health conditions in older age are noncommunicable diseases
Older people in low- and middle-income countries carry a greater disease burden than those in the rich world. Regardless of where they live the biggest killers of older people are heart disease, stroke and chronic lung disease. The greatest causes of disability are sensory impairments (particularly in low- and lower-middle-income countries), back and neck pain, chronic obstructive pulmonary disease (particularly in low- and lower-middle-income countries), depressive disorders, falls, diabetes, dementia and osteoarthritis.
Fact 4: When it comes to health, there is no ‘typical’ older person
Biological ageing is only loosely associated with person age in years. Some 80 year-olds have physical and mental capacities similar to many 20 year-olds. Other people experience declines in physical and mental capacities at much younger ages.
Fact 5: Health in older age is not random
Although some of the variations in older people’s health reflect their genetic inheritance, most is due to their physical and social environments, and the influence of these environments on their opportunities and health behaviour. Importantly, these factors start to influence ageing from childhood. This means that an older person from a disadvantaged background is both more likely to experience poor health and less likely to have access to the services and the care that they may need.
Fact 6: Ageism may now be more pervasive than sexism or racism
Ageism – discrimination against a person on the basis of their age – has serious consequences for older people and societies at large. Ageism can take many forms, including prejudicial attitudes, discriminatory practices, or policies that perpetuate ageist beliefs. It can obstruct sound policy development, and it can significantly undermine the quality of health and social care that older people receive.
Fact 7: Comprehensive public health action will require fundamental shifts in how we think about ageing and health
Health in older age shouldn’t be defined by the absence of disease. Healthy Ageing is achievable by every older person. It is a process that enables older people to continue to do the things that are important to them. While health and social care expenditures for older people are often viewed as costs to society they should be understood as investments in realising opportunities and enabling older people to continue to make their many positive contributions.
Fact 8: Health systems need to be realigned to the needs of older populations
Most health systems around the world are ill-prepared to address the needs of older people, who often have multiple chronic conditions or geriatric syndromes. Systems must be capable of providing older person-centred and integrated care, and focus on maintaining capacities as people age.
Fact 9: In the 21st century, all countries need an integrated system of long-term care
In some countries, this means building a system from almost nothing. In others, it means rethinking long-term care: from a basic safety net for the most vulnerable, towards a broader system that maximizes older people’s functional ability and upholds their autonomy and dignity. The number of older people who need support for activities of daily living in developing countries is forecast to quadruple by 2050.
Fact 10: Healthy Ageing involves all levels and sectors of government
Examples of intersectoral action include establishing policies and programmes that expand housing options; making buildings and transport accessible; promoting age-diversity in working environments; and protecting older people from poverty through social protection schemes. Making progress on Healthy Ageing will also require a far better understanding of age-related issues and trends.
World health organization age classification
International Classification of Health Interventions (ICHI)
The International Classification of Health Interventions (ICHI) is a common tool for reporting and analysing health interventions for clinical and statistical purposes.
ICHI covers interventions carried out by a broad range of providers across the full scope of health systems and includes interventions on: diagnostic, medical, surgical, mental health, primary care, allied health, functioning support, rehabilitation, traditional medicine and public health.
The classification is built around three axes: Target (the entity on which the Action is carried out), Action (a deed done by an actor to a target) and Means (the processes and methods by which the Action is carried out).
Extension codes are shared with ICD and ICF in the common foundation and allow users to describe additional detail about the intervention in addition to the relevant ICHI code. A simple, logical syntax links ICHI stem codes and extension codes, interventions performed together, and packages of interventions.
The number of categories in ICHI, is determined with regard to the use cases for ICHI and the need for stability of the classification over time. The terminological core allows for a high level of detail (granularity) for all kinds of clinical documentation and data usage.
The Beta-3 version of ICHI was released in October 2020. The component relating to clinical interventions has been finalized. The components on functioning interventions and public health interventions are under final review and are finalized 2021. ICHI will be freely available, under the same licensing as ICD (ICD-11).
How China Deceived the WHO
U.S. senators are calling for investigations and the president is threatening to cut off funding. What happened?
Back in January, when the pandemic now consuming the world was still gathering force, a Berkeley research scientist named Xiao Qiang was monitoring China’s official statements about a new coronavirus then spreading through Wuhan and noticed something disturbing. Statements made by the World Health Organization, the international body that advises the world on handling health crises, often echoed China’s messages. “Particularly at the beginning, it was shocking when I again and again saw WHO’s [director-general], when he spoke to the press … almost directly quoting what I read on the Chinese government’s statements,” he told me.
The most notorious example came in the form of a single tweet from the WHO account on January 14: “Preliminary investigations conducted by the Chinese authorities have found no clear evidence of human-to-human transmission of the novel #coronavirus.” That same day, the Wuhan Health Commission’s public bulletin declared, “We have not found proof for human-to-human transmission.” But by that point even the Chinese government was offering caveats not included in the WHO tweet. “The possibility of limited human-to-human transmission cannot be excluded,” the bulletin said, “but the risk of sustained transmission is low.”
This, we now know, was catastrophically untrue, and in the months since, the global pandemic has put much of the world under an unprecedented lockdown and killed more than 100,000 people.
The U.S. was also slow to recognize the seriousness of this new coronavirus, which caught the entire country unprepared. President Donald Trump has blamed the catastrophe on any number of different actors, most recently, singling out the WHO. “They missed the call,” Trump said about the body at a briefing this week. “They could have called it months earlier.”
Trump may well be looking to deflect blame for his own missed calls, but inherent structural problems at the WHO do make the organization vulnerable to misinformation and political influence, especially at a moment when China has invested considerable resources cultivating influence in international organizations whose value the Trump administration has questioned. (Trump just in March announced he would nominate someone to fill the U.S. seat on the WHO’s Executive Board, which has been vacant since 2018.)
Even in January, when Chinese authorities were downplaying the extent of the virus, doctors at the epicenter of the outbreak in Wuhan reportedly observed human-to-human transmission, not least by contracting the disease themselves. In the most famous example, Dr. Li Wenliang was censured for “spreading rumors” after trying to alert other doctors of the new respiratory ailment; he later died of the virus himself at age 33. China now claims him as a martyr. Asked about Li’s case at a press conference, the executive director of the WHO’s Health Emergencies Programme, Michael Ryan, said, “We all mourn the loss of a fellow physician and colleague” but stopped short of condemning China for accusing him. “There is an understandable confusion that occurs at the beginning of an epidemic,” Ryan added. “So we need to be careful to label misunderstanding versus misinformation; there’s a difference. People can misunderstand and they can overreact.”
Those lost early weeks also coincided with the Chinese New Year, for which millions of people travel to visit family and friends. “That’s when millions of Wuhan people were misinformed,” Xiao said. “Then they traveled all over China, all over the world.”
The WHO, meanwhile, was getting its information from the same Chinese authorities who were misinforming their own public, and then offering it to the world with its own imprimatur. On January 20, a Chinese official confirmed publicly for the first time that the virus could indeed spread among humans, and within days locked down Wuhan. But by then it was too late.
It took another week for the WHO to declare the spread of the virus a global health emergency—during which time Dr. Tedros Adhanom Ghebreyesus, the WHO’s director-general, visited China and praised the country’s leadership for “setting a new standard for outbreak response.” Another month and a half went by before the WHO called COVID-19 a pandemic, at which point the virus had killed more than 4,000 people, and had infected 118,000 people across nearly every continent.
The organization’s detractors are now seizing on these missteps and delays to condemn the WHO (for which the U.S. is the largest donor), call for cutting the organization’s funding, or demand Tedros’s resignation. At the White House, Trump’s trade adviser Peter Navarro has been a sharp critic.
“Even as the WHO under Tedros refused to brand the outbreak as a pandemic for precious weeks and WHO officials repeatedly praised the [Chinese Communist Party] for what we now know was China’s coordinated effort to hide the dangers of the Wuhan virus from the world, the virus spread like wildfire, in no small part because thousands of Chinese citizens continued to travel around the world,” Navarro wrote to me in an email. Secretary of State Mike Pompeo recently said the administration was “reevaluating our funding with respect to the World Health Organization;” Trump has said an announcement on the matter will come next week. On the Hill, Republican Senators Martha McSally of Arizona and Rick Scott of Florida are both seeking an investigation of the WHO’s performance in the crisis and whether China somehow manipulated the organization. “Anybody who’s clear-eyed about it understands that Communist China has been covering up the realities of the coronavirus from Day 1,” McSally, who has called for Tedros to resign, told me. “We don’t expect the WHO to parrot that kind of propaganda.” Scott told me he wants to know whether the WHO followed their own procedures for handling a pandemic and why the organization hasn’t been forceful in condemning China’s missteps.
Asked for comment, a representative from the WHO pointed to a press conference Tedros gave this week. “Please quarantine politicizing COVID,” Tedros said then. “We will have many body bags in front of us if we don’t behave … The United States and China should come together and fight this dangerous enemy.” Even in early January, when it was still describing the disease as a mysterious new pneumonia, the WHO was publishing regular guidance for countries and health-care workers on how to mitigate its spread. And the organization says it has now shipped millions of pieces of protective gear to 75 countries, sent tests to more than 126, and offered training materials for health-care workers.
In any case, it’s not the WHO’s fault if China obscured the problem early on, says Charles Clift, a senior consulting fellow at Chatham House’s Center for Universal Health who worked at the WHO from 2004 to 2006. “We’d like more transparency, that’s true, but if countries find reasons to not be transparent, it’s difficult to know what we can do about it.” The organization’s major structural weakness is that it relies on information from its member countries—and the WHO team that visited China in February to evaluate the response did so jointly with China’s representatives. The resulting report did not mention delays in information-sharing, but did say that “China’s bold approach to contain the rapid spread of this new respiratory pathogen has changed the course of a rapidly escalating and deadly epidemic.” The mission came back telling reporters they were largely satisfied with the information China was giving them.
If this is something short of complicity in a Chinese cover-up—which is what former National Security Adviser John Bolton has alleged of the WHO—it does point to a big vulnerability: The group’s membership includes transparent democracies and authoritarian states and systems in between, which means the information the WHO puts out is only as good as what it’s getting from the likes of Xi Jinping and Russian President Vladimir Putin. North Korea, for instance, has reported absolutely no coronavirus cases, and the WHO isn’t really in a position to say otherwise.
The structure also gives WHO leaders like Tedros an incentive not to anger member states, and this is as true of China as it is of countries with significantly less financial clout. During the Ebola epidemic in 2014, Clift said, WHO took months to declare a public-health emergency. “That’s three very small West African countries, and WHO didn’t want to upset them,” Clift said. “WHO didn’t cover itself in glory in that one.” The response this time has been much faster and better, in Clift’s observation. “It doesn’t mean it shouldn’t be examined afterwards to see what they could have done better,” he said. “And one should really investigate the origins of what happened in China.”
The WHO has also shown, however, that it can walk the line between the need for cooperation and information-sharing from member states and the need to hold them accountable for mistakes. During the SARS outbreak in 2003, a WHO spokesman criticized China for its lack of transparency and preparation, which had allowed the virus to spread unchecked. China even later admitted to mistakes in handling the outbreak.
No such critique has been forthcoming this time. One study found that China could have limited its own infections by up to 95 percent had the government acted in that early period when doctors were first raising the alarm and the Chinese Communist Party was still denying the extent of the problem. “The WHO at that time didn’t do their job,” Xiao said. “The opposite: They actually compounded Chinese authorities’ misinformation for a few weeks. That is, to me, unforgivable.”
International Standard Classification of Occupations (ISCO)
The International Classification of Occupations (ISCO) seeks to facilitate international communication about occupations by providing statisticians with a framework to make internationally comparable occupational data available, and by allowing international occupational data to be produced in a form that can be useful for research as well as for specific decision-making and action-oriented activities.
The current version, known as ISCO-08, was published in 2008 and is the fourth iteration, following ISCO-58, ISCO-68 and ISCO-88.
Definitions
A job is defined in ISCO-08 as “a set of tasks and duties performed, or meant to be performed, by one person, including for an employer or in self employment”.
Occupation refers to the kind of work performed in a job. The concept of occupation is defined as a “set of jobs whose main tasks and duties are characterized by a high degree of similarity”. A person may be associated with an occupation through the main job currently held, a second job, a future job or a job previously held.
Skill is defined as the ability to carry out the tasks and duties of a given job. For the purposes of ISCO-08, two dimensions of skill are used to arrange occupations into groups. These are skill level and skill specialization.
Skill level is defined as a function of the complexity and range of tasks and duties to be performed in an occupation. Skill level is measured operationally by considering one or more of:
Structure
Looking at the hierarchical structure of ISCO-08 from the top down, each of the ten major groups is made up of one or more sub-major groups, which in turn are made up of one or more minor groups. Each of the 130 minor groups is made up of one or more unit groups. In general, each unit group is made up of several “occupations” that have a high degree of similarity in terms of skill level and skill specialization.
Each group in the classification is designated by a title and code number and is associated with a description that specifies the scope of the group.
Number of groups at each level
| Major Groups | Sub Major Groups | Minor Groups | Unit Groups | Skill level |
|---|---|---|---|---|
| 1 Managers | 4 | 11 | 31 | 3 and 4 |
| 2 Professionals | 6 | 27 | 92 | 4 |
| 3 Technicians and Associate Professionals | 5 | 20 | 84 | 3 |
| 4 Clerical Support Workers | 4 | 8 | 29 | 2 |
| 5 Service and Sales Workers | 4 | 13 | 40 | 2 |
| 6 Skilled Agricultural, Forestry and Fishery Workers | 3 | 9 | 18 | 2 |
| 7 Craft and Related Trades Workers | 5 | 14 | 66 | 2 |
| 8 Plant and Machine Operators, and Assemblers | 3 | 14 | 40 | 2 |
| 9 Elementary Occupations | 6 | 11 | 33 | 2 |
| 0 Armed Forces Occupations | 3 | 3 | 3 | 1, 2 and 4 |
| Total number of groups | 43 | 130 | 436 |
Find an occupation in ISCO-08
Use the search function to find an occupation (tips: use the drop-down to select which columns to search and use quotes around a term, for example “nurse”, for more precise search results). In the table of results, click on the + sign to the left of the occupation title to learn more.
This mapping as well as ISCO-08 and ISCO-88 are also available in other formats (if your browser allows for it, or right click to copy/paste the link directly into the browser):
Skill levels
Statistics by occupation are presented in ILOSTAT according to both the categories of the latest version of the ISCO available and broad skill levels, based on the following correspondence table:
| Broad skill level | ISCO-08 | ISCO-88 |
|---|---|---|
| Skill levels 3 and 4 | 1. Managers | 1. Legislators, senior officials and managers |
| 2. Professionals | 2. Professionals | |
| 3. Technicians and associate professionals | 3. Technicians and associate professionals | |
| Skill level 2 | 4. Clerical support workers | 4. Clerks |
| 5. Service and sales workers | 5. Service workers and shop and market sales workers | |
| 6. Skilled agricultural, forestry and fishery workers | 6. Skilled agricultural and fishery workers | |
| 7. Craft and related trades workers | 7. Craft and related trades workers | |
| 8. Plant and machine operators, and assemblers | 8. Plant and machine operators and assemblers | |
| Skill level 1 | 9. Elementary occupations | 9. Elementary occupations |
| Armed forces | 0. Armed forces occupations | 0. Armed forces |
| Not elsewhere classified | X. Not elsewhere classified | X. Not elsewhere classified |
Table of contents
Statistical standards
Featured publication
International Standard Classification of Occupations (ISCO-08), Volume 1: Structure, group definitions and correspondence tables
NEWS: The forthcoming revision of ISCO
ISCO-08 is currently being revised. This revision is undertaken by a Technical Working Group (TWG) and the ILO statistics department. The objectives of the revision are:
The history of ISCO
In addition to ISCO-08, three versions of ISCO were developed in the past. The first complete version of ISCO was adopted in 1957 by the Ninth International Conference of Labour Statisticians (ICLS), it is known as ISCO-58. ISCO-58 was superseded by ISCO-68, which was adopted by the Eleventh ICLS in 1966. The third version, ISCO-88, was adopted by the Fourteenth ICLS in 1987.
Distinctions between different occupational classes were introduced in population censuses undertaken in the early parts of the 19th century in several countries, but the identification of occupation and industry as different variables, each requiring its own classification, was only made towards the end of that century, as it became increasingly clear that the division of labour between firms and organizations in an industrial society was distinct from the division of labour between different jobs within the same firm.
The history of the development of ISCO has always been closely connected with the work of the International Conference of Labour Statisticians (ICLS) which meets under the auspices of the International Labour Organization (ILO).
The need for an international standard classification of occupations was, in fact, discussed at the first ICLS in 1923, although this conference did not propose a specific grouping of occupations. The first concrete step towards its establishment was the adoption, by the Seventh ICLS in 1949 of nine major groups termed the International Standard Classification of Occupations. The seventh ICLS proposed further development of this classification to more detailed level and identified basic principles to be followed in the collection and tabulation of occupational data, including that:
In 1952, the ILO published the International Classification of Occupations for Migration and Employment Placement (ICOMEP), with descriptions of 1727 occupations based on national reference materials sourced principally from 13 countries, and organized within the framework of the nine major groups adopted by the Seventh ICLS.
In 1954, the Eighth ICLS approved a list of minor groups which was subsequently submitted to the governments and to a group of experts for comments.
In 1957, the Ninth ICLS adopted the first complete version of the International Standard Classification of Occupations known as ISCO-58 and comprising a classification structure of 10 major groups, 73 minor groups, 201 unit groups, 1345 occupations and an index of occupational titles. All groups at each level of the classification were given a unique code, title and description, drafted in consultation with the governments. It was published in 1958.
The Ninth ICLS also proposed a prompt revision of ISCO-58. In 1965, a working party examined proposals made on the basis of comments from about 80 countries and ten international organisations concerning the classification. This facilitated the development of a draft classification which was discussed, amended and adopted as ISCO-68 by the Eleventh ICLS in 1966. ISCO-68 consists of 8 major groups, 83 minor groups, 284 unit groups and 1506 occupational categories. It includes definitions for each of the 1881 groups describing the general functions of the occupations as well as the main tasks performed by the workers concerned. It includes an expanded alphabetical list of several thousand titles as well as a table of conversion from ISCO-58 to ISCO-68. The English and French versions were published in 1969 and the Spanish version in 1970.
The third edition of ISCO (ISCO-88) was adopted by the 14th ICLS in 1987 and approved by the ILO Governing Body in 1988. The major changes introduced were that:
Early during the first decade of the 21st century, it became clear that there was a need to update ISCO-88. In December 2003 the 17th ICLS requested that the ILO complete work to update ISCO-88 by the end of 2007 so that the results could be taken into account in national preparations for the majority of population censuses to be undertaken in the 2010 round. The updated classification, ISCO-08 was adopted by a Meeting of Experts in Labour Statistics in December 2007.
Whilst it employs a similar conceptual model to that used for ISCO-88, and the 10 major groups were not changed in concept, ISCO-08 is slightly more detailed at its disaggregate levels and comprises 43 sub-major groups, 131 minor groups and 436 unit groups. Like its predecessor, ISCO-08 provides descriptions for all of the categories identified at each of the four levels of its structure, and can be extended by defining detailed occupations if and when required for specific national or regional purposes. ISCO-08 is now being revised.
World health organization age classification
The international file, including all mandatory variables for all regions and countries that took part in the 2017/18 HBSC survey, will be available via Open Access from October 2022.
Launch of the new HBSC study website
Our primary goal in launching this new website is to provide visitors with a responsive, user-friendly experience that offers easy access to key information about the study and materials such as reports and other publications.
WHO European Regional Obesity Report reveals extent of health challenge across Europe
The new WHO European Regional Obesity Report 2022 reveals that almost two-thirds of adults and 1 in 3 children in the WHO European Region live with overweight or obesity, and these rates are growing.
About the study
Health Behaviour in School-aged Children (HBSC) is a WHO collaborative cross-national study of adolescent health and well-being. Founded in 1982, the survey is undertaken every four years using a self-report questionnaire. HBSC uses findings at national, regional and international levels to:
Years since the study was founded
Researchers in the network
Member countries taking part
thousand young people surveyed in 2017/18
What do we research and why?
HBSC focuses on understanding young people’s health in their social context – at home, school, and with family and friends. It aims to improve understanding of how these factors, individually and collectively, influence young people’s health throughout adolescence.
The adolescent years are a critical transitional period within the life course during which rapid physical, emotional, cognitive, and social development occurs. These years mark a period of increased autonomy during which health-related behaviours develop and independent decision-making may influence their current and future health.
The adolescent years, therefore, provide a critical opportunity for prevention and intervention to support young people’s healthy growth and development, promote future health and well-being in adulthood, and, as such, underpin the health of the next generation.
How are data collected?
Data are collected in all participating countries and regions through school-based surveys using a standard methodology detailed in the HBSC international study protocol. Each country or region uses cluster sampling to select a proportion of young people aged 11, 13 and 15, ensuring that the sample is representative of all in the age range. Around 1500 students in each HBSC country or region are selected from each age group. A total of 227 441 young people took part in the 2017/18 survey.
ICD-10 Version:2019
Quick Search Help
Quick search helps you quickly navigate to a particular category. It searches only titles, inclusions and the index and it works by starting to search as you type and provide you options in a dynamic dropdown list.
You may use this feature by simply typing the keywords that you’re looking for and clicking on one of the items that appear in the dropdown list. The system will automatically load the item that you’ve picked.
You may use wildcards ‘*’ as well to find similar words or to simply save some typing.
For example, tuber* confirmed will hit both tuberculosis and tuberculous together with the word ‘confirmed’
If you need to search other fields than the title, inclusion and the index then you may use the advanced search feature
You may also use ICD codes here in order to navigate to a known ICD category.
The colored squares show from where the results are found.
( green:Title, blue:inclusions, orange:index, red:ICD code)
You don’t need to remeber the colors as you may hover your mouse on these squares to read the source.
The top 10 causes of death
In 2019, the top 10 causes of death accounted for 55% of the 55.4 million deaths worldwide.
The top global causes of death, in order of total number of lives lost, are associated with three broad topics: cardiovascular (ischaemic heart disease, stroke), respiratory (chronic obstructive pulmonary disease, lower respiratory infections) and neonatal conditions – which include birth asphyxia and birth trauma, neonatal sepsis and infections, and preterm birth complications.
Causes of death can be grouped into three categories: communicable (infectious and parasitic diseases and maternal, perinatal and nutritional conditions), noncommunicable (chronic) and injuries.
Leading causes of death globally
At a global level, 7 of the 10 leading causes of deaths in 2019 were noncommunicable diseases. These seven causes accounted for 44% of all deaths or 80% of the top 10. However, all noncommunicable diseases together accounted for 74% of deaths globally in 2019.
The world’s biggest killer is ischaemic heart disease, responsible for 16% of the world’s total deaths. Since 2000, the largest increase in deaths has been for this disease, rising by more than 2 million to 8.9 million deaths in 2019. Stroke and chronic obstructive pulmonary disease are the 2nd and 3rd leading causes of death, responsible for approximately 11% and 6% of total deaths respectively.
Lower respiratory infections remained the world’s most deadly communicable disease, ranked as the 4th leading cause of death. However, the number of deaths has gone down substantially: in 2019 it claimed 2.6 million lives, 460 000 fewer than in 2000.
Neonatal conditions are ranked 5th. However, deaths from neonatal conditions are one of the categories for which the global decrease in deaths in absolute numbers over the past two decades has been the greatest: these conditions killed 2 million newborns and young children in 2019, 1.2 million fewer than in 2000.
Deaths from noncommunicable diseases are on the rise. Trachea, bronchus and lung cancers deaths have risen from 1.2 million to 1.8 million and are now ranked 6th among leading causes of death.
In 2019, Alzheimer’s disease and other forms of dementia ranked as the 7th leading cause of death. Women are disproportionately affected. Globally, 65% of deaths from Alzheimer’s and other forms of dementia are women.
One of the largest declines in the number of deaths is from diarrhoeal diseases, with global deaths falling from 2.6 million in 2000 to 1.5 million in 2019.
Diabetes has entered the top 10 causes of death, following a significant percentage increase of 70% since 2000. Diabetes is also responsible for the largest rise in male deaths among the top 10, with an 80% increase since 2000.
Other diseases which were among the top 10 causes of death in 2000 are no longer on the list. HIV/AIDS is one of them. Deaths from HIV/AIDS have fallen by 51% during the last 20 years, moving from the world’s 8th leading cause of death in 2000 to the 19th in 2019.
Kidney diseases have risen from the world’s 13th leading cause of death to the 10th. Mortality has increased from 813 000 in 2000 to 1.3 million in 2019.
Leading causes of death by income group
The World Bank classifies the world’s economies into four income groups – based on gross national income – low, lower-middle, upper-middle and high.
People living in a low-income country are far more likely to die of a communicable disease than a noncommunicable disease. Despite the global decline, six of the top 10 causes of death in low-income countries are communicable diseases.
Malaria, tuberculosis and HIV/AIDS all remain in the top 10. However, all three are falling significantly. The biggest decrease among the top 10 deaths in this group has been for HIV/AIDS, with 59% fewer deaths in 2019 than in 2000, or 161 000 and 395 000 respectively.
Diarrhoeal diseases are more significant as a cause of death in low-income countries: they rank in the top 5 causes of death for this income category. Nonetheless, diarrhoeal diseases are decreasing in low-income countries, representing the second biggest decrease in fatalities among the top 10 (231 000 fewer deaths).
Deaths due to chronic obstructive pulmonary disease are particularly infrequent in low-income countries compared to other income groups. It does not appear in the top 10 for low-income countries yet ranks in the top 5 for all other income groups.
Lower-middle-income countries have the most disparate top 10 causes of death: five noncommunicable, four communicable, and one injury. Diabetes is a rising cause of death in this income group: it has moved from the 15th to 9th leading cause of death and the number of deaths from this disease has nearly doubled since 2000.
As a top 10 cause of death in this income group, diarrhoeal diseases remain a significant challenge. However, this category of diseases represents the biggest decrease in absolute deaths, falling from 1.9 million to 1.1 million between 2000 and 2019. The biggest increase in absolute deaths is from ischaemic heart disease, rising by more than 1 million to 3.1 million since 2000. HIV/AIDS has seen the biggest decrease in rank among the previous top 10 causes of death in 2000, moving from 8th to 15th.
In upper-middle-income countries, there has been a notable rise in deaths from lung cancer, which have increased by 411 000; more than double the increase in deaths of all three other income groups combined. In addition, stomach cancer features highly in upper-middle-income countries compared to the other income groups, remaining the only group with this disease in the top 10 causes of death.
One of the biggest decreases in terms of absolute number of deaths is for chronic obstructive pulmonary disease, which has fallen by nearly 264 000 to 1.3 million deaths. However, deaths from ischaemic heart disease have increased by more than 1.2 million, the largest rise in any income group in terms of absolute number of deaths from this cause.
There is only one communicable disease (lower respiratory infections) in the top 10 causes of death for upper-middle-income countries. Notably, there has been a 31% fall in deaths from suicide since 2000 in this income category, decreasing to 234 000 deaths in 2019.
In high-income countries, deaths are increasing for all top 10 diseases except two. Ischaemic heart disease and stroke are the only causes of death in the top 10 for which the total numbers have gone down between 2000 and 2019, by 16% (or 327 000 deaths) and by 21% (or 205 000 deaths) respectively. High-income is the only category of income group in which there have been decreasing numbers of deaths from these two diseases. Nonetheless ischaemic heart disease and stroke have remained in the top three causes of death for this income category, with a combined total of over 2.5 million fatalities in 2019. In addition, deaths from hypertensive heart disease are rising. Reflecting a global trend, this disease has risen from the 18th leading cause of death to the 9th.
Deaths due to Alzheimer’s disease and other dementias have increased, overtaking stroke to become the second leading cause in high-income countries, and being responsible for the deaths of 814 000 people in 2019. And, as with upper-middle-income countries, only one communicable disease, lower respiratory infections, appears in the top 10 causes of death.
Why do we need to know the reasons people die?
It is important to know why people die to improve how people live. Measuring how many people die each year helps to assess the effectiveness of our health systems and direct resources to where they are needed most. For example, mortality data can help focus activities and resource allocation among sectors such as transportation, food and agriculture, and the environment as well as health.
COVID-19 has highlighted the importance for countries to invest in civil registration and vital statistics systems to allow daily counting of deaths, and direct prevention and treatment efforts. It has also revealed inherent fragmentation in data collection systems in most low-income countries, where policy-makers still do not know with confidence how many people die and of what causes.
Furthermore, the World Health Organization develops standards and best practices for data collection, processing and synthesis through the consolidated and improved International Classification of Diseases (ICD-11) – a digital platform that facilitates reporting of timely and accurate data for causes of death for countries to routinely generate and use health information that conforms to international standards.
Editor’s note
WHO Mortality Database
The WHO Mortality Database is a compilation of mortality data as reported annually by Member States from their civil registration and vital statistics systems.
Download raw data files
Basic underlying raw data files, together with the necessary instructions, file structures, code reference tables, etc. These data can be used by institutions and organizations which need access at this level of detail, mainly for research purposes, AND have the required information technology (IT) resources to use this information.
These files do not constitute a user-friendly data collection which the average user can download and access. These are the basic underlying raw data files, together with the necessary instructions, file structures, code reference tables, etc. which can be used by institutions and organizations which need access at this level of detail mainly for research purposes and have available the required information technology (IT) resources to use this information. These files will not open in programs like Excel; please refer to the «Documentation.zip» file hereafter for more information on systems requirements.
It should be noted that these data are transmitted on the understanding that no use will be made of them for commercial purposes and that no such permission or right to use may be implied thereby. WHO requests data users to adhere to the guidelines outlined on the next page.
Last update: 15 February 2022
Documentation
Last update: 18 February 2022
Contains a Word file with information on the WHO Mortality Database, file specifications and list of causes of death.
Availability
Last update: 15 February 2022
Contains an Excel file with the list of countries-years available for the mortality and population data.
Country codes
Last update: 01 March 2021
Country codes and names.
Notes
Last update: 15 February 2022
Notes pertaining to data for some countries-years.
Population and live births
Last update:15 February 2022
Reference populations and live births.
Mortality, ICD-7
Last update: 18 February 2004
Data file containing the detailed mortality data for the seventh revision of the ICD (International Classification of Diseases).
Mortality, ICD-8
Last update: 9 July 2012
Data file containing the detailed mortality data for the eighth revision of the ICD (International Classification of Diseases).
Mortality, ICD-9
Last update: 29 March 2017
Data file containing the detailed mortality data for the ninth revision of the ICD (International Classification of Diseases).
Mortality, ICD-10 (part 1/5)
Last update: 15 February 2022
Data file containing the detailed mortality data for the tenth revision of the ICD (International Classification of Diseases).
Mortality, ICD-10 (part 2/5)
Last update: 01 March 2021
Data file containing the detailed mortality data for the tenth revision of the ICD (International Classification of Diseases).
Mortality, ICD-10 (part 3/5)
Last update: 15 February 2022
Data file containing the detailed mortality data for the tenth revision of the ICD (International Classification of Diseases).
Mortality, ICD-10 (part 4/5)
Last update: 15 February 2022
Data file containing the detailed mortality data for the tenth revision of the ICD (International Classification of Diseases).
Mortality, ICD-10 (part 5/5)
Last update: 18 February 2022
Data file containing the detailed mortality data for the tenth revision of the ICD (International Classification of Diseases).
About the data files
Users should read carefully the «documentation.zip» file which contains new information added.
You are being provided herewith the original detailed data files which comprise the WHO Mortality DataBase (MDB). Due to the large size of these files, they are provided in ASCII (comma separated values) format to facilitate the download process. You should import these data files into a Database Management System rather than spreadsheets. These are the basic underlying detailed data files, together with the necessary instructions, file structures, code reference tables, etc. for use by those who need access to the full level of detail for specific analyses. Instructions for importing the comma separated values files into Microsoft Access are listed in Annex Table 3 of the «Documentation.zip» file. However users are strongly recommended not to try to import the data into spreadsheets because of the excessive number of records. There are over 2 million records in one data file.
The data available on this web site comprise deaths registered in national vital registration systems, with underlying cause of death as coded by the relevant national authority. These data are official national statistics in the sense that they have been transmitted to the World Health Organization by the competent authorities of the countries concerned. Each Member State reports population data along with their mortality data, for the population covered by the death registration system. Where this is a subset of the national population, the data is labelled accordingly in the WHO Mortality Database, e.g. Brazil (North and North-east) or Paraguay (reporting areas). However, the completeness of death registration may also be less than 100% for the specified registration population.
For Member States with incomplete vital registration systems, demographic techniques have been used by WHO to estimate the level of completeness of death recording for the specified population to allow the calculation of death rates. These population data are provided along with the deaths data. The proportion of all deaths which are registered in the population covered by the vital registration system for a country (referred to as completeness) has been estimated by WHO for the latest available year and is given in Table 3 available on this website.
The designations employed and the presentation of material in the MDB do not imply the expression of any opinion whatsoever on the part of the World Health Organization or other parties involved in the MDB concerning the legal status of any country, territory or area, its authorities, its current or former official name, or the delimitation of its frontiers or boundaries. Accordingly: a) strictly for purposes of statistical use, denominations are used which, although applicable at one particular time, may not reflect correct terminology at some other point in the historical context in which they are so used; b) references to «former» entities refer to countries that formerly existed under those names, or abbreviations; and c) in some cases, denominations are used to refer to countries as they currently exist and, when used with respect to data relating to before the existence of these countries as independent states, to sub-national entities of formerly existing larger countries.
WHO asks users to cooperate in the use of electronically transmitted data by adhering to the following guidelines:
It should be noted that these data are transmitted on the understanding that no use will be made of them for commercial purposes and that no such permission or right to use may be implied thereby.
It’s Time to Dismantle the World Health Organization
The WHO and those in charge of public health, the virologists and the pharmaceutical laboratories… created a whole system around the imminence of a pandemic.
There is a lot of money at stake, as well as networks of influence, careers and whole institutions! And the minute one of the flu viruses mutates we’d see the whole machine roll into action.
The ultimate international authority for infectious diseases is the World Health Organization (WHO).
Due to its widespread acceptance by the world’s national governments, it has been extremely successful in assuming the helm to monitor regional and global infectious diseases and dictate medical intervention policies to international health agencies.
The organization has become the final word to rule whether the spread of a serious pathogen is a pandemic or not.
For the majority of the medical community, the media and the average person, the WHO is the front line command post for medical prevention (i.e., vaccination) and treatment.
Consequently its rulings are often regarded as the gold standard. On matters of global health, the WHO holds dominance.
For approximately a year the WHO has propagated the belief that the first line of defense for curtailing the COVID-19 pandemic is self-isolation, distancing, masks and, ultimately, vaccination.
Although it approved Ivermectin as a cost-effective treatment against SARS-CoV-2 infections, it disapproved hydroxychloroquine in favor of Gilead Bioscience’s and the National Institute of Allergy and Infectious Disease’s (NIAID) Anthony Fauci’s novel and costly drug Remdesivir.
Much of it’s funding efforts have been reserved for mass-vaccination with the new generation of experimental jjabs.
Throughout these efforts, the WHO has allied itself with the US’s and UK’s national health systems, and the Bill and Melinda Gates Foundation and his Global Alliance for Vaccines and Immunization (GAVI) initiative.
Most people wrongly assume the WHO acts independently from private commercial and national government interests for the welfare of the world’s population.
The legitimacy of the WHO as a gold standard of health is dubious.
The organization has frequently been accused of conflicts of interests with private pharmaceutical companies and mega-philanthropic organizations such as the Gates’ Foundation, as well as being riddled with political alliances, ideologies, and profiteering motives.
Despite it’s mega-pharmaceutical interests and consultants representing private jjab interests, in the past the WHO has had the audacity to ridicule the pharmaceutical industry of corruption.
“Corruption in the pharmaceutical sector occurs throughout all stages of the medicine chain, from research and development to dispensing and promotion…. A lack of transparency and accountability within the medicines chain can also contribute to unethical practices and corruption.”
These are similar charges that have been leveled against the WHO.
An article in the National Review called the WHO “scandal plagued” with “wasteful spending, utter disregard for transparency, pervasive incompetence, and failure to adhere to even basic democratic standards.”
In his book, Immunization: How Vaccines Became Controversial, University of Amsterdam professor emeritus Dr. Stuart Blume raises the serious problem of the WHO’s most influential advisors on emergency health conditions, such as the current Covid-19 pandemic and earlier the 2009 H1N1 swine flu scare that never was, serve as consultants for the jjab industry.
During times of global emergencies and crises, the WHO confers with a separate group of advisors outside its formal sitting Strategic Advisory Group of Experts or SAGE; the names of this group’s members are not made public.
We would add that the WHO’s level of incompetence has resulted in serious misinformation about pandemics, medical risks of jjabs and other health-threatening chemicals.
For example, during the early stage of the COVID-19 outbreak in Wuhan, the organization reported it could not find any evidence of human transmission.
However, the WHO has repeatedly kowtowed to China’s demands and unscrupulously accepts whatever statistics and statements the Chinese Communist Party (CCP) provides.
Responding to a petition signed by over 700,000 signatories demanding the resignation of the current WHO Director General Tedros Adhanom, Japan’s Deputy Prime Minister Taro Aso told the Japanese parliament that the organization “should be renamed the Chinese Health Organization” for favoring China’s policy to stall and obstruct international investigations and for lauding unsubstantiated praise on the country’s transparency and handling of the pandemic.
Back on December 31, 2019, Taiwan – which has been barred from WHO membership due to China’s political maneuvering – had been warning of a possible human-to-human transmission contrary to the wet-market narrative, but this was largely ignored in order to avoid upsetting the CCP.
The UK’s Sunday Times reported that Chinese scientists were forced to destroy their proof of the virus shortly after its discovery. In the province of Hubei, authorities ordered the cessation of further testing and the destruction of existing samples. Other researchers who made efforts to warn the public were punished.
Writing for The Hill, University of Texas at San Antonio professor Bradley Thayer wrote:
“Tedros apparently turned a blind eye to what happened in Wuhan and the rest of China and… has helped play down the severity, prevalence and scope of the Covid-19 outbreak.”
Thayer concludes, “Tedros is not fit to lead the WHO.”
He has no formal medical training as a physician or any international management experience in global health. Many others have voiced similar criticisms pointing out Tedro’s unsuitable background.
Now heading the WHO, Tedros appears to continue lobbying on China’s behalf. In 2017, the Washington Post noted the fundamental problem:
“[China] worked tirelessly behind the scenes to help Tedros defeat the United Kingdom candidate for the WHO job, David Nabarro. Tedros’s victory was also a victory for Beijing, whose leader Xi Jinping has made public his goal of flexing China’s muscle in the world.”
Upon assuming his new position at the WHO, Tedros had left Ethiopia’s healthcare system in ruin. As one young healthcare worker reported, there was no “bare necessities of a health care office…. Sterile gloves, paper exam gowns and covers, cotton swabs, gauze, tongue depressors, alcohol prep pads, chemical test strips, suturing equipment, syringes, stethoscopes… were non-existent. This is a fact in most health care centers in Ethiopia.”
During the more recent re-investigation of SARS-CoV-2 origins, the Chinese authorities refused to provide raw case data and created repressive conditions to curtail reliable analysis and disclosure.
The WHO’s final report concluded that the virus had an animal origin and did not escape Wuhan’s high security pathogen laboratory.
But there are viable reasons to discredit the report as untrustworthy at best and perhaps intentionally deceptive.
First, the entire agenda of the investigation was staged theater rather than a deep investigation to uncover empirical evidence.
The team simply inspected seafood and open-air markets. Consequently, the WHO team returned empty handed and without laboratory records for a proper forensic examination.
To call the entire WHO effort gross incompetence would be an understatement.
Based upon all the evidence that has emerged, a large number of professional medical voices are calling the entire investigation a farce.
Most problematic is the appointment of Peter Daszak on the WHO’s group to carry out the investigation.
Daszak, the founding president of the shadowy non-profit organization EcoHealth Alliance, has headed many hunting adventures worldwide to identify the emergence of potential pathogens that could become pandemics.
With the intention to divert attention away from an escaped laboratory virus, Daszak stated on a Going Viral podcast there was no evidential reason to visit and inspect the Wuhan laboratory.
According to Independent Science News, despite Daszak’s denial of a lab origin:
“EcoHealth Alliance funded bat coronavirus research, including virus collection, at the Wuhan Institute of Virology and thus could themselves be directly implicated in the outbreak.”
The research at the Wuhan lab included ‘gain of function” efforts on coronaviruses, and received funds directly approved by Anthony Fauci.
Daszak himself has authored 25 studies funded by the Chinese Academy of Medical Sciences, think tanks, universities, military institutions, and ministries directly connected with the Chinese Communist Party.
Given the halls of power within the WHO, we are outlining some of the more salient reasons why the organization’s declarations about infectious diseases, pandemics and vaccination should not be trusted.
Vaccine Promotional Misconduct
For many years the WHO’s recommendations for certain jjabs were kept secret.
Writing in a 2006 issue of the Journal of American Physicians and Surgeons, Dr. Marc Girard uncovered “scientific incompetence, misconduct or even criminal malfeasance” over the intentional inflation of jjabs’ benefits while undermining toxicity and adverse effects.
Dr. Girard testified as a medical expert for a French court in a criminal trial against the WHO after French health officials obliged the organization to launch its universal Hepatitis B jjab campaign. The campaign resulted in the deaths of French children.
Girard gained access to confidential WHO documents. He noted that the WHO’s “French figures about chronic liver diseases were simply extrapolated from the U.S. reports.”
He further accused the WHO serving “merely as a screen for commercial promotion, in particular via the Viral Hepatitis Prevention Board (VHPB), which was created, sponsored, and infiltrated by the manufacturers.”
Now during the Covid-19 pandemic, as early as last July, the WHO approved of China’s first jjab for emergency use, long before it had undergone proper clinical trials and much earlier than Moderna’s and Pfizer’s mRNA jjabs’ approval.
Orchestration of Pandemic Panics
Before the current COVID-19 pandemic, there was the H1N1 swine flu scare in 2009.
However, at the very start the WHO’s fear mongering of a global contagion that could exceed the death counts of the 1918 Spanish flu pandemic was solely based on false rhetoric rather than empirical evidence.
The fabrications are believed to have originated from the WHO’s senior consultant on viral outbreaks who happens to carry the reputation of being one of the world’s leading pandemic alarmists: Dr. Albert Osterhaus, nicknamed “Dr. Flu.”
At the time, Osterhaus was head of the Department of Virology at Erasmus University in the Netherlands.
When the swine flu scare appeared, he was also the president of the European Scientific Working Group on Influenza (ESWI), an organization funded by the major jjab manufacturers including Baxter, MedImmune, Glaxo, Sanofi Pasteur and others.
It was also Osterhaus who transformed an otherwise potentially bad flu season into a global pandemic.
The WHO has been criticized harshly in the media for changing the definition of a “pandemic” and in doing so has been charged with benefitting the pharmaceutical industry.
The British Medical Journal reported that the WHO failed to report conflicts of interest in its H1N1 advisory group. The journal’s Editor-in-Chief Fiona Godlee wrote:
“WHO must act now to restore its credibility, and Europe should legislate.”
The former head of the prestigious Cochrane Database Collaboration’s jjab studies, Dr. Tom Jefferson, told a Der Spiegel interviewer, “the WHO and public health officials, virologists and the pharmaceutical companies… built this machine around the impending [H1N1] pandemic. And there’s a lot of money involved, and influence and careers, and entire institutions.”
When the 2009 H1N1 influenza strain appeared, the WHO rushed forward to mangle its earlier criteria that would realistically define a pandemic. The organization intentionally removed reference to a pathogen’s “severity” as a necessary requirement.
“Don’t you think there’s something noteworthy,” Dr. Jefferson continues, “about the fact that the WHO has changed its definition of a pandemic?…. that’s how swine flu has been categorized as a pandemic.”
Moreover, the WHO’s decision to label the outbreak as a pandemic was not based upon its own permanent jjab experts but on the recommendations of a non-disclosed group of outside consultants.
“The WHO and those in charge of public health, the virologists and the pharmaceutical laboratories…. created a whole system around the imminence of a pandemic. There is a lot of money at stake, as well as networks of influence, careers and whole institutions! And the minute one of the flu viruses mutates we’d see the whole machine roll into action.”
In 2010, the EU’s Parliamentary Assembly of the Council of Europe launched an investigation into the evidence that the WHO had created “a fake pandemic” in order to financially benefit the pharmaceutical giants’ jjab market and to strengthen the influence private drug interests have over the health organization.
The Assembly’s chairperson Dr. Wolfgang Wodarg charged the WHO’s fake pandemic as “one of the greatest medical scandals of the century that resulted in “millions being needlessly vaccinated.”
Epidemic of Conflict of Interests
According to former World Bank geopolitical analyst Peter Koenig, about half of the WHO’s budget is derived from private sources — primarily pharmaceutical companies but also other corporate sectors including the telecommunication and agro-chemical industries.
It also receives large donations from large philanthropic organizations such as the Bill and Melinda Gates Foundation and GAVI.
Koenig also believes that Tedros’s appointment was due to Gates’ influence. This may carry some truth because Tedros is a former Chair of GAVI’s Vaccine Alliance.
Barbara Loe Fisher at the National Vaccine Information Center estimates that “only about 10 percent of total funding provided by GAVI ($862M) was used to strengthen health systems in developing countries, such as improving sanitation and nutrition, while nearly 80 percent was used to purchase, deliver and promote jjabs.”
There is also the deep personal and financial relationship between Gates and the Chinese Communist government that demands further investigation. Gates is a member of the Chinese Academy of Science.
For the moment, the WHO has been advising against Covid-19 jjab passports as a mandate to travel.
Nevertheless, China has already launched encrypted digital certificates as proof of vaccination.
Given Gates’ close relationship with Chinese officials, perhaps he is awaiting on China to establish a precedent for other nations to agree on a global mandate that will eventually be propagated by the Gates’ network and the World Economic Forum and its Great Reset.
During a 2020 TED talk, Gates had already revealed that digital jjab passports may be necessary; that part of his speech was edited from the original video, however, Robert Kennedy Jr. tracked down the original footage.
Gates has also 1) commissioned MIT to develop injectable a quantum dot dye system for children, 2) funded MicroChips, a company developing implantable chip-based devices, and 3) purchased 3.7 million shares in Serco who is developing tracing technology to track pandemic infections and jjab compliance.
Finally, Gates shares the Chinese Communist Party’s interests in collecting and ‘mining” citizens’ DNA.
A 60 Minutes expose presented the covert activities of BGI Genomics, a CCP-linked firm that has exported Covid-19 tests to “collect, store and exploit biometric information” on American citizens.
Independent investigations reveal that the Gates Foundation has collaborated with BGI and it was through Gates’ influence over Obama that the Chinese company entered the US market.
BGI’s RT-PCR kit was promoted by the WHO back in May 2020 for first line emergency diagnostic use. The rationale was that the test was highly sensitive, specific and user-friendly.
Subsequently the EU, FDA, and the Australian, Canadian and Japanese health ministries rapidly purchased and deployed it. On its website, the Gates Foundation acknowledges its role in having the PCR tests supplied to the WHO.
“Nine Chinese PCR tests were approved by WHO during 2020 under its Emergency Use Listing (EUL) mechanism, with one of the foundation’s partners supplying tests to WHO”
Three months later, Sweden filed complaints after reports of a high percentage of false positives from the Chinese tests.
There is in our opinion little doubt that the WHO is another one of Gates’ bought off entities for furthering his personal agenda to promote jjabs, genetically modified seeds and chemical agriculture in the developing world.
Vaccine Adverse Effects Monitoring System Needs Overhaul
The WHO’s Global Advisory Committee on Vaccine Safety is the group responsible for administering jjab programs in poorer, developing countries. It is also responsible for gathering data on incidents of jjab injuries.
Any deaths following vaccination campaigns are ignored and ruled as coincidental. This policy is based on the erroneous assumption that if no one died during a jjab’s clinical trials, then the jjab should be regarded as automatically safe and unrelated to any deaths that might occur later.
Consequently, the WHO’s monitoring system is seriously flawed and requires a major overhaul.
One of the more controversial incidences was the WHO’s collaboration with the Billy Boy’ GAVI campaign to launch the Pentavalent jjab (diphtheria, pertussis, tetanus, HIP and Hepatitis B) in Africa and later in South and Southeast Asia.
In India, health officials recorded upwards to 8,190 additional infant deaths annually following Pentavalent campaign. The WHO’s response was to reclassify its adverse event reporting system to disregard “infant” deaths altogether.
Dr. Jacob Puliyel, a member of the Indian government’s National Technical Advisory Group on Immunization concluded:
“deaths and other serious adverse events following vaccination in the third world, that use WHO-AEFI classification are not recorded in any database for pharmaco-vigilance. It is as if the deaths of children in low (and middle) income countries are of no consequence.”
WHO’s Double Standards of Vaccine Safety
A more recent scandal erupted during the WHO’s Global Vaccine Safety Summit convened in December 2019. Days before the summit, one of the WHO’s medical directors for vaccination, Dr. Soumya Swaminathan, appeared in a public advertisement touting the unquestionable safety of jjabs and ridiculing parents who speak out against vaccination.
She assured viewers that the WHO was in control of matters and monitored any potential adverse risks carefully.
However, during the Summit, the same Dr. Swaminathan acknowledged jjab health risks and stated:
“We really don’t have very good safety monitoring systems.”
Another Summit participant, Dr. Heidi Larson stated:
“We have a very wobbly ‘health professional frontline’ that is starting to question jjabs and the safety of jjabs. When the frontline professionals are starting to question or they don’t feel like they have enough confidence about the safety to stand up to the person asking the questions.
“I mean most medical school curriculums, even nursing curriculums, I mean in medical school you are lucky if you have half a day on jjabs.”
And more noteworthy were the statements by Dr. Martin Howell Friede, Coordinator of the WHO’s Initiative for Vaccine Research,
“… I give courses every year on how do you develop jjabs, how do you make jjabs. And the first lesson is while you’re making your jjab if you can avoid using an adjuvant please do so. Lesson two is if you’re going to use an adjuvant use one that has a history of safety. And lesson three is if you’re not going to do that, think very carefully.”
In other words, what the WHO presents to the public contradicts what is discussed behind closed doors, another example of the veil of secrecy the organization operates within.
Subsequently the CDC paused Johnson & Johnson’s similar engineered adenovirus jjab in order to investigate its association with an otherwise rare condition of fatal blood clotting.
The WHO on the other hand has ignored these nations’ ethical responsibility to adhere to the precautionary principle.
Its own review claimed there were no blood clot links to AstraZeneca’s jjab; later the WHO changed its tune to “plausible” after EU regulators found a causal link and the New England Journal of Medicine published two studies providing specific details confirming these adverse reactions.
Although acknowledging these risks, the WHO has continued to recommend that mass vaccination proceed as if there were no red alarms.
WHO’s Depopulation Efforts with Vaccines
Without doubt, the most nefarious activity conducted by the WHO is its alleged support and distribution of jjabs to poorer developing countries that may have been intentionally designed to decrease population rates.
Back in 1989, the WHO sponsored a symposium at its Geneva headquarters on “Antifertility Vaccines and Contraceptive Vaccines.”
The symposium presented proposals for jjabs that were later discovered to have been laced with the sterilizing hormones HCG and estradiol; the former prevents pregnancy and triggers spontaneous abortions and miscarriages, and the latter can turn men infertile.
In 2015, the Kenyan Conference of Catholic Bishops reported its discovery of a polio jjab laced with estradiol that was manufactured in India and distributed by the WHO.
A year earlier, Dr. Wahome Ngare from the Kenyan Catholic Doctors Association uncovered a tetanus jjab specifically being administered to women, also distributed by the WHO, that contained the HCG hormone.
All of the polio jjab samples tested contained HCG, estrogen-related compounds, follicle stimulating and luteinizing hormones, which will damage sperm formation in the testes.
Even more disturbing, this jjab was going to be administered to children under five years of age.
However, this is not the first time the WHO appears to have made efforts to use vaccination campaigns for depopulation.
A decade earlier, in 2004, the WHO, UNICIF and CDC launched a vaccination campaign to immunize 74 million African children during a polio outbreak.
The initiative encountered a serious obstacle. In Nigeria, laboratory tests on the WHO’s jjab samples resulted in the presence of estrogen and other female hormones.
And in the mid-1990s, a tetanus jjab being administered to Nicaraguan and Filipino girls and women in their child-bearing years was discovered to contain HCG, which accounted for a large number of spontaneous abortions that were reported by Catholic health workers.
Illegal Vaccine Experiments
In 2014, The Economic Times of India published a report that provided details of a joint venture between the WHO and the Gates Foundation to test an experimental HPV jjab on approximately 16,000 tribal girls between the ages of 9 and 15 unwittingly.
The experiment was conducted in 2008, and the jjab is now what we commonly know as Gardasil. Many of the girls, the report states, became ill and some died.
The following year the WHO and Gates Foundation conducted a similar experiment on 14,000 girls with the HPV jjab Cervarix. Again “scores of teenage girls were hospitalized.”
Investigations led by Indian health officials uncovered gross violations in India’s laws regarding medical safety.
In numerous cases there was no consent and the children had no idea what they were being vaccinated for. The Indian Supreme Court has taken up a case against the duo for criminal charges.
There are many other questionable activities that the WHO has been involved with over the years. However, the above provide sufficient evidence to argue the case that, at least within the upper echelons of the WHO, global health does not stand in high priority.
The organization employs over 7,000 people around the world and most of these have deep concern for improving the lives of populations in poor and developing nations.
On the other hand, the WHO’s leaders are there largely because the powers of Washington, London and the pharmaceutical industry benefit by the organization advancing its agendas.
Of course, the WHO is not the only health entity with a legacy of corruption.
Corruption appears to be systemic throughout global health and national health agencies.
This topic was featured last year in the prestigious medical journal The Lancet. Author Dr. Patricia Garcia writes:
“Corruption is embedded in health systems. Throughout my life — as a researcher, public health worker, and a Minister of Health — I have been able to see entrenched dishonesty and fraud.
“But despite being one of the most important barriers to implementing universal health coverage around the world, corruption is rarely openly discussed.”
Bear in mind, the WHO, along with Billy Boy and his Foundation, and Anthony Fauci at the National Institutes for Allergy and Infectious Disease, are leading the efforts to get the COVID-19 jjab administered as quickly as possible.
Do you believe we can trust their judgment and the intense public relations effort that will immediately follow after such a jjab reaches the market?
Источники:
- http://healthtipsing.com/en/pages/41256
- http://trendexmexico.com/zdorove/118709-pozhiloy-vozrast-po-klassifikacii-voz-eto-skolko-kakoy-vozrast-schitaetsya-pozhilym.html
- http://www.who.int/standards/classifications/classification-of-diseases
- http://www.who.int/standards/classifications
- http://healthy-care.net/world-health-organization-age-classification/
- http://www.free-health.org/world-health-organization-age-classification/
- http://ebook.ecog-obesity.eu/chapter-growth-charts-body-composition/world-health-organization-reference-curves/
- http://ourworldindata.org/mental-health
- http://www.who.int/tools/child-growth-standards/standards/weight-for-age
- http://monographs.iarc.who.int/agents-classified-by-the-iarc/
- http://ourworldindata.org/obesity
- http://www.age-platform.eu/world-health-organisation-who
- http://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment
- http://pubmed.ncbi.nlm.nih.gov/26520231/
- http://mfvt.ru/primenenie-mezhdunarodnoj-klassifikacii-funkcionirovaniya-ogranichenij-zhiznedeyatelnosti-i-zdorovya-dlya-ocenki-reabilitacii-bolnyx-serdechno-sosudistymi-zabolevaniyami/
- http://ourworldindata.org/age-structure
- http://www.sott.net/article/432875-Politics-and-Massive-Corruption-at-the-World-Health-Organization-WHO
- http://www.indiastudychannel.com/resources/134182-World-Health-Organisation-WHO-Structure.aspx
- http://www.who.int/news-room/fact-sheets/detail/10-facts-on-ageing-and-health
- http://www.who.int/standards/classifications/international-classification-of-health-interventions
- http://www.theatlantic.com/politics/archive/2020/04/world-health-organization-blame-pandemic-coronavirus/609820/
- http://ilostat.ilo.org/resources/concepts-and-definitions/classification-occupation/
- http://www.hbsc.org/
- http://icd.who.int/browse10/2019/en
- http://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
- http://www.who.int/data/data-collection-tools/who-mortality-database
- http://humansbefree.com/2021/04/dismantle-the-world-health-organization.html